A Device for Quantitative Analysis of
the Thumb Ulnar Collateral Ligament
The MIT Faculty has made this article openly available.
Please share
how this access benefits you. Your story matters.
Citation
Cervantes, Thomas, Woojeong Elena Byun, Ava Chen, Kristina Kim,
Kaitlyn Nealon, Jay Connor, and Alexander Slocum. “A Device for
Quantitative Analysis of the Thumb Ulnar Collateral Ligament.”
2018 Design of Medical Devices Conference 9-12 April 9, 2018,
Minneapolis, Minnesota, USA, ASME, 2018.
As Published
http://dx.doi.org/10.1115/DMD2018-6868
Publisher
American Society of Mechanical Engineers
Version
Final published version
Citable link
http://hdl.handle.net/1721.1/121125
Terms of Use
Article is made available in accordance with the publisher's
policy and may be subject to US copyright law. Please refer to the
publisher's site for terms of use.
A DEVICE FOR QUANTITATIVE ANALYSIS OF THE THUMB ULNAR COLLATERAL
LIGAMENT
Thomas Cervantes
Department of Mechanical Engineering, Massachusetts Institute of Technology,
Cambridge, MA, USA
Stanford University School of Medicine, Stanford, CA, USA
Woojeong Elena Byun
Department of Mechanical Engineering, Massachusetts Institute of
Technology, Cambridge, MA, USA
Ava Chen
Department of Mechanical Engineering, Massachusetts Institute of
Technology, Cambridge, MA, USA
Kristina Kim
Department of Mechanical Engineering, Massachusetts Institute of
Technology, Cambridge, MA, USA
Kaitlyn Nealon
Department of Mechanical Engineering, Massachusetts Institute of
Technology, Cambridge, MA, USA
Jay Connor
Mount Auburn Hospital, Cambridge, MA, USA
Alexander Slocum
Department of Mechanical Engineering, Massachusetts Institute of
Technology, Cambridge, MA, USA
BACKGROUND
A device to quantitatively assess the ulnar collateral ligament of the thumb was developed to facilitate rapid and accurate diagnosis of the ligamentous injury known as Skier’s thumb.
Skier’s thumb is a partial or complete tear of the ulnar collateral ligament (UCL), which connects the first metacarpal to the proximal phalanx of the thumb. This injury commonly occurs when falling while grasping an object (such as a ski pole), and has a yearly incidence of ~200,000 [1]. The UCL plays a key role in the ability to grip objects; patients suffering from Skier’s thumb are often forced to take a leave of absence from work until the injury is healed. Timely, accurate diagnosis is essential for patients to receive proper treatment and regain functionality of their hand.
The treatment of skier’s thumb is a function of UCL tear severity and falls within two categories of treatments: partial UCL tears can be left to heal on their own with cast stabilization, while full tears require surgical intervention to
ensure full recovery [1]. The optimal window for surgical repair is within two weeks of the initial injury [2].
Initial diagnosis occurs through physical exam of the thumb metacarpo-phalangeal (MCP) joint. The physician performs a stress test to analyze the integrity of the UCL ligament. The metacarpal is held fixed in space while the thumb is moved laterally by the examiner. The metrics of the stress test are 1) maximum angular deflection of the thumb, and 2) assessment of endpoint stability at maximum deflection. A “soft” endpoint, with maximum deflection greater than 30-35 degrees, is indicative of a full UCL tear. A “firm” endpoint, with smaller angular deflection, is considered partially torn [3]. The injured thumb is typically compared against the healthy thumb to account for normal variations in joint flexibility [4].
The initial stress-test is a primarily qualitative assessment and relies heavily on the experience of the examiner to accurately diagnose the degree of injury. Because the difference in treatment options for full vs partial tear is so drastic (surgery vs cast), patients are often referred for further imaging studies to confirm the diagnosis. MRI is the gold standard for
Proceedings of the 2018 Design of Medical Devices Conference DMD2018 April 9-12, 2018, Minneapolis, MN, USA
UCL secondary diagnosis [3]. However, MRI can add significant cost to the patient’s treatment, and can also push surgery outside of the optimal treatment window of two weeks. Diagnosis and treatment of Skier’s thumb injuries could be improved through precise, quantitative assessment of the UCL at the time of initial examination. A reliable method for performing this assessment has the potential to reduce the costs of care and improve surgical outcomes by precluding the need for MRI as a secondary diagnostic tool.
METHODS
A device to quantitatively assess the thumb UCL was developed using a deterministic design process. The following functional requirements were identified:
1) Measure parameters that directly correspond to UCL integrity
2) Examiner-independent performance
3) Stabilize metacarpal to isolate MCP abduction in the coronal plane
4) Accommodates a wide range of bilateral thumb sizes 5) User-friendly operation
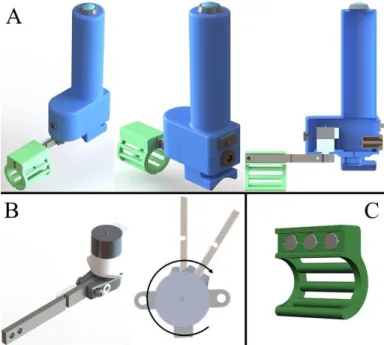
6) Safe operation through emergency stop functionality The final device design (Fig. 1A) is a motorized, hand-held device that rotates the thumb radially and measures the applied torque. The primary functional module is a stepper motor that is coupled to a cantilevered load cell (Fig. 1B). The load cell interfaces with the patient’s thumb through a magnetically-attached cradle (Fig. 1C) designed to accommodate up to the 99th percentile male thumb dimensions
[5]. When the motor turns, the load cell is rotated about the MCP joint, and a torque is applied to the ulnar side of the thumb via the thumb cradle.
The cradle is also designed as a safety countermeasure, and will magnetically break-away once a 10N force threshold is reached. The device is positioned on the hand through a V-shaped cradle over the 1st metacarpal. Angular displacement is
calculated by counting the number of steps taken by the motor. Torque applied to the thumb is measured using the strain gauge and an on-board instrument amplifier. These measurements of angular displacement and torque are transmitted wirelessly via Bluetooth to a computer or phone. Right hand vs left hand operation can be selected via a switch on the back of the device.
To conduct testing of the thumb, the physician positions the device such that the axis of rotation is aligned with the MCP joint, and the load cell is aligned with the long axis of the thumb (Fig. 2). Movement is initiated by holding the button at the top of the vertical handle. If the button is released, the device immediately stops. The device slowly rotates the thumb at ~2 degrees/sec while continuously taking measurements from the load cell. Testing is terminated once user-defined torque & displacement limits are exceeded.
Figure 1: (A) CAD models of the thumb UCL testing device. (B) Stepper motor coupled to the cantilever load cell. As the motor rotates, the load cell measures the torque applied to the thumb. (C) Thumb cradle with magnetic attachments.
Figure 2: Final built prototype of the thumb UCL testing device being used to test a thumb. When the motor turns, the thumb is moved in the direction of the arrow, thereby generating a torque on the MCP joint.
RESULTS
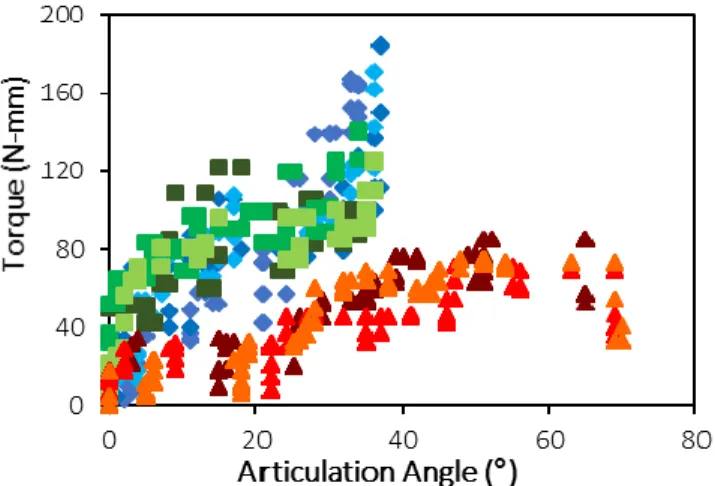
Quantitative testing of the device was performed using a series of thumb models designed to mimic the articulation of the MCP joint. Extension springs with different spring constants were incorporated in the joint to simulate UCL tears of differing severity. Each thumb model was affixed to the device using the metacarpal and thumb cradles. Testing was performed for simulated full and partial UCL tears, as well as a simulated intact ligament. Results are shown below in Fig. 3. There is a clear distinction between the torque-angle curves of the fully torn UCL model, compared to the curves of the intact and partially torn UCL models.
Figure 3: Torque vs articulation angle plot of thumb model tests. Squares = intact UCL, Diamonds = partially torn UCL, Triangles = full tear of UCL
Additional testing was conducted on healthy human subjects to determine a range of normal MCP joint stiffness. Eight subjects were tested (6 male, 2 female, age 21-52 years), with two testing trials performed on each hand. Figure 4 shows a representative plot of torque and stiffness vs angular displacement for a single subject’s hand. Peak thumb torque measured for all subject was 213.5 ± 19.2 N-mm; peak MCP joint stiffness was 4.70 ± 0.39 N-mm/degree. A sharp increase in torque and stiffness is noted around 35-40o, and likely
represents “engagement” of the UCL ligament.
INTERPRETATION
A device was created to quantitatively assess the integrity of the thumb UCL through measurement of applied torque and angular displacement. These measurements correspond to the parameters currently used in the clinical stress-test, namely the “soft vs hard” endpoint. Preliminary testing on thumb models showed that full tears of the UCL can be readily distinguished from partially torn and intact ligaments. Preliminary testing on healthy thumbs showed peak torque and stiffness
measurements to be on the order of 213.5 mm and 4.70 N-mm/deg, respectively.
Future iterations of the device are focused on improving the precision of torque measurements from the load cell, and creating a real-time visual display of the data as it is being collected. Further healthy human subject testing is needed to establish a range of normal values for thumb MCP stiffness. Cadaver testing will be conducted to characterize device performance while imposing UCL tears of known severity, followed by testing of patients with suspected Skier’s thumb injury.
Figure 4: Representative plots of torque (triangles, bottom) and stiffness (circles, top) vs articulation angle plot of a healthy test subject.
ACKNOWLEDGMENTS
The authors would like to acknowledge the students, faculty, and staff from the Medical Device Design class at MIT (2.75). Human subject testing was performed with approval from the MIT Committee On the Use of Humans as Experimental Subjects (protocol # 1710122344).
REFERENCES
[1] Mahajan, M. and Rhemrev SJ, 2013, “Rupture of the ulnar collateral ligament of the thumb – a review,” Int. Journal of Emergency Medicine, 6 (31). doi:10.1186/1865-1380-6-31.
[2] Ritting, A.W., Baldwin, P.C., and Rodner, C.M., 2010, “Ulnar collateral ligament injury of the thumb metacarpophalangeal joint,” Clin J Sport Med, 20(2), pp. 106-12. doi: 10.1097/JSM.0b013e3181d23710
[3] Arende, C.F. and da Silva, T.R., 2014, “The role of US in the evaluation of clinically suspected ulnar collateral ligament injuries of the thumb: spectrum of findings and
differential diagnosis,” Acta Radiologica. 55(7), pp. 814-23. doi: 10.1177/0284185113506139
[4] Chuter, G.S., Muwanga, C.L., and Irwin, L.R., 2009, “Ulnar collateral ligament injuries of the thumb: 10 years of surgical experience,” Injury, 40(6), pp. 652-6. doi: 10.1016/j.injury.2009.01.107
[5] Tilley, Alvin, 2002, The Measure of Man & Woman. Wiley, New York. Print