LETTER TO THE EDITOR
Aggressive skin cancers in patients who experienced chronic
GvHD after allogeneic bone marrow transplantation
Bone Marrow Transplantation (2017) 52, 130–131; doi:10.1038/ bmt.2016.187; published online 18 July 2016
Treatment by allogeneic BMT has resulted in an increasingly large cohort of long-term survivors. However, the price of this success, as in organ transplant recipients, is the risk of cutaneous cancers.1The 20-year cumulative incidence for skin cancers after a bone marrow transplant is 6.5% for basal cell carcinoma (BCC) and 3.4% for squamous cell carcinoma (SCC).2 Compared to the general population,3 the risk for BCC is 3.1 (95% confidence
interval (CI), 1.9–5.2), for SCC is 18.3 (95% CI, 4.1–18.8) and for malignant melanoma (MM) it is 5.5 (95% CI, 1.7–17.7). The median interval from marrow transplantation to carcinoma diagnosis is 7.3–9.4 years for BCC and 2.1–7.0 years for SCC.2 The risk of skin melanoma in allogeneic transplant recipients is 3-fold higher than in renal transplant patients.3Conditioning with total-body irradiation increases the risk of BCC (HR, 3.9 (95% CI, 2.6–6.8)).3GvHD is an independent risk factor for skin cancers after BMT.4–7 Curtis et al.5showed that the risk for SCC among bone marrow transplant recipients who developed chronic GvHD was nearly 3-fold higher (relative risk (RR) = 2.79) than in patients with no acute and no chronic GvHD. Major risk factors for the development of SCC were long duration of chronic GvHD therapy (Po0.001), the use of azathioprine, particularly when combined with cyclosporine and steroids (Po0.001), and severe chronic GvHD (P = 0.004). No increase in risk was found for BCC or MM.5
The large series reporting skin carcinoma risk in hematologic patients are retrospective studies based on national registries. In consequence, there are no data on the severity of the lesions. Most patients experiencing GvHD are referred to dermatologists because of the prevalence of skin symptoms. We decided
therefore to characterize the skin cancers observed in this patient population.
We investigated the charts of patients who were bone marrow transplanted after 1983 in the hematology and pediatric departments of our institution. To have a sufficient follow-up period, we limited our search to patients transplanted before 2009. Between 1983 and 2009, 480 patients were transplanted. One-hundred and sixty-two developed cutaneous GvHD. We contacted these patients by phone to be reexamined. Many declined because they were deterred by the prospect of further medical care considering themselves as definitively cured, some had moved away from the region and were lost to follow-up, and others had died. Finally, 31 patients accepted the invitation to be examined.
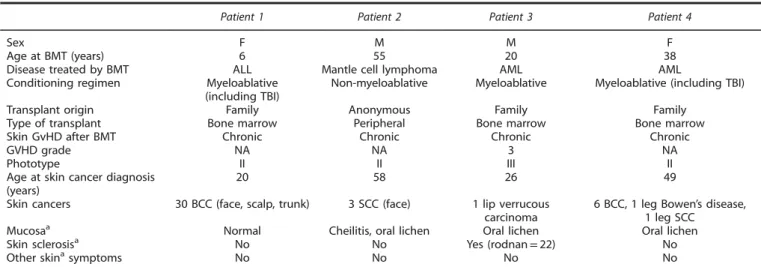
The medical history of the patients since BMT was recorded and skin and mucosa (oral and genital) were examined by a trained dermatologist. No skin or mucosal cancers were detected. Four patients, two females and two males (12.9%), had developed a total of 42 secondary skin carcinomas (36 BCC and 6 SCC). No melanoma was recorded. The median age of these patients at the time of BMT was 29 years (range, 6–55). Initial diagnosis was acute lymphocytic leukemia (1one case), acute myeloblastic leukemia (two cases) and mantle cell lymphoma (one case). None of these patients had a history of carcinoma before transplantation. The median age at skin carcinoma diagnosis was 37 years (range, 20–58) with a median interval of 8.5 years (3–14) after bone transplantation.
The first patient, a woman, bone marrow-transplanted at the age of 6, had developed 30 BCC on the face, scalp and trunk 14 years after transplant. The second was transplanted at the age of 55 and had developed three SCC on his face 3 years after transplantation. The third was a 49-year-old woman, transplanted 11 years before, who had developed six BCC, one Bowen’s
Table 1. Patients with skin cancer
Patient 1 Patient 2 Patient 3 Patient 4
Sex F M M F
Age at BMT (years) 6 55 20 38
Disease treated by BMT ALL Mantle cell lymphoma AML AML Conditioning regimen Myeloablative
(including TBI)
Non-myeloablative Myeloablative Myeloablative (including TBI) Transplant origin Family Anonymous Family Family
Type of transplant Bone marrow Peripheral Bone marrow Bone marrow Skin GvHD after BMT Chronic Chronic Chronic Chronic
GVHD grade NA NA 3 NA
Phototype II II III II
Age at skin cancer diagnosis (years)
20 58 26 49
Skin cancers 30 BCC (face, scalp, trunk) 3 SCC (face) 1 lip verrucous carcinoma
6 BCC, 1 leg Bowen’s disease, 1 leg SCC
Mucosaa Normal Cheilitis, oral lichen Oral lichen Oral lichen
Skin sclerosisa No No Yes (rodnan
= 22) No
Other skinasymptoms No No No No
Abbreviations: BCC= basal cell carcinoma; F = female; HSCT = hematopoietic stem cell transplantation; M = male; NA = not available; SCC = squamous cell carcinoma.aAt the time of skin examination.
Bone Marrow Transplantation (2017)52, 130–131 © 2017 Macmillan Publishers Limited, part of Springer Nature. All rights reserved 0268-3369/17 www.nature.com/bmt
disease and one SCC on the legs. The fourth was a 26-year-old man who had a verrucous carcinoma on the upper lip 6 years after transplantation (Table 1). In situ hybridization studies of each of these tumors were done using probes recognizing humanpoliomavirus (HPV) 6, 11, 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 66 (inform HPV II family 6 and HPV III family 16 probe, Ventana Medical Systems, USA) and did not detect viral infection. None of these carcinomas progressed to a metastatic disease. One patient had normal skin and mucosa, two had oral non-erosive lichen without other symptoms of chronic GvHD and the last had oral lichen associated with a crippling skin sclerosis. Three patients had a fair phototype (type II) and one a medium one (type III). None declared sun exposure at the workplace and all denied any excessive sun exposure during leisure time. None of these patients were smokers or regular drinkers of alcohol. No HPV was found on any tumors.
The small number of patients included in this study prevents us from establishing a statistical analysis of carcinoma incidence. Our sample may have been enriched with patients having severe forms of skin cancers and who consequently felt more concerned by such a study. In addition, the incidence of skin carcinomas in our series was 12.9%, whereas the cumulative incidence of these pathologies in large series iso7% 20 years after transplantation.5 We can nevertheless draw some conclusions regarding the clinical presentation of our patients, which was remarkable in many respects. First, most of the patients had a surprisingly high number of carcinoma lesions despite the absence of other skin risk factors such as excessive sun exposure. Second, skin lesions were observed in three patients who had been free of skin GvHD for several years. Third, skin and mucosal cancers appeared not only in the period immediately following transplantation but also410 years after. None of the patients’ lesions were metastatic. Metastatic cancers after marrow transplantation have been occasionally reported, with either skin8 or mucosal carcinoma.9
Research for the association between HPV infection and oral carcinomas in bone marrow transplanted patients gave contro-versial results10,11and no data have been published concerning
skin carcinomas. In our patients, including patient 4 with lip carcinoma, no HPV was detected in tumor cells suggesting that the role of the virus in carcinogenesis is not as constant as it is in organ transplanted patients. This difference between the two transplanted populations may be due to the lower duration of immunosuppression after bone marrow transplant. However, these data should be confirmed by additional studies.
In conclusion, the risk of skin cancer should be seriously taken into account during follow-up of patients after bone marrow transplantation. Our series suggests that these cancers can be highly relapsing, even several years after transplantation and even after resolution of GvHD. We would like to encourage our hematologist colleagues to have their marrow-transplanted patients examined annually by a dermatologist throughout life. Most skin carcinomas are induced by ultraviolet exposure and hence these patients, like organ transplant recipients, should receive advice and guidance about effective sun protection.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AS Zampaolo1, J Kanold2, O Tournilhac3, F Franck4, M Bachelerie4and M D’Incan1
1Department of Dermatology, Université d’Auvergne, CHU
Clermont-Ferrand, Clermont-Ferrand, France;
2Regional Center for Pediatric Cancerology and
Cell Therapy, Université d’Auvergne, CHU Clermont-Ferrand, Clermont-Ferrand, France;
3
Department of Hematology, Université d’Auvergne 1, CHU Clermont Ferrand, Clermont-Ferrand, France and
4
Department of Pathology, Université d’Auvergne 1, CHU Clermont-Ferrand, Clermont-Ferrand, France E-mail: annesoz_2@hotmail.fr
REFERENCES
1 Mougel F, Kanitakis J, Faure M, Euvrard S. Basosquamous cell carcinoma in organ transplant patients: a clinicopathologic study. J Am Acad Dermatol 2012;66: e151–e157.
2 DePry JL, Vyas R, Lazarus HM, Caimi PF, Gerstenblith MR, Bordeaux JS. Cutaneous malignant neoplasms in hematopoietic cell transplant recipients: a systematic review. JAMA Dermatol 2015;151: 775–782.
3 Omland SH, Gniadecki R, Hædersdal M, Helweg-Larsen J, Omland LH. Skin cancer risk in hematopoietic stem-cell transplant recipients compared with background population and renal transplant recipients: a population-based cohort study. JAMA Dermatol 2016;152: 177–183.
4 Rizzo JD, Curtis RE, Socié G, Sobocinski KA, Gilbert E, Landgren O et al. Solid cancers after allogeneic hematopoietic cell transplantation. Blood 2009;113: 1175–1183.
5 Curtis RE, Metayer C, Rizzo JD, Socié G, Sobocinski KA, Flowers MED et al. Impact of chronic GVHD therapy on the development of squamous-cell cancers after hematopoietic stem-cell transplantation: an international case-control study. Blood 2005;105: 3802–3811.
6 Schwartz JL, Kopecky KJ, Mathes RW, Leisenring WM, Friedman DL, Deeg HJ. Basal cell skin cancer after total-body irradiation and hematopoietic cell transplanta-tion. Radiat Res 2009;171: 155–163.
7 Leisenring W, Friedman DL, Flowers MED, Schwartz JL, Deeg HJ. Nonmelanoma skin and mucosal cancers after hematopoietic cell transplantation. J Clin Oncol 2006;24: 1119–1126.
8 Mittal C, Hassan S, Mattour A, Janakiraman N. Metastatic squamous cell carcinoma in a bone marrow transplant recipient. Hematol Oncol Stem Cell Ther 2013;6: 46–47.
9 Montebugnoli L, Gissi DB, Marchetti C, Foschini MP. Multiple squamous cell carcinomas of the oral cavity in a young patient with graft-versus-host disease following allogenic bone marrow transplantation. Int J Oral Maxillofac Surg 2011; 40: 556–558.
10 Katz J, Islam MN, Bhattacharyya I, Sandow P, Moreb JS. Oral squamous cell carcinoma positive for p16/human papilloma virus in post allogeneic stem cell transplantation: 2 cases and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol 2014;118: e74–e78.
11 Chen MH, Chang PM, Li WY, Hsiao LT, Hong YC, Liu CY et al. High incidence of oral squamous cell carcinoma independent of HPV infection after allogeneic hematopoietic SCT in Taiwan. Bone Marrow Transplant 2011;46: 567–572.
Letter to the Editor
131