Anarlf
meeting
Assessing
consciousness
in
coma
and
related
states
using
transcranial
magnetic
stimulation
combined
with
electroencephalography
§
E´valuation
de
la
conscience
chez
les
patients
en
coma
et
en
e´tats
apparente´s
par
stimulation
magne´tique
transcraˆnienne
combine´e
a` l’e´lectroence´phalographie
Olivia
Gosseries
a,*
,b,c,
Aurore
Thibaut
a,
Me´lanie
Boly
a,b,d,
Mario
Rosanova
e,
Marcello
Massimini
e,f,
Steven
Laureys
aa
ComaScienceGroup,CyclotronResearchCenterandNeurologyDepartment,UniversityofLie`geandUniversityHospitalofLie`ge,SartTilmanB30,alle´edu 6-Aouˆt-no
8,4031Lie`ge,Belgium
b
CenterforSleepandConsciousness,DepartmentofPsychiatry,UniversityofWisconsin,Madison,WI,USA
c
PostleLaboratory,DepartmentofPsychologyandPsychiatry,UniversityofWisconsin,Madison,WI,USA
d
DepartmentofNeurology,UniversityofWisconsin,Madison,WI,USA
e
DepartmentofBiomedicalandClinicalSciences‘‘LuigiSacco’’,UniversityofMilan,Milan,Italy
fIstitutoDiRicoveroeCuraaCarattereScientifico,FondazioneDonCarloGnocchi,20148Milan,Italy
ARTICLE INFO Keywords:
Disordersofconsciousness Unresponsivewakefulnesssyndrome Vegetativestate
Minimallyconsciousstate Locked-insyndrome
Transcranialmagneticstimulation Electroencephalography Anesthesia Sleep Brainstimulation Motscle´s: Troublesdelaconscience Syndromed’e´veilnon-re´pondant E´tatve´ge´tatif
E´tatdeconscienceminimale Locked-insyndrome
Stimulationmagne´tiquetranscraˆnienne E´lectroence´phalographie
Anesthe´sie Sommeil
Stimulationce´re´brale
ABSTRACT
Thankstoadvancesinmedicalcare,anincreasednumberofpatientsrecoverfromcoma.However,some remaininvegetative/unresponsivewakefulnesssyndromeorinaminimallyconsciousstate.Detection of awareness in severely brain-injured patients is challenging because it relies on behavioral assessments,whichcanbe affected bymotor,sensoryand cognitive impairmentsofthepatients. Othermeansofevaluationareneededtoimprovetheaccuracyofthediagnosisinthischallenging population.Wewillherereviewthedifferentalteredstatesofconsciousnessoccurringafterseverebrain damage,andexplainthedifficultiesassociatedwithbehavioralassessmentofconsciousness.Wewill thendescribeanon-invasivetechnique,transcranialmagneticstimulationcombinedwithhigh-density electroencephalography (TMS-EEG), which has allowed us to detect the presence or absence of consciousness in different physiological, pathologicaland pharmacological states. Some potential underlyingmechanismsofthelossofconsciousnesswillthenbediscussed.Inconclusion,TMS-EEGis highlypromisinginidentifyingmarkersofconsciousnessattheindividuallevelandmightbeofgreat valueforcliniciansintheassessmentofconsciousness.
ß2013Socie´te´ franc¸aised’anesthe´sieetdere´animation(Sfar).PublishedbyElsevierMassonSAS.All rightsreserved.
RE´ SUME´
Aveclesavance´esre´centesdelame´decine,deplusenplusdepatientssortentducoma.Cependant, certainsrestentene´tatve´ge´tatif/syndromed’e´veilnon-re´pondantouene´tatdeconscienceminimale. L’e´valuationdeleurniveaudeconsciencerestedifficilenotammentparcequ’ellereposesurdesexamens comportementauxquipeuventeˆtrebiaise´spardesde´ficitsmoteurs,sensorielsetcognitifs.D’autres outilsd’e´valuationdelaconsciencesontdoncne´cessairesafindepre´ciserlediagnosticdespatients se´ve`rementce´re´brole´se´s.Danscetarticle,nousexposeronslesdiffe´rentse´tatsdeconsciencealte´re´e survenanta` lasuited’unegravele´sionce´re´braleetlesdifficulte´slie´es a` l’e´valuationduniveaude conscienceauchevetdespatients.Nousde´crironsensuiteunetechniquenoninvasive,lastimulation magne´tique transcraˆnienne combine´e a` l’e´lectroence´phalographie a` haute densite´ (SMT-EEG) qui permet de de´tecter la pre´sence ou l’absence de conscience dans diffe´rents e´tats physiologiques,
§
FrenchNeuroAnesthesiaandIntensiveCareSocietyMeeting,Paris,November2013,21stand22nd:‘‘Theacutelybrain-injuredpatient:consciousnessandneuroethic’’. * Correspondingauthor.
E-mailaddress:ogosseries@ulg.ac.be(O.Gosseries).
0750-7658/$–seefrontmatterß2013Socie´te´ franc¸aised’anesthe´sieetdere´animation(Sfar).PublishedbyElsevierMassonSAS.Allrightsreserved.
1. Disordersofconsciousness
Since the invention of mechanical ventilation in the 1950s, manypatientssurviveevenafterseverebraindamage.Afterthe comatosephasewherepatientsliewitheyesclosed(i.e.,coma), somepatientsregainfullconsciousnesswhilesomeprogresstoa stateofpreservedwakefulnessintheabsenceofawareness(i.e., unresponsive wakefulness syndrome). Others show fluctuating signs of awareness but they remain unable to communicate consistently (i.e., minimally conscious state). Finally, some patients fully recover awareness but lack motor output (i.e., locked-insyndrome).
1.1. Coma
Comaisanacutestateofnon-responsivenessinwhichpatients cannot be awakened even when intensively stimulated [1]. Patientsina comalacksleep-wakecyclesand onlyshowsome reflexbehaviors[2].Theautonomousfunctionssuchasbreathing andthermoregulationarereducedandglobalbrainmetabolismis significantlydiminished[3].Comaistheresultofdiffusecorticalor whitematterdamageand/oranacutelesioninthebrainstem[4].It lastsatleastonehour(tobedistinguishedfromsyncope)andupto afewdays.Theprolongedcomaalsoexistsbutisrareandcanlast twotofiveweeks(e.g.,pharmacologically-inducedcoma). 1.2. Unresponsivewakefulnesssyndrome
Thisstatewasfirstnamedapallicsyndrome[5]orcomavigil [6], and in 1972 it was termed vegetative state [7]. New terminologywasproposedin2010–theunresponsive wakeful-ness syndrome (UWS) [8] – to avoid the strong negative connotation with inadvertently risking comparisons between patients and vegetables. The term ‘‘UWS’’ also allows a more precisedescriptionoftheclinicalstate,referringtopatientsthat are unable to react to stimuli in a non-reflexive way (hence unresponsive),whilstshowingperiodsoftimewitheyesopened (hence wakefulness). Clinically, this state is thus defined by wakefulnesswithoutawareness,andinwhichpatientsareableto open their eyes but remain unaware of the environment and themselves[9].Theyonlyshowspontaneousorstimulus-induced reflexbehaviorssuchasgrindingteeth,movingeyes,swallowing, chewing, yawning or groaning. This state may be transitory, chronicorpermanent.
Althoughrecoveryofthesleep-wakecycleispartofthecriteria of UWS, recent studies have demonstrated an absence of electrophysiologicalcharacteristicsofsleepinUWS[10,11].Brain metabolismis usually diminishedby 40 to 50% withimpaired cortico-thalamo-cortical circuits but relatively preserved brain-stem functions [12]. Brain dysfunctions are more specifically locatedinthefrontoparietalnetwork(includingbothmedialand lateralnetworksrelatedtoselfandenvironmentrespectively)and inthethalami [13]. During sensorystimulations,UWS patients usuallyshowmetabolicbrainactivationthatremainsisolatedin theprimary cortices [14,15]. Finally, top-downprocesses from frontaltotemporal corticeshavebeenshowntobeimpairedin patients in UWS when measuringthe electrical activityduring auditorystimulations[16].
1.3. Minimallyconsciousstate
The minimally conscious state (MCS) is characterized by primaryinconsistentsignsofconsciousness[17,18].Thecriteria of MCS, introducedin 2002,include reproducibleresponses to verbalorwrittencommands,visualpursuit,localizationtopain, intelligibleverbalizations,intentionalcommunicationand reach-ing/holding objects [18]. Adapted emotional behaviors such as smiles,laughsortearscanalsobeobserved[18].Thisclinicalentity hasbeenrecentlysubcategorizedin‘‘minimallyconsciousplus’’ (MCS+)forpatientswhopresenthigh-orderbehavioralresponses to stimuli (e.g., response to a command which involves the preservation of language) and ‘‘minimally conscious minus’’ (MCS ) for patients who only show low-level non-reflexive responses to stimuli (e.g., visual pursuit or localization to nociception)[19].Thisclassificationissupportedby neuroanato-mical data that demonstrate better preservation of language-relatednetworksinMCS+ascomparedtoMCS patients[20].The overall cerebral metabolic activity in MCS patients is usually reducedbuttheautonomousfunctionsarepreserved,and cortico-thalamo-corticalconnectionsarepartly restored[21].Themain metabolicdysfunctionsappeartobelocatedinthelateralnetwork and in the thalami [13]. When patients recover the ability to functionally communicate or to use objects adequately, this is referredto‘‘emergenceoftheminimallyconsciousstate’’(EMCS) [18].
1.4. Locked-insyndrome
Locked-insyndrome(LIS),alsoknownaspseudocoma,isnota disorderofconsciousnesspersebutcanbemistakenasone.LISis characterizedbyacompleteparalysisofthebodyresultingfroma lesion in the brainstem affecting the pyramidal tract, most frequentlydue toanischemic pontine lesion[17].If thelesion is onlyrestricted tothebrainstem, LISpatientshave preserved sensory and cognitive functions [22]. The primary way of communication is through vertical eye movements or blinking [23].Throughtherecoveryofdistalmovements,suchasthetipofa fingerorheadmovement,chronicLISpatientsareoftenableto communicate via a computer and to control their wheelchair. Communicationhasalsobeenrecentlymadepossibleby measur-ingelectricalbrainactivity[24]andpupilsize[25].Finally,many chronicLISpatientsreporthavingahappyandmeaningfullifeand thedemandforeuthanasia,albeitexisting,isnotsofrequent[26]. 2. Assessmentofthelevelofconsciousness
Todate,thelevelofconsciousnessis mainlyassessedatthe patient’sbedsidebysearchingforresponsetocommandor non-reflexivebehaviorsinresponsetosensorystimulations.Assessing thepresenceorabsenceofconsciousnessofnon-communicative brain-damagedpatientsishoweverdifficult,asconsciousnessisa subjective first-person experience, and one has necessarily to make inferences about its presence based on the patient’s behavior. Currently, the diagnostic decision-making process is extremelychallengingleadingtoadiagnosticerrorrateupto40% whennotassessedwithappropriatestandardizedscales[27].The ComaRecoveryScale-Revised(CRS-R)hasbeenshowntobethe
pathologiques et pharmacologiques. Des me´canismes potentiels pouvant expliquer la perte de conscienceserontensuitediscute´s.Dansnotreconclusion,nousexposeronslesavantagesdela SMT-EEGetenquoicettetechniqueprometteusepourraiteˆtred’unegrandeutilite´ poure´valuerleniveaude conscienceauchevetdespatients.
ß2013Socie´te´ franc¸aised’anesthe´sieetdere´animation(Sfar).Publie´ parElsevierMassonSAS.Tous droitsre´serve´s.
bestscaletodifferentiatebetweenUWSandMCSpatients[28,29]. Intheacutesetting,theFullOutlineofUnResponsiveness(FOUR) hasalsobeenproposedasanalternativescaleforthewidelyused Glasgow Coma Scale because it facilitates thediagnosis of LIS patients,anditincludesassessmentofvisualpursuit(oneofthe firstbehaviorsobservedwhenapatientemergesfromcoma)[30]. Even with the best clinical assessment, patients might be underestimated in terms of residual awareness due to motor dysfunction,sensorydeficit,impairedcognitionorfluctuationof vigilancethatcanpreventvoluntaryresponses[31].Recentstudies provideevidenceforpreservedawarenessinsomeUWSpatients [32].Forinstance,usingfunctionalmagneticresonanceimaging (fMRI)orelectroencephalography(EEG)suchpatientsgenerated appropriatebrainresponses,similartothoseobservedinhealthy controls, when instructed to perform cognitive tasks (e.g., activation of the supplementary motor area when asked to imagineplaying tennis)[33–35].Despitebeingunresponsive at thebedside,thesepatientsshouldbeconsidered consciousand theirdiagnosisshouldbereplaced.Theterms‘‘functionalLIS’’[19], ‘‘functional MCS’’ [36] and ‘‘MCS*’’ [37] have been recently suggestedtodefinepatientswhoshownon-behavioralevidence ofconsciousnessthatisonlymeasurablevianeuroimagingtesting. TheserecenttechnologiesusingactiveEEGandfMRIparadigms are therefore helpful in detecting consciousness in some UWS patientsbuttheycannotbeusedatthesingle-subjectlevelduetoa high rate of negative results. Moreover, these tools require preservedlanguagecomprehensionandtheactive participation of the patients. The combination of single-pulse transcranial magneticstimulation(TMS)withEEGovercomestheseissuesand canbeemployedatthebedsidetoassessbrainfunction.
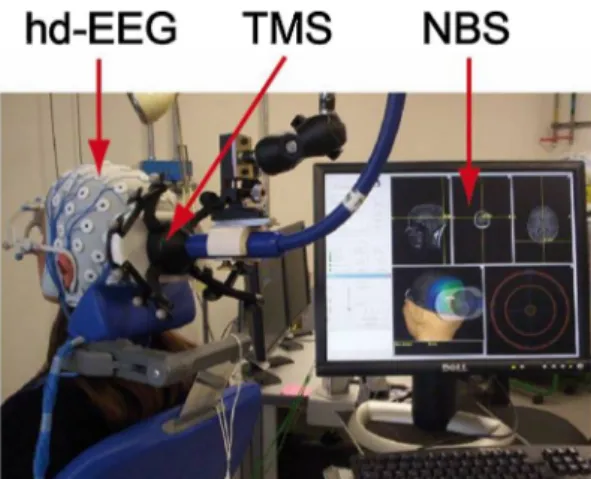
3. Transcranialmagneticstimulationcombinedwith electroencephalography
TMShasbeenusedforneurologicalandpsychiatricresearch applicationssince theearly1980s. Thisnon-invasivetechnique allowsstimulatingthecerebralcortexnon-invasivelyby generat-ingabriefbutstrongmagneticpulsethroughacoilappliedtothe surfaceof thescalp.Thefast changeinmagnetic fieldstrength inducesacurrentflowinthetissue,whichresultsintheactivation ofunderlyingneuronalpopulations[38].TMSwasfirstappliedto the motor cortex with single-pulses, and electromyography responseswererecordedfromperipheralmuscles[39].Repetitive TMS hassince beenused toinducea sustained inhibition (i.e., <1Hz)oractivation(>1Hz)oftheneuronal population,which allowed stimulating other brain areas while observing the subsequent behavioral and cognitive changes [40]. In the last severalyears,TMShasbeencombinedwithhigh-densityEEGanda neuronavigation systemtodirectly measure theactivity of the brainitself(insteadofmeasuringmuscularactivityorbehavioral responsesinducedbytheTMSstimulation)(Fig.1).Inthis way, single-pulsesTMSinducefocalneuronaldischargeatthecortex surface,and anEEGmeasurescorticalelectricalresponsesboth locally and at distant sites. This enables study of cortical excitabilityunderthesiteofstimulation,andlong-rangecortical effective connectivity (i.e., causal interactions between distant brain areas) with good spatio-temporal resolution [41]. The neuronavigationsystemallowsprecisestimulationofa selected brainareaandensuresstabilityofthepositionofthestimulationas wellasreproducibilityamongdifferentsessions[42,43].Studies demonstratedthatmeaningfulrecordingscouldbederived with-outbeingsubstantiallyaffectedbyTMS-inducedartifactthanksto newhardwaresolutions,improvedEEGamplifiertechnology,and advanced data processing techniques[44]. Using recent source modelingandstatisticalanalyses,itiscurrentlypossibletodetect
theeffectofthefocal perturbationbothatdistanceandintime [45].
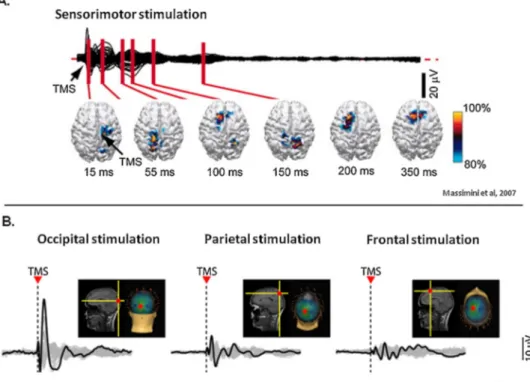
3.1. TMS-EEGinhealthyawakesubjects
Usinga60-channelTMS-compatibleEEGamplifier,Massimini et al. [46] showed that during wakefulness, TMS triggers sustained long-rangeandcomplexpatterns ofactivation.TMS induceslow-amplitudewaveshapes,whichareassociatedwith spatiallyandtemporallydifferentiatedresponses(Fig.2A)[47]. Thesebrainresponsesvarydependingonthesiteofstimulation, meaningthateachcorticalareatendstopreserveitsownnatural frequency(Fig.2B)[48].Forinstance,TMSconsistentlyevoked dominant alpha-band oscillations (8–12Hz) in the occipital cortex,beta-bandoscillations(13–20Hz)intheparietalcortex, andfastbeta-/gamma-bandoscillations(21–50Hz)inthefrontal cortex[48].Brainregionswerealsooscillatingattheirnatural frequencieswhenindirectlystimulatedby TMS,throughbrain connections. More recently, it has been shown that cortical excitabilityincreaseswithtimeawake[49].Short-termmemory taskshavealsobeenshowntoincreasetheoverallstrengthand thespatialspreadoftheelectricalcurrentsinducedbyTMS[50]. Finally,intensivetrainingonaworkingmemorytaskincreases effectiveconnectivityacrossfrontoparietalandparieto-occipital networks[51].
3.2. TMS-EEGinpatientsrecoveringfromcoma
TMS-EEGoffersaneffectivewaytoassessbrainfunctionsatrest in patients withdisorders ofconsciousnessbecauseit does not depend on the integrity of sensory and motor pathways, it bypassessubcorticalandthalamicgates,anditdoes notrequire language comprehension, nor active participation of subjects [41,52].We recordedTMS-evokedbrain responsesin17 awake patientsdiagnosedinUWS,MCSandLIS.Whenstimulatingfrontal and parietalbrainareasofUWSpatients, TMStriggeredalarge low-frequencywaveassociatedwithstronginitialcortical activa-tion, which did not propagate to adjacent brain areas, and dissipatedrapidly.Thisstereotypedandlocalslowwaveresponse indicatesabreakdownofeffectiveconnectivity[53].Bycontrast,in MCSpatients,TMStriggeredaseriesofloweramplitudeand high-frequencywavesassociatedwithcorticalactivationsthat sequen-tiallyinvolveddistantcorticalareasipsi-andcontralateraltothe site of stimulation. These complex long-lasting widespread activationpatternsweresimilartotheonesrecorded(Fig.3)[52].
Fig. 1. Set up of the TMS-EEG technique. Hd-EEG: high-density electroencephalography; TMS: transcranial magnetic stimulation; NBS: navigatedbrainstimulationincludingthestructuralMRIofthesubject. Takenfrom[42].
Through longitudinal measurements, we measured brain activityduring recovery of consciousness. When patients were inUWS,asimplelocalslowwaveresponsetoTMSwasrecorded and when patients recovered consciousness and functional communication,intracorticalconnectivityresurged[52]. Interest-ingly,oneMCSpatientwasunresponsiveatthebedsidethedayof theexperimentbut stillshowedcomplexand widespreadbrain responsestoTMS.Thissuggestsclear-cutdifferencesin intracor-ticaleffective connectivity that occur at an early stage during
recoveryofconsciousness,beforereliablecommunicationcanbe observedatthebedside.
Basedontheseresults,TMS-EEGseemstoconstituteanovel andinterestingtooltodetectsubtlediscriminationbetweenUWS andMCSatthesingle-subjectlevel,aswellastotrackrecoveryof consciousness in severely brain-injured patients. One should, however,makesuretoassessthepatientinanawakestate(i.e., eyesopen),beawareofthepotentialriskofinducingepilepsyin thisalreadyfragilepopulation,andtostimulatepreservedbrain
Fig.2.TMS-EEGinhealthyawakesubjects.A.CorticalactivationduringwakefulnessevokedbyTMSdeliveredoverthesensorimotorcortex.AveragedTMS-evokedpotentials recordedatallelectrodesandsuperimposedinabutterflydiagramalongwiththecurrentdensitydistributionhighlightingthelocationofmaximumcurrentsources.B. ResponseundertheTMSstimulation(blacktrace)andinotherlocationsofthebrain(greytraces)whenstimulatingoccipital,parietal,andfrontalcortices.Redspotillustrates thesiteoftheTMSstimulation.TMS:transcranialmagneticstimulation.
Adaptedfrom[47]and[48].
Fig.3.TMS-EEGresponsesinseverelybrain-injuredpatients.ResponseundertheTMSstimulation(blacktrace)andthefollowingspreadingoftheactivityinthebrain(colors representthelocationofthebrainareas).WhitecrossillustratesthesiteoftheTMSstimulation(parietalcortex).TMS:transcranialmagneticstimulation;L:left;R:right. Adaptedfrom[52].
areasusinganeuronavigationsystemsinceTMSappliedonabrain lesionmightinducenoresponse.
AnotherstudyrecentlyconfirmedtheabilityoftheTMS-EEGto differentiateUWSfromMCSpatientsandshowedthesuperiority of the TMS-EEG compared to traditional neurophysiological methods,suchasshort-latency somatosensoryevokedpotential andevent-relatedpotentials[54].Inthemostrecentstudy,brain responseswerecomparedbetweenconsciouspatientswithmild brain injury and healthy awake subjects [55]. Results showed alteredbrainreactivityandconnectivityintheformercomparedto thelatterthat mayberelated tocompensatory mechanismsof recovery.Largerpopulationstudiesareneededtoconfirmthese resultsandtobetterunderstand theneuralmechanisms under-lyingthefunctionalrecoveryinpost-comatosepatients.
3.3. TMS-EEGinsleepandanesthesia
ThedynamicsofTMS-EEG responseshave alsobeenstudied under physiological and pharmacological unconscious states. During non-rapid eye movement sleep, TMS triggers a simple positive-negativeslowwave,similartotheoneobservedinUWS patients[46].Dependingontheintensityofthestimulation,this slowwavecaneitherremainlocalorburstintoanexplosiveand stereotypical response.During deep sleep, thethalamo-cortical systemdespitebeingactiveandreactivethustendstobreakdown into isolated modules, and to lose the ability to produce differentiatedresponses[47].TMS-EEGresponseshavealsobeen recordedduringrapideyemovement(REM)sleepduringwhich therearedreams.In thisparadoxicalstate,corticalresponsesto TMSpropagatebeyondthestimulationsiteandlastslongerthan duringdeepsleep(althoughstill lessthanduringwakefulness), indicatingthateffectivecorticalconnectivityislargelypreserved (Fig.4)[56].
Finally,TMS-EEGhasbeenemployedduringgeneralanesthesia inducedbyapharmacologicalagent,benzodiazepinemidazolam [57].ResultsshowedthatresponsivenessofacorticalareatoTMS wasmaintainedorevenaugmented,butthespreadofactivityto adjacentareasandthereverberatoryreactivationofthestimulated sitewerequenched.Similarlyinmanyregardstowhatoccursin UWSpatientsandindeepsleep,midazolamanesthesiainducesa localslowwaveresponseand abreakdownoflong-rangebrain connectivityinresponsetoTMS.
4. Potentialmechanismsexplaining(thelossof)consciousness Aswehaveseenabove,consciousnessinvolvesmanydifferent cortical areas engaging in rapid causal interactions, whilst
unconsciousnessischaracterizedbystereotypical positive-nega-tiveslowwaveanddecreasedlarge-scalebrainconnectivity.One commonhypotheticalneurophysiologicalmechanismexplaining unconsciousnessisbistability,whichcouldunablecorticalneurons tosustainbalancedpatternsofactivation.Theresultswouldlead toasilent,hyperpolarizeddownstateaftertheinitialactivation, which could prevent the brain from successfully integrating information [58]. Potential causes of this bistability might be alterations in the balance between excitation and inhibition, increasedpotassium currents, and corticaldeafferentation[58]. Consciousness thus seems to emerge from both functional integration(i.e.,connectivity)andpreservedinformationcapacity inthebrain(i.e.,differentiationresponsesbetweenbrainregions) [59,60]. To achieve a most accurateestimation of the level of consciousness, theoretical approaches such as the Integrated InformationTheoryofConsciousness(IITC)aimatdescribingthe mechanisms involvedin consciousness [60,61]. The IITCtheory emphasizesthedynamicalcomplexity ofconsciousness, charac-terized by information being simultaneously integrated and differentiated,whereasunconsciousnessresultsfromthelossof thebrain’sabilitytointegrateinformation.Thesestatementsarein line with our TMS-EEG observations. Moreover, we recently designedareliabletheoretically-basedmeasureofconsciousness, theso-called PerturbationalComplexityIndex(PCI), inorderto quantifyinonenumbertheTMS-EEGresponsesobservedinthe aforementioned physiological,pathological andpharmacological states.
5. ThePerturbationalComplexityIndex
The PCI is a recent measure that allows estimating brain complexity, including both the information content and the integrationofbrainactivations,throughalgorithmic compres-sibility(‘‘zipping’’)[62].Thisindexhasbeenshownto success-fullydifferentiatebetweenconsciousnessandunconsciousness attheindividualsubjectlevel.Indeed,thePCIisinvariablyhigh inhealthyawakesubjects,inpatientsinMCS,EMCSandLISas well as in healthy subjects inREM sleep (i.e., above 0.3). In contrast,thePCIisalwayslowduringdeepsleep,inbothUWS patientsandinthoseundergeneralanesthesiausingmidazolam, propofolorxenon(i.e.,below0.3)(Fig.5).Furtherconfirmation studies should test the PCI on a larger cohort of patients to objectivelyandquantitativelyassessthelevelofconsciousness, butalsotodeterminetheefficacyofpharmacologicaldrugsor brain stimulation procedures in patients with disorders of consciousness.
Fig.4.TMS-EEGresponsesinsleepascomparedtowakefulness.YellowcrossillustratesthesiteoftheTMSstimulation(frontalcortex). Takenfrom[56].
6. Conclusion
Patients withdisorders ofconsciousnessconstitutea major challenge regarding diagnosis, prognosis and treatment. As clinicalassessmentfrequentlyleads todiagnosticerrors,other techniquesareneeded.TMS-EEGandPCIseemtoconstitutean appropriatemeasureto assessthe presenceor the absenceof consciousness.Duringconsciousness,thebrainisabletosustain long-range,complexpatternsof activationandthePCIishigh, whileduringunconsciousness,thisabilityislostandthePCIis low.ThePCIthuspotentiallyprovidesasimpleandreliablemetric toobjectivelymeasurethelevelofconsciousnessatthe single-subjectlevel.Futurestudiesonalargercohortofpatientsshould beconductedtoconfirmtheseinauguralresults.Moreworkisalso neededbeforeusingthistoolinroutineclinicalpractice,suchas developingcompactTMS-EEGequipmentandfast,standardized dataanalysissoftware.RepetitiveTMSshouldalsobeinvestigated fortherapeuticpurposesaspositiveeffectshavebeenobservedin a few UWS and MCS patients [63,64] as well as in patients suffering from aphasia [65], depression [66], tinnitus [67] or migraine [68]. The challenge in future years will also be to combine information coming from different neuroimaging techniquesavailable (e.g.,fMRI, TMS, EEG)in order todeepen ourunderstanding ofbrain (dys)functions and toimprovethe processofdiagnosis,aswellasinimprovingtheprognosisinthis challengingpopulation.
Disclosureofinterest
The authors declare that they have no conflicts of interest concerningthisarticle.
Acknowledgements
Thisresearchwasfunded by theBelgianNational Fundsfor Scientific Research (FNRS), Fonds Le´on-Fredericq, the James McDonnell Foundation, the European Commission, the Mind ScienceFoundation,theFrenchSpeakingCommunityConcerted ResearchAction(ARC-06/11-340),theFondationme´dicale Reine-E´lisabethandtheUniversityofLie`ge.O.G.receivedsupportfrom NIH grant MH095984toBradley R.Postle and supportfromG. Tononi. O.G. and M.B. are postdoctoral researcher and S.L. is researchdirectorattheFNRS.
References
[1]PlumF,PosnerJB.In:DavisFA,editor.Thediagnosisofstuporandcoma.3rd ed,Philadelphia:Davis;1983.
[2]TeasdaleG,JennettB.Assessmentofcomaandimpairedconsciousness.A practicalscale.Lancet1974;2:81–4.
[3]LaureysS.Scienceandsociety:death,unconsciousnessandthebrain.NatRev Neurosci2005;6:899–909.
[4]VanhaudenhuyseA,BolyM,LaureysS.Vegetativestate.Scholarpedia2009;4,
http://www.scholarpedia.org/article/Vegetative_state.
[5]Kretschmer E. Das apallische syndrom. Z Gesamte Neurol Psychiatr 1940;169:576–9.
Fig.5.ThePerturbationalComplexityIndex.A.PCIvaluesinhealthysubjects.PCImeasuredduringconsciousnessrangedbetween0.44and0.67,whereasthePCImeasuredduring unconsciousnessrangedbetween0.12and0.31.B.PCIvaluesinseverelybrain-injuredpatients.PCIprogressivelyincreasesfromunresponsivewakefulness(UWS)tominimally conscious(MCS)andtorecoveryoffunctionalcommunication(EMCS).PCIattainslevelsofhealthyawakesubjectsinLISpatients.CRS-R:ComaRecoveryScale-Revised.
[6]CalvetJ,CollJ.Meningitisofsinusoidoriginwiththeformofcomavigil.Rev Otoneuroophtalmol1959;31:443–5.
[7]JennettB,PlumF.Persistentvegetativestateafterbraindamage.Asyndrome insearchofaname.Lancet1972;1:734–7.
[8]LaureysS,CelesiaG,CohadonF,LavrijsenJ,Leo´n-Carrio´nJ,SannitaW,etal. Unresponsive wakefulness syndrome: a new name for the vegetative state or apallic syndrome.BMCMed2010;8:68.http://dx.doi.org/10.1186/1741-7015-8-68. [9]TheMulti-Society Task Forceon PVS.Medical aspectsof the persistent
vegetativestate(1).NEnglJMed1994;330:1499–508.
[10]CologanV,DrouotX,ParapaticsS,DelormeA,GruberG,MoonenG,etal.Sleep intheunresponsivewakefulnesssyndromeandminimallyconsciousstate.J Neurotrauma2013;30:339–46.
[11]LandsnessE,BrunoMA,NoirhommeQ,RiednerB,GosseriesO,SchnakersC, etal.Electrophysiologicalcorrelatesofbehaviouralchangesinvigilancein vegetativestateandminimallyconsciousstate.Brain2011;134:2222–32.
[12]GosseriesO,BrunoMA,ChatelleC,VanhaudenhuyseA,SchnakersC,SodduA,etal. Disordersofconsciousness:what’sinaname?Neurorehabilitation2011;28:3–14.
[13]ThibautA,BrunoMA,ChatelleC,GosseriesO,VanhaudenhuyseA,DemertziA, etal.Metabolicactivityin externalandinternal awarenessnetworksin severelybrain-damagedpatients.JRehabilMed2012;44:487–94.
[14]LaureysS,FaymonvilleME,DegueldreC,FioreGD,DamasP,LambermontB, etal.Auditoryprocessinginthevegetativestate.Brain2000;123:1589–601.
[15]BolyM,FaymonvilleM,PeigneuxP,LambermontB,DamasF,LuxenA,etal. Cerebralprocessingofauditoryandnoxiousstimuliinseverelybraininjured patients: differences between VS and MCS. Neuropsychol Rehabil 2005;15:283–9.
[16]BolyM,GarridoMI,GosseriesO,BrunoMA,BoverouxP,SchnakersC,etal. Preservedfeedforwardbutimpairedtop-downprocessesinthevegetative state.Science2011;332:858–62.
[17]AmericanCongressofRehabilitationMedicine.Recommendationsforuseof uniformnomenclaturepertinenttopatientswithseverealterationsof con-sciousness.ArchPhysMedRehabil1995;76:205–9.
[18]GiacinoJT,AshwalS,ChildsN,CranfordR,JennettB,Katz DI,etal.The minimally conscious state: definition and diagnostic criteria. Neurology 2002;58:349–53.
[19]BrunoMA,VanhaudenhuyseA,ThibautA,MoonenG,LaureysS.From unre-sponsivewakefulnesstominimallyconsciousPLUSandfunctionallocked-in syndromes:recentadvancesinourunderstandingofdisordersof conscious-ness.JNeurol2011;258:1373–84.
[20]BrunoMA,MajerusS,BolyM,VanhaudenhuyseA,SchnakersC,GosseriesO, etal.Functionalneuroanatomyunderlyingtheclinicalsubcategorizationof minimallyconsciousstatepatients.JNeurol2012;259:1087–98.
[21]LaureysS,FaymonvilleME,LuxenA,LamyM,FranckG,MaquetP.Restoration ofthalamocortical connectivityafter recoveryfrom persistentvegetative state.Lancet2000;355:1790–1.
[22]SchnakersC,MajerusS,GoldmanS,BolyM,VanEeckhoutP,GayS,etal. Cognitivefunctioninthelocked-insyndrome.JNeurol2008;255:323–30.
[23]BaubyJD.Lescaphandreetlepapillon.ThedivingbellandthebutterflyParis: LaffontEdition;1997,139p.
[24]LuleD,NoirhommeQ,KleihSC,ChatelleC,HalderS,DemertziA,etal.Probing commandfollowinginpatientswithdisordersofconsciousnessusinga brain-computerinterface.ClinNeurophysiol2013;124:101–6.
[25]StollJ,ChatelleC,CarterO,KochC,LaureysS,EinhauserW.Pupilresponsesallow communicationinlocked-insyndromepatients.CurrBiol2013;23:R647–8.
[26]BrunoMA,BernheimJL,LedouxD,PellasF,DemertziA,LaureysS.Asurveyon self-assessedwell-beinginacohortofchroniclocked-insyndromepatients: happymajority,miserableminority.BMJOpen2011;1:e000039.
[27]SchnakersC,VanhaudenhuyseA,GiacinoJT,VenturaM,BolyM,MajerusS, etal.Diagnosticaccuracyofthevegetativeandminimallyconsciousstate: clinicalconsensusversus standardized neurobehavioral assessment.BMC Neurol2009;9:35.
[28]GiacinoJT,KalmarK,WhyteJ.TheJFKcomarecoveryscale-revised:measurement characteristicsanddiagnosticutility.ArchPhysMedRehabil2004;85:2020–9.
[29]SeelRT,ShererM,WhyteJ,KatzDI,GiacinoJT,RosenbaumAM,etal. Assess-mentscalesfordisordersofconsciousness:evidence-basedrecommendations forclinicalpracticeandresearch.ArchPhysMedRehabil2010;91:1795–813.
[30]BrunoMA,LedouxD,LambermontB,DamasF,SchnakersC,Vanhaudenhuyse A,etal.ComparisonoftheFullOutlineofUnResponsivenessandGlasgow LiegeScale/GlasgowComaScaleinanintensivecareunitpopulation. Neuro-critCare2011;15:447–53.
[31]MajerusS,Gill-ThwaitesH,AndrewsK,LaureysS.Behavioralevaluationof consciousnessinseverebraindamage.ProgBrainRes2005;150:397–413.
[32]FaugerasF,RohautB,WeissN,BekinschteinTA,GalanaudD,PuybassetL,etal. Probingconsciousnesswithevent-relatedpotentialsinthevegetativestate. Neurology2011;77:264–8.
[33]MontiMM,VanhaudenhuyseA,ColemanMR,BolyM,PickardJD,TshibandaL, etal.Willfulmodulationofbrainactivityindisordersofconsciousness.NEngl JMed2010;362:579–89.
[34]CruseD,ChennuS,ChatelleC,BekinschteinTA,Fernandez-EspejoD,Pickard JD,etal.Bedsidedetectionofawarenessinthevegetativestate:acohortstudy. Lancet2011;378:2088–94.
[35]NaciL,OwenAM.Makingeverywordcountfornonresponsivepatients.JAMA Neurol2013.http://dx.doi.org/10.1001/jamaneurol.2013.3686[Epubahead ofprint].
[36]VogelD,Markl A, Yu T,Kotchoubey B, Lang S,MullerF. Canmental imagery functional magnetic resonance imaging predict recovery in
patients with disorders of consciousness? Arch Phys Med Rehabil 2013;94:1891–8.
[37]GosseriesO,ZaslerN,LaureysO.Recentadvancesindisordersof conscious-ness:focusonthediagnosis.BrainInj[inpress].
[38]HallettM.Transcranialmagneticstimulationandthehumanbrain.Nature 2000;406:147–50.
[39]LapitskayaN,ColemanM,NielsenJ,GosseriesO,deNoordhoutA.Disordersof consciousness:furtherpathophysiologicalinsightsusingmotorcortex tran-scranialmagneticstimulation.ProgBrainRes2009;177:191–200.
[40]MiniussiC,RossiniPM.Transcranialmagneticstimulationincognitive reha-bilitation.NeuropsycholRehabil2011;21:579–601.
[41]MassiminiM,BolyM,CasaliA,RosanovaM,TononiG. Aperturbational approachforevaluatingthebrain’scapacityforconsciousness.ProgBrain Res2009;177:201–14.
[42]Rosanova M, Casarotto S, Pigorini A,Canali P,Casali AG, MassiminiM. Combiningtranscranialmagneticstimulationwithelectroencephalography tostudyhumancorticalexcitabilityandeffectiveconnectivity.In:FellinTHM, editor.Neuronalnetworkanalysis,Neuromethods.Volume67,HumanaPress, SpringerScience+Business,LLC.p.435–457.
[43]CasarottoS,RomeroLauroLJ,BellinaV,CasaliAG,RosanovaM,PigoriniA,etal. EEGresponsestoTMSaresensitivetochangesintheperturbationparameters andrepeatableovertime.PLoSOne2010;5:e10281.
[44]RogaschNC,FitzgeraldPB.Assessingcorticalnetworkpropertiesusing TMS-EEG.HumBrainMapp2012.
[45]CasaliAG,CasarottoS,RosanovaM,MariottiM,MassiminiM.Generalindices tocharacterizetheelectricalresponseofthecerebralcortextoTMS. Neuro-image2010;49:1459–68.
[46]MassiminiM,FerrarelliF,HuberR,EsserSK,SinghH,TononiG.Breakdownof corticaleffectiveconnectivityduringsleep.Science2005;309:2228–32.
[47]MassiminiM,FerrarelliF,EsserSK,RiednerBA,HuberR,MurphyM,etal. Triggeringsleepslowwavesbytranscranialmagneticstimulation.ProcNatl AcadSciUSA2007;104:8496–501.
[48]RosanovaM,CasaliA,BellinaV,RestaF,MariottiM,MassiminiM.Natural frequenciesofhumancorticothalamiccircuits.JNeurosci2009;29:7679–85.
[49]HuberR,MakiH,RosanovaM,CasarottoS,CanaliP,CasaliA,etal.Human corticalexcitabilityincreaseswithtimeawake.CerebCortex2013;23:332–8.
[50]JohnsonJ,KunduB,CasaliA,PostleB.Task-dependentchangesincortical excitabilityandeffectiveconnectivity:acombinedTMS-EEGstudy.J Neuro-physiol2012;107:2383–92.
[51]KunduB,SuttererDW,EmrichSM,PostleBR.Strengthenedeffective con-nectivityunderliestransferofworkingmemorytrainingtotestsofshort-term memoryandattention.JNeurosci2013;33:8705–15.
[52]RosanovaM,GosseriesO,CasarottoS,BolyM,CasaliA,BrunoM,etal.Recovery ofcorticaleffectiveconnectivityandrecoveryofconsciousnessinvegetative patients.Brain2012;135(Pt4):1308–20.
[53]FristonKJ.Functionalandeffectiveconnectivity:areview.Brain Connect 2011;1:13–36.
[54]RagazzoniA,PirulliC,VenieroD,FeurraM,CincottaM,GiovannelliF,etal. Vegetativeversusminimallyconsciousstates:astudyusingTMS-EEG,sensory andevent-relatedpotentials.PLoSOne2013;8:e57069.
[55]TallusJ,LioumisP,Ha¨ma¨la¨inenH,Ka¨hko¨nenS,TenovuoO.TMS-EEGresponses inrecoveredandsymptomaticmildtraumaticbraininjury.JNeurotrauma 2013;30:1270–7.
[56]MassiminiM,FerrarelliF,MurphyM,HuberR,RiednerB,CasarottoS,etal. CorticalreactivityandeffectiveconnectivityduringREMsleepinhumans. CognNeurosci2010;1:176–83.
[57]FerrarelliF,MassiminiM,SarassoS,CasaliA,RiednerBA,AngeliniG,etal. Breakdownincorticaleffectiveconnectivityduringmidazolam-inducedloss ofconsciousness.ProcNatlAcadSciUSA2010;107:2681–6.
[58]MassiminiM,FerrarelliF,SarassoS,TononiG.Corticalmechanismsoflossof consciousness:insightfromTMS/EEGstudies.ArchItalBiol2012;150:44–55.
[59]BolyM,MassiminiM,TononiG.Theoreticalapproachestothediagnosisof alteredstatesofconsciousness.ProgBrainRes2009;177:383–98.
[60]TononiG.Consciousnessasintegratedinformation:aprovisionalmanifesto. BiolBull2008;215:216–42.
[61]Tononi G. Integrated information theory of consciousness: an updated account.ArchItalBiol2012;150:56–90.
[62]CasaliAG,GosseriesO,RosanovaM,BolyM,SarassoS,CasaliKR,etal.A theoreticallybasedindexofconsciousnessindependentofsensoryprocessing andbehavior.SciTranslMed2013;5:198ra05.
[63]Louise-BenderPapeT,RosenowJ,LewisG,AhmedG,WalkerM,GuernonA, etal.Repetitive transcranialmagnetic stimulation-associated neurobeha-vioralgainsduringcomarecovery.BrainStimul2009;2:22–35.
[64]ManganottiP,FormaggioE,StortiSF,FiaschiA,BattistinL,ToninP,etal.Effect ofhigh-frequencyrepetitivetranscranialmagneticstimulationonbrain excit-abilityinseverelybrain-injuredpatientsinminimallyconsciousorvegetative state.BrainStimul2013;6:913–21.
[65]DammekensE,VannesteS, OstJ, DeRidderD.Neuralcorrelatesofhigh frequency repetitive transcranial magnetic stimulation improvement in post-strokenon-fluentaphasia:acasestudy.Neurocase2014;20:1–9.
[66]DumasR,PadovaniR,RichieriR,Lanc¸onC.Repetitivetranscranialmagnetic stimulationinmajordepression:responsefactor.Encephale2012;38:360–8.
[67]DeRidderD,SongJ,VannesteS.FrontalcortexTMSfortinnitus.BrainStimul 2014;20:1–9.
[68]LiptonR,PearlmanS.Transcranialmagneticstimulationinthetreatmentof migraine.Neurotherapeutics2010;7:204–12.