ArchivesofCardiovascularDisease(2019)112,430—440
Availableonlineat
ScienceDirect
www.sciencedirect.com
REVIEW
Pathophysiology
and
management
of
combined
aortic
and
mitral
regurgitation
Physiopathologie
et
prise
en
charge
des
insuffisances
valvulaires
aortiques
et
mitrales
combinées
Philippe
Unger
a,∗,
Patrizio
Lancellotti
b,c,
Mihaela
Amzulescu
a,
Aurelia
David-Cojocariu
a,
Didier
de
Cannière
daDepartmentofCardiology,CHUSaint-Pierre,UniversitéLibredeBruxelles,1000Brussels,
Belgium
bDepartmentofCardiology,HeartValveClinic,GIGACardiovascularSciences,Universityof
LiègeHospital,CHUSartTilman,4000Liège,Belgium
cGruppoVillaMariaCareandResearch,AntheaHospital,70124Bari,Italy
dDepartmentofSurgery,CHUSaint-Pierre,UniversitéLibredeBruxelles,1000Brussels,
Belgium
Received19March2019;receivedinrevisedform7April2019;accepted15April2019 Availableonline29May2019
KEYWORDS Aorticregurgitation; Mitralregurgitation; Multiplevalve disease;
Heartvalveteam
Summary Thecombinationofaorticandmitralregurgitationisatypicalexampleofa
fre-quentyetunderstudiedmultiplevalvedisease scenario.Theaetiologyisoftenrheumaticor
degenerative; less frequently itcan be induced by drugs or radiation, orcaused by
infec-tive endocarditis or congenital valvular lesions. Aortic regurgitation resulting in secondary
mitralregurgitationisalsonotuncommon. Therearelimiteddatatoguidethemanagement
ofcombinedaorticandmitralregurgitation.Leftventriculardysfunctionisfrequentatinitial
presentation,andevenmoresopostoperatively,suggestingthatsurgicalmanagementshould
notbedelayed,particularlywhensymptomsoccurorwhenthereisevidenceofevensubtle
leftventriculardysfunction.Thedecisiontooperateononeorbothvalvesnotonlydepends
ontheseverityofeachlesion,butalsoonseveralotherfactors,includingage,co-morbidities
andfrailty,theincreasedoperativeriskofdoublevalvesurgery,theincreasedriskoflong-term
Abbreviations: AHA/ACC, American Heart Association/American College of Cardiology; AR, aortic regurgitation; LV, left ventri-cle/ventricular;MR,mitralregurgitation.
∗Correspondingauthorat:DepartmentofCardiology,CHUSaint-Pierre,322rueHaute,1000Brussels,Belgium.
E-mailaddress:punger@ulb.ac.be(P.Unger). https://doi.org/10.1016/j.acvd.2019.04.003
thromboticandbleedingcomplicationswithmultiplemechanicalvalves,theriskofleavingone
valveunoperatedandtheprobabilityofrequiringredosurgery.Theroleofamultidisciplinary
heartvalveteamiscriticalinthissettingtooptimizemanagementandoutcomes.Theroleof
transcatheterapproachesiscurrentlylimited,buttechnologicaladvanceswillprobablysoon
changethemanagementparadigm.
©2019ElsevierMassonSAS.Allrightsreserved.
MOTSCLÉS Insuffisance aortique; Insuffisancemitrale; Cardiopathies valvulaires; Affectionsvalvulaires multiples
Résumé L’associationd’unerégurgitationvalvulaireaortiqueàunerégurgitationmitraleest
unexempletypiqued’affectionplurivalvulaire,fréquenteetcependantpeuétudiée.Les
éti-ologiesrhumatismalesetdégénérativessontlespluscourantes;l’endocarditeinfectieuse,les
atteintesvalvulairesmédicamenteusesetradiques,ainsiquelesvalvulopathiescongénitales
devrontaussiêtre recherchées.L’insuffisance aortiqueavec insuffisancemitrale secondaire
estaussiunesituationfréquente.Lapriseenchargedespatientsdecespatientsn’aétéque
peuétudiée.Ladysfonctionsystoliqueventriculaire,fréquentelorsdudiagnostic,l’estencore
plus enpostopératoire, plaidant pourune priseencharge chirurgicale précoce, etce, dès
l’apparitiondesymptômesoudesignes>mêmediscretsdedysfonctionventriculaire.La
déci-siondetraiterlesdeuxvalvesd’embléeouden’enopérerqu’une dépendranonseulement
delasévéritédechacunedesrégurgitations,maisaussidemultiplesfacteurs,parmilesquels
l’âge,lescomorbiditésetlafragilitédupatient,lerisqueopératoireetdesrisques
hémorrag-iquesetthrombotiquesinhérentsàlachirurgiebivalvulaireetlerisquedelaissertellequ’elle
unevalvedysfonctionnelleetdedevoirl’opérerultérieurement.Uneéquipemultidisciplinaire
spécialiséedanslapriseenchargedesaffectionsvalvulairesseraparticulièrementbénéfique
pourenoptimaliserletraitementetaméliorerlepronosticdupatient.Silaplacedévolueau
traitementpercutanédesaffectionsbivalvulairesrégurgitantesestactuellementlimitée,ilne
faitaucundoutequelesprogrèstechnologiquesmodifierontconsidérablementnotreapproche
thérapeutique.
©2019ElsevierMassonSAS.Tousdroitsr´eserv´es.
Background
The diagnosis ofvalvularheart diseasehas improved con-siderably over recent years, as has its management, but therearestilllimiteddatatoguideclinicaldecisionmaking inpatients withmultiple valvedisease [1—3].Inthis con-text,thecombinationofaorticregurgitation(AR)andmitral regurgitation(MR) is a typical example of a frequent yet understudiedscenario[3].Theaimofthisarticleisto pro-videastate-of-the-artreviewofthepathophysiologyofthis conditionandmanagementstrategies,takingintoaccount itsvariousclinicalpresentations.
Aetiology
and
prevalence
WithareportedprevalenceintheCARDIAstudyof0.5%in subjectsaged21to35years,thecombinationofARandMR isuncommoninyoungadults[4].Amongolderpatientswith amean ageof54 yearsfromtheFraminghamcohort, the prevalence of regurgitation involving twovalves was10% for men and 8% for women, but more than mild MR and morethantraceARwereinfrequent[5].However,Paietal. reportedthat amongpatients with severe AR,up to one-quarteralsohad moderate-to-severeMR [6].Ina Swedish
nationwideregistry includingall hospitals andspecialized outpatient clinics, 10.7% of patients with AR had conco-mitantMR,and 8%of patientswithadiagnosis of MRhad concomitantAR[7].Moreover,22%ofthepatientswith mul-tiplevalvediseasehadacombinationofARandMR,making this the third most frequent form of multiple and mixed valvedisease[7].
In combinedAR and MR, the twoconditions may have a similar aetiology or, less frequently, be the result of twounrelatedprimarydiseaseprocesses.IntheEuroHeart Survey,rheumatic heart disease wasthe leadingcause of multiplevalvedisease (51%of cases)(Fig.1), and degen-erativeaetiologies were responsible for 41% of cases [8]. However,whereastheincidenceofrheumaticheartdisease hasdeclined over thepast few decades, theagingof the population ofindustrialized countries accountsfor a shift towardsdegenerativeaetiologies, without aglobal reduc-tionintheoverallprevalenceofvalvularheartdisease[9]. All other aetiologies, including infective endocardi-tis, drugs, radiation and congenital valvular lesions, are much less frequent. Nonetheless, multiple valve disease is observed in more than 20% of patients with drug- or radiation-inducedheartvalvedisease[10,11].Multiplevalve disease resulting from infective endocarditis carries an increasedriskofheartfailure[12].
432 P.Ungeretal.
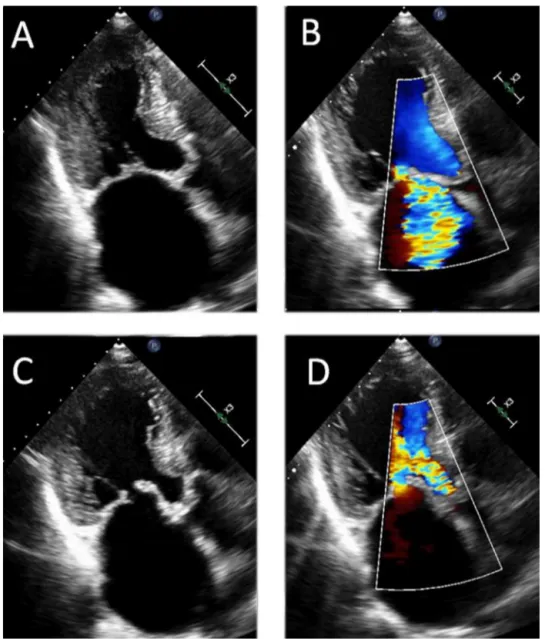
Figure1. Combinedrheumaticaorticandmitralregurgitation.AandB.Systolicstillframes.CandD.Diastolicstillframes.
Varying degrees of MR may result from remodelling, shape distortion and impaired function of the left ven-tricle (LV) associated with severe AR, thereby restricting mitral valve motion [13]. Secondary (functional) MR, in whichthevalveisstructurallynormalandtheleaflet coap-tationdefectmainlyresultsfromventricularand/or atrial remodelling,is common in patients withaortic valve dis-ease;however, moststudies included patients withaortic stenosis, and there are limited data focusingon patients withpredominant AR [13,14]. In a series of 779 patients whohad undergone aortic valve replacement, Lim et al. identified155 patients (20%)withmild-to-moderate func-tional MR, but the number of patients with severe MR was not reported [14]. In a series of 816 patients with AR,Beaudoin etal.reporteda5.6%prevalence of moder-ateorseveresecondaryMR[13].Interestingly,theauthors attributedthis lowprevalence to asignificant increase in mitralvalveleafletareacomparedwithcontrols andwith patientswithfunctional MRof other aetiologies[13]. The mechanism of this valvular remodelling was unclear, but itwaspostulated thatthe increasein mitralvalveleaflet
areamightbeacompensatorymechanism,preventingthe developmentof MR by helpingto preservea normal rela-tionship to the area needed for closure in a dilated LV
[13].
Pathophysiology
Both AR and MR increase left ventricular (LV) preload, whereas only AR has a significant effect on afterload,as a result of the impact of the increased total stroke vol-ume ejected on systemic vascular resistance, and of the resulting systolic hypertension [15]. Therefore, severe LV dilatationmayoccurwhenARandMRarepresenttogether. Inaddition,theresultingcombinationofvolumeand pres-sure load further increaseswall thickness[16]. Thus, the resulting LVhypertrophy will usually beeccentric, with a wallthickness-to-cavityratiotypically<0.45,andincreased sphericity[17].Attheonsetofsymptoms,patientsmayhave a reduced LVejection fraction, which can beeven worse thanthatassociatedwithisolatedARorMR[17,18](Fig.2).
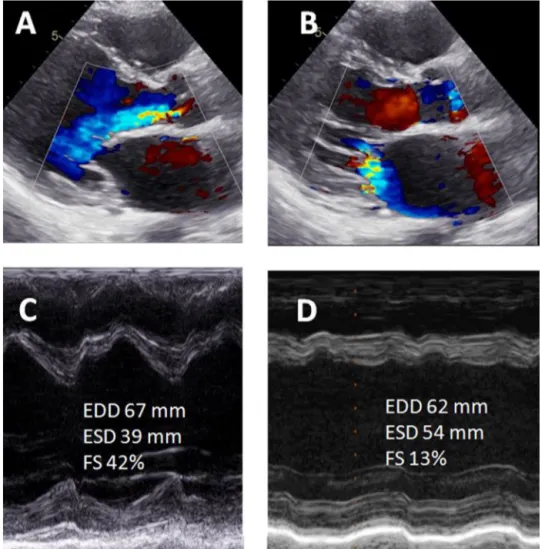
Figure2. A.Severemitralregurgitation.B.Severeaorticregurgitation.Leftventricularejectionfractionis35%(notshown).CandD. ShortdP/dt(618ms;C)andmarkedreductioningloballongitudinalstrain(—6.4%;D)areconsistentwithsevereleftventriculardysfunction.
When acuteand severeAR developsin patients with pre-existingMR,themarkedincreaseinLVend-diastolicpressure maybetransmittedbackwards,asprematuremitralvalve closure no longer limits the amount of flow into the left atrium and pulmonary veins(Fig. 3). The combination of ARandMRpredisposestoatrialfibrillationandpulmonary hypertension. As a result of chronic volume and pressure overload,MRisanindependentriskfactorforreduced sur-vivalinpatients withsevere AR,withmortalityincreasing witheachgradeofMRseverity[6].
Diagnosis
The proximal isovelocity surface area (PISA) method and the assessment of vena contractafor quantifying regurgi-tant lesions are lesser load-dependent methods that can beuseful in thissetting. Bycontrast,volumetricmethods of assessing the severity of MR and AR can be chal-lenging, because left-sided assessment of forward flow is invalid. However, the right ventricular outflow tract can
beused as an alternative to assess the net forward flow
[3,19].Thepressurehalf-timecanbeinaccuratein
assess-ing the severity of AR, and the mitral-to-aortic velocity timeintegral ratio is inherently unreliable. Cardiac mag-neticresonanceimagingmaybeusedtoquantifyregurgitant lesions, particularly when the echocardiographic image qualityis inadequate or when echocardiographyvariables arediscordant withclinical assessment [19,20]. However, volumetricmethodscanalsobeinaccurateinthepresence of multiple regurgitant lesions, asthese methods assume that only one valve is affected [21]. Cardiac magnetic resonanceimagingmayaccuratelyquantifychangesin ven-tricularvolumes,massandfunctionand,hence,byassessing the global burden of the valve regurgitations, may con-tributetodeterminingtheoptimaltiming forintervention
[20].
Nostudyhasevaluatedthevalueofglobal longitudinal straininthespecificsettingofmultiplevalvedisease. How-ever,itsrolehasbeenconsistentlyhighlightedinisolatedAR
andMR[22,23]and,consequently,itmightberecommended
434 P.Ungeretal.
Figure3. Acuteaorticregurgitation(AR)asaresultofinfectiveendocarditis.A.Parasternallong-axisviewshowingconcomitantAR(yellow arrows)andmitralregurgitation(MR)(whitearrows)duringend-diastole.B.Thepressurehalf-timeoftheARjetis108ms,consistentwith severeAR.CandD.ColourDopplerandcolourM-modeobtainedinthe140◦planebytransoesophagealechocardiography,confirmingthe occurrenceofdiastolicMR.DiastolicMR resultsfrom increasedleftventriculardiastolicpressure,andreflects prematuremitralvalve closure.LA:leftatrium;LV:leftventricle.
Management
Most published results of double valve replacement for combined AR and MR come from studies focusing on youngpatients,predominantlywithrheumaticheartdisease aetiology[17,18,22,24].Whetherolderpatientswith degen-erativevalvedisease,andthus alongerhistoryofvalvular regurgitationanda lowerlifeexpectancy, wouldsimilarly benefitfromextensivesurgeryislargelyspeculative.In gen-eral,thedecisiontooperateononeorbothvalvesdepends on the severity of each lesion, but other factors should also be taken into account. The increased operative risk of double valvesurgery [25,26] and the increased risk of long-termthromboticandbleedingcomplicationswith mul-tiplemechanicalvalves[27]shouldbebalancedagainstthe probabilityof requiring redo surgery and itsinherent risk ifonlyonevalveisreplaced.This decisionmusttherefore takeintoaccountmanyfactors,includingpatientage, co-morbiditiesandfrailty[28].Inaddition,expertiseincardiac imaging,cardiacsurgery,haemodynamicmanagement, geri-atricsandanaesthesia,inthesettingofamultidisciplinary heart valve team, is required to optimize management
[28].
Effects
of
aortic
valve
replacement
on
the
severity
of
MR
LVfunction,mass andvolumesfrequentlyimprove follow-ingaorticvalvereplacementinpatientsundergoingsurgery for severe AR, witha variabletime-courseresponse [29]. Thus,whenconcomitantfunctionalMRismildtomoderate, aortic valvesurgeryfor severe ARis expectedtoimprove MR (Fig. 4). In a study by Lim etal., an improvement in MRseveritywasobservedin88%ofpatients,evenwithout concomitantmitralvalveannuloplasty,andwasparalleled byareductioninLVend-diastolicdimension[14].However, whethercorrectionofthevolumeoverloadbyaorticvalve replacement is sufficient to managesevere secondary MR hasnotyetbeenestablished.
Effects
of
double
valve
surgery
on
LV
volume
and
function
As a result of specific loading conditions, LV function frequentlydecreasesaftermitralvalvereplacementfor iso-latedMR,therebyprecludingmitralvalvesurgeryinpatients withsevereLVdysfunction.Bycontrast,LVfunctionusually
Figure4. Severeaorticregurgitation.A.Usingtransoesophagealechocardiography,thereisalargevenacontracta,consistentwithsevere aorticregurgitation(whitearrow).B.Thereisconcomitantmoderatesecondarymitralregurgitation,asseenbytransthoracic echocardio-graphy(yellow arrow).C.Aortic valvereplacementwasperformed;ontheseventhpostoperativeday,onlytrace mitralregurgitation remained.Ao:ascendingaorta;LV:leftventricle.
improvesafteraorticvalvereplacementforisolatedAR,so thepresenceofevenaseverelydepressedLVejection frac-tion does not exclude aortic valvereplacement. Whether doublevalvesurgeryfor combinedARandMRimprovesor worsens LVperformance isthus an important issue. Essop et al.compared the effects of double valvereplacement forcombinedAR/MRwiththoseofmitralvalvereplacement for isolatedMR. Asimilarreductioninend-diastolic diam-eter was observed, but, 3 months after surgery, a larger
reduction in end-systolic diameter after double valve surgerywasassociatedwithasmallerdeteriorationin ejec-tionfraction[30]. Thisobservation suggeststhatlevelsof ejectionfractionthatprecludesurgeryforisolatedMRmight stillbeacceptablefordoublevalvereplacementforAR/MR
[30]. However, discrepant results were reported by Gen-tles et al. [17]. In a child and young adult population, the development or persistence of postoperative LV dys-function (definedas a Z-score<—2) occurred significantly
436 P.Ungeretal.
Figure5. A.andB.Diastolicandsystolicparasternallong-axisviewsshowingsevereARandmoderate-to-severeMR,respectively.Cand D.Despitebeingpreservedbeforesurgery(C),fractionalshorteningismarkedlydecreasedfollowingdoublevalvereplacement(D).EDD: end-diastolicdiameter;ESD:end-systolicdiameter;FS:fractionalshortening.
more often after double valvesurgery (84.4%) than after isolated aortic valve replacement for AR (35.7%) or iso-latedmitralvalvereplacementforMR(57.1%)[17](Fig.5). The betterresults from Essopetal. were attributedtoa shorterdurationofvolumeloading,therebyemphasizingthe roleof early surgical management [30].Importantly, Sku-dickyetal.observedthat,despiteinitialdeterioration,LV ejectionfractiontendedtonormalize1yearaftersurgery
[24].Moreover,LVejectionfractionandend-systolic diam-eterwereidentifiedasindependentpredictive factorsfor postoperativesystolicperformance[24].Theprobabilityof havinganejectionfraction<50%afterameanfollowupof 40monthsrosesignificantlywhenthepreoperativeejection fractionwas<60%,and/or whenthe LVend-systolic diam-eterwas>40mm[24].Thereiscurrentlynodefinitelower thresholdthatwouldcontraindicateadoublevalve proce-dure,particularlyifARispredominant.
Surgery
and
prognosis
In a study dating back to the early 1990s, Niles et al. reportedthatpatientswithdoublevalvereplacementhad
significantlyreducedpostoperativesurvival,andmore fre-quently reportedpersistent postoperative symptoms than patients who underwent surgery for single valve disease
[18].More recently,Pai etal.reportedonaseriesof 191 patients withsevereAR andconcomitant grade3—4+ MR. Among them,65 patientsunderwentaortic valve replace-ment, and had significantly better survival than patients whodidnothaveaorticvalvereplacement[6].Importantly, among these patients, 39 had concomitant mitral valve surgery and 26 had only isolated aortic valve surgery. In thislimitedseries,asurvivalbenefitwasobservedonly in the subgroup that had undergone mitral valve repair (17 patients).Similarbenefitsofmitralvalverepairhavebeen observedinretrospectiveseriesthatincludedpatientswho hadsurgery for both ARandMR [31,32],but studieshave also been published in which no benefit of mitral repair over replacement was shown [33,34]. Prospective data addressingthisissuearecurrentlylacking.Combinedaortic and mitralvalve repair has occasionally been attempted, yielding acceptablelong-term survival rates,but withthe drawbackoflimiteddurability,leadingtoa10-year reoper-ationrateof35%[35].
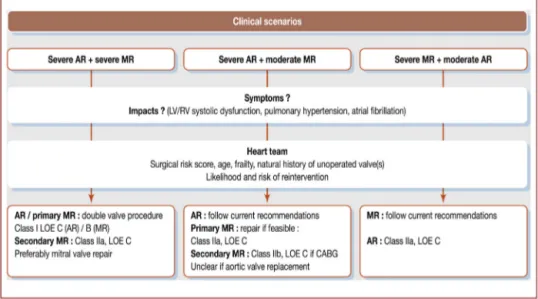
Figure6. Managementstrategyaccordingtotheseverityofaorticregurgitation(AR)andofmitralregurgitation(MR),accordingtothe AmericanHeartAssociation/AmericanCollegeofCardiologyguidelinesforthemanagementofpatientswithvalvularheartdisease[2]. CABG:coronaryarterybypassgrafting;LOE:levelofevidence;LV:leftventricular;RV:rightventricular.
Management
according
to
lesion
severity
Current literature lacks evidence-based management strategies,asemphasized bytheC levelof evidence sup-porting most recommendations in the current guidelines fromEuropeandtheUSA[1,2].Nomedicaltreatment has provedbeneficialforisolatedorcombinedARandMR. How-ever,asisrecommendedinisolatedAR,highbloodpressure shouldbe corrected usingvasodilators, and diuretics may playanimportantroleinreducingcongestionandsymptoms inpatients withcombinedARandMR forwhomsurgeryis notfeasible.Conventionalheartfailuretreatments, includ-ingangiotensin-convertingenzymeinhibitors,beta-blockers andmineralocorticoidreceptorsantagonists,shouldnotbe used in asymptomatic patients without LV dysfunction to avoid delay in symptom onset and, hence, in referral to surgery,butshouldbeconsideredappropriateinpatientsnot consideredforsurgery,orifsymptomsand/orLVdysfunction persistordevelopaftersurgery.
Inclinical practice,thecombination ofARandMR usu-allypresentsasoneofthefollowingscenarios:(1)thetwo regurgitationsaresevere;(2)ARissevereandMRis mod-erate;or(3)MRissevereandARismoderate.Mildlesions needonlywatchfulwaiting.Amanagementstrategyadapted fromcurrentAmericanHeartAssociation/AmericanCollege of Cardiology (AHA/ACC) guidelinesis presented in Fig. 6
[2].
Scenario
1:
The
two
lesions
are
severe
Inthissetting,bothlesionsshouldbetreated.Mitralvalve repairor replacement inpatientswithchronic severe pri-maryMRundergoingaorticvalvereplacementhasreceived aClassIrecommendation(levelof evidenceB),but hasa ClassIIarecommendation(levelofevidenceC)forsecondary MR. Aortic valvereplacement has a Class I recommenda-tion(levelofevidenceC)forpatientswithsevereARwhile undergoingsurgeryforMR.
Scenario
2:
AR
is
severe
and
MR
is
moderate
SevereARshouldbemanaged accordingtocurrent guide-lines. However, whether moderate MR should be treated concomitantly remains controversial. Indeed, no survival benefit has been demonstrated after the surgical treat-ment of moderate secondary MR in prospective studies. MitralvalverepairinpatientswithmoderatesecondaryMR undergoingcoronaryarterybypasssurgerythereforehasa ClassIIbrecommendation(level ofevidence C)in current AHA/ACCguidelines.Moreover,thelikelihoodofMR improv-ingfollowing aorticvalvereplacementishigh,makingthe need totreat MR in this setting evenmore questionable. Despitethelackofarandomizedcomparisonbetweenvalve replacement andrepair, it is widely accepted that, when feasible,valverepairisthepreferredtreatmentfor moder-ateprimaryMR.Therefore,concomitantmitralvalverepair isconsideredreasonableinpatientswithchronicmoderate primaryMRundergoingcardiacsurgeryforotherindications (ClassIIa,levelofevidenceC).
Scenario
3:
MR
is
severe
and
AR
is
moderate
SevereMRshouldbemanagedaccordingtocurrent guide-lines.Correctingmoderate ARat thetimeof mitralvalve surgeryisconsideredasreasonable intheAHA/ACC guide-lines (Class IIa, level of evidence C), because of the likelihoodofprogressiveworseningofARovertime.
Occasionally, twomoderate lesions mayhave deleteri-ousclinicalrepercussions,includingsymptoms,LVdilatation with or without dysfunction, reduction in net forward flow,increased natriuretic peptide concentrations and/or impairedexercisetolerancewithmaximaloxygen consump-tion(Fig.7). To the bestof our knowledge, nostudy has assessed the impactof combinedmoderate ARand mod-erate MR, and this scenario is not addressed in current guidelines. Nevertheless, such patients should undergo a thorough assessment of the global repercussions of the tworegurgitantlesions. Ifthe results are consistent with
438 P.Ungeretal.
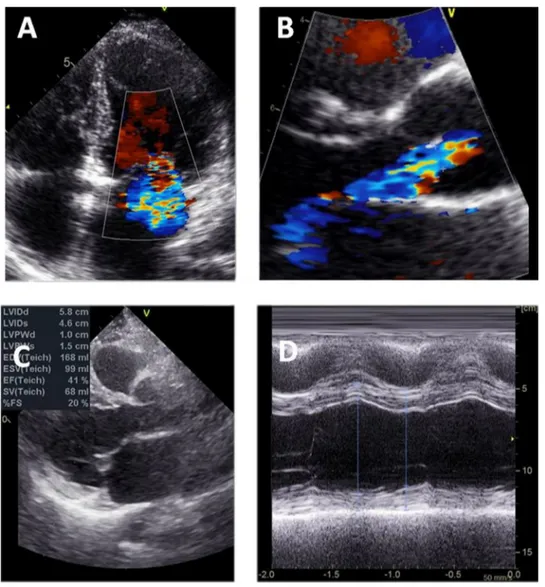
Figure7. AandB.Rheumaticheartdisease,includingmoderatemitralregurgitation(mitraleffectiveregurgitantorifice0.25cm2;A)
andmoderateaorticregurgitation(venacontracta5mm;B).CandD.Althougheachlesionisseparatelyconsideredmoderate,theleft ventricleismildlydilated(end-diastolicdiameter58mm),consistentwithasignificantglobalimpactofthetworegurgitations.
asignificant globalhaemodynamic impact, valverepair or replacementmightbeconsidered,butthisstrategyrequires carefulexclusionofconfoundingfactors,includingchronic lungdiseaseandprimaryventriculardysfunction.
Themanagementofasymptomaticpatientsinthesetting of combined AR and MR also lacks evidence-based sup-port.Ifthetwolesionsaresevere,the stricterthresholds of MR should be used to indicate surgery, including a LV end-systolic diameter≥40mm and/or a LV ejection
frac-tion<60%[1,24].IfMRorARispredominant,therespective
thresholdsin current guidelines shouldbeused [1,2],but evensubtleevidenceforLVdysfunction,includingreduced globallongitudinalstrain,mightbeconsideredasan incen-tiveforearliersurgery.Asmentionedabove,anassessment of the global repercussion should be strongly considered, including exercise testing to detect pseudoasymptomatic patients.
Role
of
transcatheter
interventions
Percutaneousrepair ofMRhas beenshown tobesafeand efficacious[36]. Although ithas notyet become standard
practice,thereisrecentevidencethattranscatheteraortic valvereplacementmaybefeasibleinpatientsathigh sur-gicalrisk withnativevalveAR[37].However,theuseofa fullytranscatheterapproachforthetwoconditionsremains exceptional.Inarecentliteraturereview,Andoetal. iden-tified37 studiesincluding60patients consideredtobeat high or inoperable surgical risk who had combined tran-scatheteraorticandmitralvalveintervention.Amongthese, fourpatients(7%)hadbothARandMR,threeofwhomhad undergoneatleastonevalve-in-valveprocedure.Onlyone patient had a fully transcatheter approach performed on nativevalves[38,39].
Conclusions
There arelimiteddatatoguide themanagementof com-bined AR and MR. LV dysfunction is frequent at initial presentationandpostoperativeLVdysfunctioniscommon, suggestingthatsurgicalmanagementshouldnotbedelayed, particularlywhensymptomsoccurorwhenthereisevidence of LV dysfunction. As with other combined valve disease
combinations,all decisionsshouldbemadeby a multidis-ciplinaryheartteaminordertooptimizepatientoutcomes. The roleof transcatheterapproaches iscurrently limited, but technologicaladvanceswill probablysoon change the managementparadigm.
Disclosure
of
interest
Theauthorsdeclarethattheyhavenocompetinginterest.
References
[1]BaumgartnerH,FalkV,BaxJJ,etal.2017ESC/EACTS Guide-linesforthemanagementofvalvularheartdisease.EurHeart J2017;38:2739—91.
[2]Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC focusedupdateofthe2014AHA/ACCguidelineforthe mana-gementof patientswithvalvularheartdisease: a reportof theAmerican College ofCardiology/American Heart Associ-ation TaskForce on clinicalpractice guidelines. Circulation 2017;135:e1159—95.
[3]UngerP,PibarotP,TribouilloyC,etal.MultipleandMixed Valvu-larHeartDiseases.CircCardiovascImaging2018;11:e007862. [4]ReidCL,Anton-CulverH,YunisC,GardinJM.Prevalenceand clinicalcorrelatesofisolatedmitral,isolatedaortic regurgita-tion,andbothinadultsaged21to35years(fromtheCARDIA study).AmJCardiol2007;99:830—4.
[5]Singh JP, Evans JC, Levy D, et al. Prevalence and clinical determinantsofmitral,tricuspid,andaorticregurgitation(the FraminghamHeartStudy).AmJCardiol1999;83:897—902. [6]PaiRG,VaradarajanP.Prognosticimplicationsofmitral
regurgi-tationinpatientswithsevereaorticregurgitation.Circulation 2010;122:S43—7.
[7]AndellP,Li X,MartinssonA, etal. Epidemiologyofvalvular heartdiseaseinaSwedishnationwidehospital-basedregister study.Heart2017;103:1696—703.
[8]IungB,BaronG,TornosP,Gohlke-BarwolfC,ButchartEG, Vaha-nianA.Valvularheartdiseaseinthecommunity:aEuropean experience.CurrProblCardiol2007;32:609—61.
[9]Goldbarg SH, Elmariah S, Miller MA, Fuster V. Insights into degenerative aortic valve disease. J Am Coll Cardiol 2007;50:1205—13.
[10] CutterDJ,SchaapveldM,DarbySC,etal.Riskofvalvularheart diseaseaftertreatmentforHodgkinlymphoma.JNatlCancer Inst2015:107.
[11] TribouilloyC,MarechauxS,JobicY,etal.Frequencyof drug-inducedvalvularheartdiseaseinpatientspreviously exposd tobenfluorex: a multicentreprospective study.EurHeart J 2013;34:3580—7.
[12] LopezJ,RevillaA,VilacostaI,etal.Multiple-valveinfective endocarditis:clinical,microbiologic, echocardiographic,and prognosticprofile.Medicine(Baltimore)2011;90:231—6. [13] BeaudoinJ,HandschumacherMD,ZengX,etal.Mitralvalve
enlargementinchronicaorticregurgitationasacompensatory mechanismtoprevent functionalmitralregurgitationinthe dilatedleftventricle.JAmCollCardiol2013;61:1809—16. [14] LimJY,JungSH,KimJB,etal.Managementofconcomitant
mildtomoderatefunctionalmitralregurgitationduringaortic valvesurgeryforsevereaorticinsufficiency.JThorac Cardio-vascSurg2014;148:441—6.
[15] WisenbaughT,SpannJF,CarabelloBA.Differencesin myocar-dial performance and load between patients with similar amountsofchronicaorticversuschronicmitralregurgitation. JAmCollCardiol1984;3:916—23.
[16]CarabelloBA.Isitevertoolatetooperateonthepatientwith valvularheartdisease?JAmCollCardiol2004;44:376—83. [17]Gentles TL, Finucane AK, Remenyi B, Kerr AR, Wilson NJ.
Ventricular function before and after surgery for isolated and combined regurgitation in theyoung. Ann Thorac Surg 2015;100:1383—9.
[18]NilesN,BorerJS,KamenM,HochreiterC,DevereuxRB, Klig-field P.Preoperative left and right ventricular performance incombined aorticand mitralregurgitationand comparison with isolated aortic or mitral regurgitation. Am J Cardiol 1990;65:1372—8.
[19]Zoghbi WA, Adams D, Bonow RO, et al. Recommendations for noninvasive evaluation of native valvular regurgitation: a report from the american society of echocardiography developed in collaboration with the society for cardiovas-cular magnetic resonance. J AmSoc Echocardiogr 2017;30: 303—71.
[20]Hundley WG, Bluemke DA, Finn JP, et al. ACCF/ACR/AHA/NASCI/SCMR 2010 expert consensus doc-ument on cardiovascular magnetic resonance: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. Circulation 2010;121: 2462—508.
[21]Cawley PJ,Maki JH,Otto CM.Cardiovascular magnetic res-onance imaging for valvular heart disease: technique and validation.Circulation2009;119:468—78.
[22]AlashiA,MentiasA,AbdallahA,etal.Incrementalprognostic utilityofleftventriculargloballongitudinalstrainin asymp-tomaticpatientswithsignificantchronicaorticregurgitation andpreservedleftventricularejectionfraction.JACC Cardio-vascImaging2018;11:673—82.
[23]Thomas JD, Kinno M. The Prognostic Role of Global Longi-tudinalStraininSeverePrimaryMitralRegurgitation:Moving Past the Proof-of-Concept Era. JACC Cardiovasc Imaging 2018;11:1245—7.
[24]Skudicky D, Essop MR, Sareli P. Time-related changes in left ventricular function after double valve replacement for combined aortic and mitral regurgitation in a young rheumaticpopulation.Predictorsofpostoperativeleft ventric-ularperformanceandroleofchordalpreservation.Circulation 1997;95:899—904.
[25]Iung B, Baron G, Butchart EG, et al. A prospective sur-vey of patients with valvularheart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur Heart J 2003;24:1231—43.
[26]VassilevaCM, Li S, ThouraniVH, et al. Outcome character-isticsofmultiple-valvesurgery:comparisonwithsingle-valve procedures.Innovations(Phila)2014;9:27—32.
[27]CannegieterSC,RosendaalFR,WintzenAR,vanderMeerFJ, Vandenbroucke JP,Briet E.Optimaloralanticoagulant ther-apyinpatientswithmechanicalheartvalves. NEngl JMed 1995;333:11—7.
[28]UngerP,ClavelMA,LindmanBR,MathieuP,PibarotP. Patho-physiologyandmanagementofmultivalvulardisease.NatRev Cardiol2016;13:429—40.
[29]UneD,MesanaL,ChanV,etal.Clinicalimpactofchangesinleft ventricularfunctionafteraorticvalvereplacement: analysis from3112patients.Circulation2015;132:741—7.
[30]Essop MR,Wisenbaugh TW, SareliPE. Discordantchangesin leftventricularperformanceaftervalvereplacementfor iso-latedrheumatic mitralregurgitationversuscombined mitral andaortic regurgitationinteenagers.AmJCardiol1994;73: 910—4.
[31]Coutinho GF,Martinez Cereijo JM,Correia PM,et al. Long-term results after concomitant mitral and aortic valve surgery: repair or replacement? Eur J Cardiothorac Surg 2018;54:1085—92.
440 P.Ungeretal. [32]GillinovAM,BlackstoneEH,CosgroveDM3rd,etal.Mitralvalve
repairwithaorticvalvereplacementissuperiortodoublevalve replacement.JThoracCardiovascSurg2003;125:1372—87. [33]Hamamoto M, Bando K, Kobayashi J, et al. Durability and
outcome of aortic valve replacement with mitral valve repair versus double valve replacement. Ann Thorac Surg 2003;75:28—33[discussion-4].
[34]Leavitt BJ, Baribeau YR, DiScipio AW, et al. Outcomes of patients undergoing concomitant aortic and mitral valve surgery in northern New England. Circulation 2009;120:S155—62.
[35]Gillinov AM, Blackstone EH, White J, et al. Durability of combined aortic and mitral valve repair. Ann Thorac Surg 2001;72:20—7.
[36]LimGB.BenefitoftheMitraClipformitralregurgitation.Nat RevCardiol2018;15:728.
[37]Haddad A, Arwani R, Altayar O, Sawas T, Murad MH, de MarchenaE.Transcatheteraorticvalvereplacementinpatients with pure native aortic valve regurgitation: A systematic reviewandmeta-analysis.ClinCardiol2019;42:159—66. [38]Ando T, Takagi H, Briasoulis A, et al. A systematic
review of reported cases of combined transcatheter aortic and mitral valve interventions. Catheter Cardiovasc Interv 2018;91:124—34.
[39]GerosaG,D’OnofrioA,ManzanE,etal.One-stageoff-pump transapicalmitralvalverepairandaorticvalvereplacement. Circulation2015;131:e430—4.