Resuscitation
j o ur na l h o me pa g e:ww w . e l s e v i e r . c o m / l o c a t e / r e s u s c i t a t i o n
European
Resuscitation
Council
Guidelines
for
Resuscitation
2015
Section
2.
Adult
basic
life
support
and
automated
external
defibrillation
Gavin
D.
Perkins
a,b,∗,
Anthony
J.
Handley
c,
Rudolph
W.
Koster
d,
Maaret
Castrén
e,
Michael
A.
Smyth
a,f,
Theresa
Olasveengen
g,
Koenraad
G.
Monsieurs
h,i,
Violetta
Raffay
j,
Jan-Thorsten
Gräsner
k,
Volker
Wenzel
l,
Giuseppe
Ristagno
m,
Jasmeet
Soar
n,
on
behalf
of
the
Adult
basic
life
support
and
automated
external
defibrillation
section
Collaborators
1 aWarwickMedicalSchool,UniversityofWarwick,Coventry,UKbCriticalCareUnit,HeartofEnglandNHSFoundationTrust,Birmingham,UK cHadstock,Cambridge,UK
dDepartmentofCardiology,AcademicMedicalCenter,Amsterdam,TheNetherlands
eDepartmentofEmergencyMedicineandServices,HelsinkiUniversityHospitalandHelsinkiUniversity,Finland fWestMidlandsAmbulanceServiceNHSFoundationTrust,Dudley,UK
gNorwegianNationalAdvisoryUnitonPrehospitalEmergencyMedicineandDepartmentofAnesthesiology,OsloUniversityHospital,Oslo,Norway hFacultyofMedicineandHealthSciences,UniversityofAntwerp,Antwerp,Belgium
iFacultyofMedicineandHealthSciences,UniversityofGhent,Ghent,Belgium jMunicipalInstituteforEmergencyMedicineNoviSad,NoviSad,Serbia
kDepartmentofAnaesthesiaandIntensiveCareMedicine,UniversityMedicalCenterSchleswig-Holstein,Kiel,Germany lDepartmentofAnesthesiologyandCriticalCareMedicine,MedicalUniversityofInnsbruck,Innsbruck,Austria mDepartmentofCardiovascularResearch,IRCCS-IstitutodiRicercheFarmacologiche“MarioNegri”,Milan,Italy nAnaesthesiaandIntensiveCareMedicine,SouthmeadHospital,Bristol,UK
Introduction
Thischaptercontains guidanceonthetechniques used dur-ingtheinitialresuscitationofanadultcardiacarrestvictim.This includes basiclife support(BLS: airway, breathing and circula-tionsupportwithouttheuseofequipmentotherthanaprotective device)andtheuseofanautomatedexternaldefibrillator(AED). Simpletechniquesusedin themanagement ofchoking (foreign bodyairwayobstruction)arealsoincluded.Guidelinesfortheuse ofmanualdefibrillatorsandstartingin-hospitalresuscitationare foundinthesectionAdvancedLifeSupportChapter.1Asummary
oftherecoverypositionisincluded,withfurtherinformation pro-videdintheFirstAidChapter.2
TheguidelinesarebasedontheILCOR2015Consensuson Sci-enceandTreatmentRecommendations(CoSTR)forBLS/AED.3The
ILCORreviewfocusedon23keytopicsleadingto32treatment rec-ommendationsinthedomainsofearlyaccessandcardiacarrest prevention,early,high-qualityCPR, and earlydefibrillation. For theseERCguidelinestheILCOR recommendationswere supple-mentedbyfocusedliteraturereviewsundertakenbyWritingGroup membersinareasnotreviewedbyILCOR.Thewritinggroupwere
∗ Correspondingauthor.
E-mailaddress:g.d.perkins@warwick.ac.uk(G.D.Perkins).
1 The members of the Adult basic life support and automated external defibrillationsectionCollaboratorsarelistedintheCollaboratorssection.
cognisantofthecostsandpotentialconfusioncreatedbychanging guidancefrom2010,andthereforesoughttolimitchangestothose judgedtobeessentialandsupportedbynewevidence.Guidelines weredraftedbyWritingGroupmembers,thenreviewedbythe fullwritinggroupandnationalresuscitationcouncilsbeforefinal approvalbytheERCBoard.
SummaryofchangessincetheERC2010guidelines
Guidelines2015highlightsthecriticalimportanceofthe inter-actionsbetweentheemergencymedicaldispatcher,thebystander who provides CPR and the timely deployment of an auto-matedexternaldefibrillator.Aneffective,co-ordinatedcommunity responsethatdrawstheseelementstogetheriskeytoimproving survivalfromout-of-hospitalcardiacarrest(Fig.2.1).
Theemergencymedicaldispatcherplaysanimportantrolein theearlydiagnosisofcardiacarrest,theprovisionof dispatcher-assistedCPR(alsoknownastelephoneCPR),andthelocationand dispatchof anautomated external defibrillator. Thesooner the emergencyservicesarecalled,theearlierappropriatetreatment canbeinitiatedandsupported.
Theknowledge,skillsandconfidenceofbystanderswillvary accordingtothecircumstances,ofthearrest,leveloftrainingand priorexperience.
TheERCrecommendsthatthebystanderwhoistrainedandable shouldassessthecollapsedvictimrapidlytodetermineifthevictim
http://dx.doi.org/10.1016/j.resuscitation.2015.07.015
COMMUNITY RESPONSE
SAVES LIVES 112
Fig.2.1.Theinteractionsbetweentheemergencymedicaldispatcher,thebystander whoprovidesCPRandthetimelyuseofanautomatedexternaldefibrillatorarethe keyingredientsforimprovingsurvivalfromoutofhospitalcardiacarrest.
isunresponsiveandnotbreathingnormallyandthenimmediately alerttheemergencyservices.
Wheneverpossible,alerttheemergencyserviceswithout leav-ingthevictim.
Thevictimwhoisunresponsiveandnotbreathingnormallyis incardiacarrestandrequiresCPR.Immediatelyfollowingcardiac arrestbloodflowtothebrainisreducedtovirtuallyzero,whichmay causeseizure-likeepisodesthatmaybeconfusedwithepilepsy. Bystandersandemergencymedicaldispatchersshouldbe suspi-ciousofcardiacarrestinanypatientpresentingwithseizuresand carefullyassesswhetherthevictimisbreathingnormally.
Thewritinggroupendorses theILCORrecommendationthat allCPRprovidersshouldperformchestcompressionsforall vic-timsincardiacarrest.CPRproviderstrainedandabletoperform rescue breaths shouldcombine chest compressionsand rescue breaths.Theadditionofrescuebreathsmayprovideadditional ben-efitforchildren,forthosewhosustainanasphyxialcardiacarrest, orwhere theemergency medicalservice (EMS) response inter-valisprolonged.Ourconfidenceintheequivalencebetweenchest compression-onlyandstandardCPRisnotsufficienttochange cur-rentpractice.
Highqualitycardiopulmonaryresuscitationremainsessential toimprovingoutcomes.TheERC2015guidelineforchest compres-siondepthisthesameasthe2010guideline.CPRprovidersshould ensurechestcompressionsofadequatedepth(atleast5cmbutnot morethan6cm)witharateof100–120compressionsperminute. Allowthechesttorecoilcompletelyaftereachcompressionand minimiseinterruptionsincompressions.Whenprovidingrescue breaths/ventilationsspend approximately1sinflating thechest withsufficientvolumetoensurethechestrisesvisibly.Theratioof chestcompressionstoventilationsremains30:2.Donotinterrupt chestcompressionsformorethan10stoprovideventilations.
Defibrillationwithin3–5minofcollapsecanproducesurvival ratesashighas50–70%.Earlydefibrillationcanbeachievedthrough CPRprovidersusingpublicaccessandon-siteAEDs.Publicaccess AEDprogrammesshouldbeactivelyimplementedinpublicplaces thathaveahighdensityofcitizens,suchasairports,railway sta-tions,bus terminals,sportfacilities,shoppingmalls,offices and casinos.It is herethat cardiacarrests are oftenwitnessed, and trainedCPR providerscan beon-scenequickly.Placing AEDsin areaswhere one cardiacarrest per5 years canbe expected is consideredcost-effective,andthecostperaddedlife-yearis com-parable to other medical interventions. Past experience of the numberofcardiacarrestsinacertainarea,aswellasthe neighbour-hoodcharacteristics,mayhelpguideAEDplacement.Registration
ofpublicaccessAEDsallowsdispatcherstodirectCPRprovidersto anearbyAEDandmayhelptooptimiseresponse.
TheadultCPRsequencecanbeusedsafelyinchildrenwhoare unresponsiveandnotbreathingnormally.ForCPRproviderswith additionaltrainingamodifiedsequencewhichincludesproviding5 initialrescuebreathsbeforestartingchestcompressionsand delay-inggoingforhelpintheunlikelysituationthattherescuerisalone isevenmoresuitableforthechildanddrowningvictim.Chest com-pressiondepthsinchildrenshouldbeatleastonethirdofthedepth ofthechest(forinfantsthatis4cm,forchildren5cm).
Aforeignbody causingsevereairway obstructionisa medi-calemergency.Italmostalwaysoccurswhilstthevictimiseating ordrinkingandrequiresprompttreatment.Startbyencouraging thevictimtocough.Ifthevictimhassevereairwayobstructionor beginstotire,givebackblowsand,ifthatfailstorelievethe obstruc-tion,abdominalthrusts.Ifthevictimbecomesunresponsive,start CPRimmediatelywhilsthelpissummoned.
Cardiacarrest
Sudden cardiac arrest (SCA) is one of theleading causesof deathinEurope.DependinghowSCAisdefined,about55–113per 100,000inhabitantsayearor350,000–700,000individualsayear areaffectedinEurope.4–6Oninitialheart-rhythmanalysis,about
25–50%ofSCAvictimshaveventricularfibrillation(VF),a percent-agethathasdeclinedoverthelast20years.7–13Itislikelythatmany
morevictimshaveVForrapidventriculartachycardia(VT)atthe timeofcollapse,butbythetimethefirstelectrocardiogram(ECG) isrecordedbyemergencymedicalservicepersonneltheirrhythm hasdeterioratedtoasystole.14,15Whentherhythmisrecordedsoon
aftercollapse,inparticularbyanon-siteAED,theproportionof
vic-timsinVFcanbeashighas76%.16,17MorevictimsofSCAsurvive
ifbystandersactimmediatelywhileVFisstillpresent. Success-fulresuscitationislesslikelyoncetherhythmhasdeterioratedto asystole.
TherecommendedtreatmentforVFcardiacarrestis immedi-atebystanderCPRandearlyelectricaldefibrillation.Mostcardiac arrests of non-cardiac origin have respiratory causes, such as drowning (among them many children) and asphyxia. Rescue breathsaswellaschestcompressionsarecriticalforsuccessful resuscitationofthesevictims.
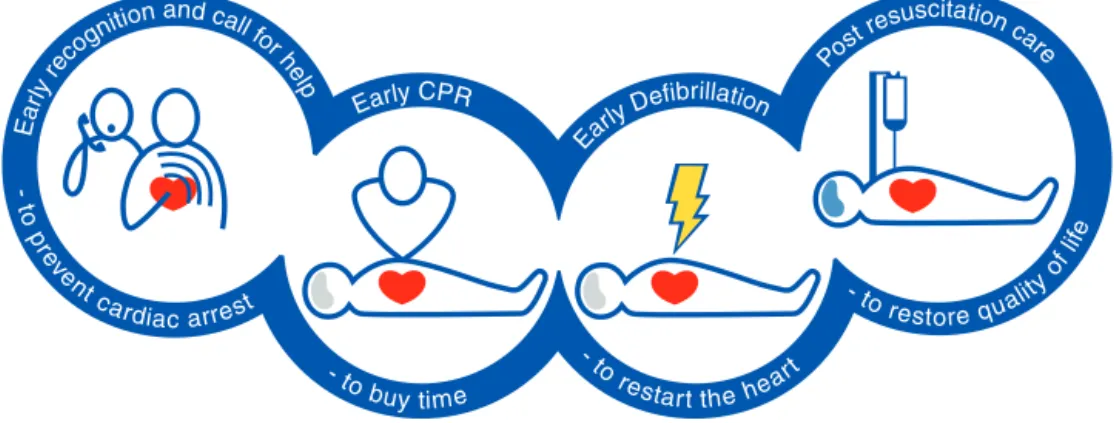
Thechainofsurvival
TheChainofSurvivalsummarisesthevitallinksneededfor suc-cessfulresuscitation(Fig.2.2).Mostoftheselinksapplytovictims ofbothprimarycardiacandasphyxialarrest.18
Earlyrecognitionandcallforhelp
Chestpainshouldberecognisedasasymptomofmyocardial ischaemia.Cardiacarrestoccursinaquartertoathirdofpatients withmyocardialischaemiawithinthefirsthourafteronsetofchest pain.19Recognisingthecardiacoriginofchestpain,andcallingthe
emergencyservicesbeforeavictimcollapses,enablesthe emer-gencymedical servicetoarrivesooner,hopefully beforecardiac arresthasoccurred,thusleadingtobettersurvival.20–23
Once cardiac arrest has occurred, early recognition is criti-caltoenablerapid activationoftheEMSand promptinitiation of bystander CPR. The key observations are unresponsiveness
andnotbreathingnormally.Emergencymedicaldispatcherscan improverecognitionbyfocusingonthesekeywords.
Fig.2.2.Thechainofsurvival.
EarlybystanderCPR
TheimmediateinitiationofCPRcandoubleorquadruple sur-vival from cardiac arrest.20,24–28 If able, bystanders with CPR
trainingshouldgivechestcompressionstogetherwithventilations. Whenabystander hasnotbeentrained in CPR,theemergency medical dispatcher should instruct him or her to give chest-compression-onlyCPRwhileawaitingthearrivalofprofessional help.29–31
Earlydefibrillation
Defibrillationwithin3–5minofcollapsecanproducesurvival ratesashighas50–70%.Thiscanbeachievedbypublicaccessand onsiteAEDs.13,17,32,33Eachminuteofdelaytodefibrillationreduces
theprobabilityofsurvivaltodischargeby10–12%.Thelinksinthe chainworkbettertogether:whenbystanderCPRisprovided,the declineinsurvivalismoregradualandaverages3–4%perminute delaytodefibrillation.20,24,34
Earlyadvancedlifesupportandstandardisedpost-resuscitation care
Advanced life support with airway management, drugs and correctingcausalfactorsmaybeneededifinitialattemptsat resus-citation are un-successful. The quality of treatmentduring the post-resuscitationphaseaffectsoutcomeandareaddressedinthe adultadvancedlifesupportandpostresuscitationcarechapters.1,35
Thecriticalneedforbystanderstoact
In most communities, the median time from emergency callto emergency medical service arrival (responseinterval) is
5–8min,16,36–38or8–11mintoafirstshock.13,27Duringthistime
thevictim’ssurvivaldependsonbystanderswhoinitiateCPRand useanautomatedexternaldefibrillator(AED).
Victimsof cardiacarrest needimmediateCPR. Thisprovides a small but critical blood flow to the heart and brain. It also increasesthelikelihood that theheartwill resumeaneffective rhythmand pumpingpower.Chestcompressionsare especially importantifashockcannotbedeliveredwithinthefirstfew min-utesaftercollapse.39Afterdefibrillation,iftheheartisstillviable,
itspacemakeractivityresumesandproducesanorganisedrhythm followedbymechanicalcontraction.Inthefirstminutesafter ter-minationofVF,theheartrhythmmaybeslow,andtheforceof contractionsweak;chestcompressionsmust becontinueduntil adequatecardiacfunctionreturns.
UseofanAEDbylayCPRprovidersincreasessurvivalfrom car-diacarrestinpublicplaces.16AEDuseinresidentialareasisalso
increasing.40AnAEDusesvoicepromptstoguidetheCPRprovider,
analysethecardiacrhythmandinstructtheCPRprovidertodeliver ashockifVForrapidventriculartachycardia(VT)isdetected.They areaccurateandwilldeliverashockonlywhenVF(orrapidVT)is present.41,42
Recognitionofcardiacarrest
Recognisingcardiacarrestcanbechallenging.Bothbystanders and emergency call handlers (emergency medical dispatchers) havetodiagnosecardiacarrestpromptlyinordertoactivatethe chainofsurvival.Checkingthecarotidpulse(oranyotherpulse) hasprovedtobeaninaccuratemethodforconfirmingthepresence orabsenceofcirculation.43–47
Agonalbreathsareslowanddeepbreaths,frequentlywitha characteristicsnoringsound.Theyoriginatefromthebrainstem, thepartofthebrainthatremainsfunctioningforsomeminutes evenwhendeprivedofoxygen.Thepresenceofagonalbreathing canbeerroneouslyinterpretedasevidencethatthereisa circu-lationand CPRisnotneeded.Agonalbreathingmaybepresent inupto40%ofvictimsinthefirstminutesaftercardiacarrest, andifrespondedtoasasignofcardiacarrest,isassociatedwith highersurvivalrates.48Thesignificanceofagonalbreathingshould
beemphasisedduringbasiclifesupporttraining.49,50Bystanders
shouldsuspectcardiacarrestandstartCPRifthevictimis unre-sponsiveandnotbreathingnormally.
Immediatelyfollowingcardiacarrest,bloodflowtothebrainis reducedtovirtuallyzero,whichmaycauseseizure-likeepisodes thatcanbeconfusedwithepilepsy.Bystandersshouldbe suspi-ciousofcardiacarrestinanypatientpresentingwithseizures.51,52
Although bystanderswho have witnessedcardiac arrest events reportchangesinthevictims’skincolour,notablypallorandbluish changesassociatedwithcyanosis,thesechangesarenotdiagnostic ofcardiacarrest.51
Roleoftheemergencymedicaldispatcher
Theemergencymedicaldispatcherplaysacriticalroleinthe diagnosisofcardiacarrest,theprovisionofdispatcherassistedCPR (alsoknownastelephoneCPR),thelocationanddispatchofan auto-matedexternal defibrillatoranddispatchofa highpriorityEMS response.Thesoonertheemergencyservicesarecalled,theearlier appropriatetreatmentcanbeinitiatedandsupported.
Dispatcherrecognitionofcardiacarrest
Confirmation of cardiac arrest, at the earliest opportunity is critical. If the dispatcher recognises cardiac arrest, survival is more likely becauseappropriate measures canbe taken.53,54
Enhancingdispatcherabilitytoidentifycardiacarrest,and optimis-ingemergencymedicaldispatcherprocesses,maybecost-effective solutionstoimproveoutcomesfromcardiacarrest.
Useofscripteddispatchprotocolswithinemergencymedical communicationcentres,includingspecificquestionstoimprove cardiac arrest recognition may be helpful. Patients who are
unresponsiveandnotbreathingnormallyshouldbepresumedto beincardiacarrest.Adherencetosuchprotocolsmayhelpimprove cardiacarrestrecognition,9,55–57whereasfailuretoadhereto
pro-tocolsreducesratesofcardiacarrestrecognitionbydispatchersas wellastheprovisionoftelephone-CPR.58–60
Obtaining an accurate description of the victim’s breathing patternischallengingfor dispatchers.Agonalbreathing isoften present, and callers may mistakenly believe the victim is still breathingnormally.9,60–68Offeringdispatchersadditional
educa-tion,specificallyaddressingtheidentificationandsignificanceof agonalbreathing,canimprovecardiacarrestrecognition,increase theprovision of telephone-CPR,67,68 and reducethe number of
missedcardiacarrestcases.64
Askingquestionsregardingtheregularityorpatternof breath-ingmayhelpimproverecognitionofabnormalbreathingandthus identificationofcardiacarrest.Iftheinitialemergencycallisfora personsufferingseizures,thecalltakershouldbehighlysuspicious ofcardiacarrest,evenifthecallerreportsthatthevictimhasaprior historyofepilepsy.61,69
DispatcherassistedCPR
BystanderCPRratesarelowinmanycommunities. Dispatcher-assistedCPR(telephone-CPR)instructionshavebeendemonstrated to improve bystander CPR rates,9,56,70–72 reduce the time to
firstCPR,56,57,68,72,73increasethenumberofchestcompressions
delivered70 and improve patient outcomes following
out-of-hospitalcardiacarrest(OHCA)inallpatientgroups.9,29–31,57,71,74
Dispatchersshouldprovidetelephone-CPRinstructions inall casesofsuspectedcardiacarrestunlessatrainedproviderisalready deliveringCPR.Whereinstructionsarerequiredforanadultvictim, dispatchersshouldprovidechest-compression-onlyCPR instruc-tions.
Ifthevictimisa child,dispatchersshouldinstructcallersto provide both ventilations and chest compressions. Dispatchers shouldthereforebetrainedtoprovideinstructionsforboth tech-niques.
AdultBLSsequence
Thesequenceofstepsfortheinitialassessmentandtreatmentof theunresponsivevictimaresummarisedinFig.2.3.Thesequence ofstepstakesthereaderthroughrecognitionofcardiacarrest, call-ingEMS,startingCPRandusinganAED.Thenumberofstepshas beenreducedtofocusonthekeyactions.Theintentoftherevised algorithmistopresentthestepsinalogicalandconcisemanner thatiseasyforalltypesofrescuerstolearn,rememberandperform.
Fig.2.4 presents the detailed step-by-step sequence for the trainedprovider.Itcontinuestohighlighttheimportanceof ensur-ingrescuer,victimandbystandersafety.Callingforadditionalhelp (ifrequired)isincorporatedinthealertingemergencyservicesstep below.Forclaritythealgorithmispresentedasalinearsequence ofsteps.Itisrecognisedthattheearlystepsofcheckingresponse, openingtheairway,checkingforbreathingandcallingthe emer-gencymedicaldispatchermaybeaccomplishedsimultaneouslyor inrapidsuccession.
Those who are not trained to recognise cardiac arrest and startCPRwouldnotbeawareoftheseguidelinesandtherefore requiredispatcherassistancewhenever theymakethedecision
Unresponsive and
not breathing normally
Call Emergency Services
Give 30 chest compressions
Give 2 rescue breaths
Continue CPR 30:2
As soon as AED arrives - switch
it on and follow instructions
Fig.2.3.TheBLS/AEDAlgorithm.
to call 112. These guidelines do not therefore include specific recommendationsforthosewhoarenottrainedtorecognise car-diacarrestandstartCPR.
Theremainderofthissectionprovidessupplemental informa-tiononsomeofthekeystepswithintheoverallsequence. Openingtheairwayandcheckingforbreathing
Thetrainedprovidershouldassessthecollapsedvictimrapidly todetermineiftheyareresponsiveandbreathingnormally.
Opentheairwayusingtheheadtiltandchinlifttechniquewhilst assessingwhetherthepersonisbreathingnormally.Donotdelay assessmentbycheckingfor obstructionsintheairway.Thejaw thrustandfingersweeparenolongerrecommendedforthelay provider.Checkfor breathingusingthetechniquesdescribedin
Fig.2.4notingthecriticalimportanceofrecognisingagonal breath-ingdescribedabove.
Alertingemergencyservices
112istheEuropeanemergencyphonenumber,available every-where in theEU,free of charge. It ispossible tocall112from fixedand mobilephonestocontact anyemergency service:an ambulance,thefirebrigadeorthepolice.SomeEuropeancountries provideanalternativedirectaccessnumbertoemergencymedical services,whichmaysavetime.Bystandersshouldthereforefollow nationalguidelinesontheoptimalphonenumbertouse.
Earlycontactwiththeemergencyserviceswillfacilitate dis-patcherassistanceintherecognitionofcardiacarrest,telephone instructiononhowtoperformCPR,emergencymedicalservice/first responderdispatch,andonlocatinganddispatchingofanAED.75–78
Ifpossible,stay withthevictimwhilecallingtheemergency services.Ifthephonehasaspeakerfacilityswitchittospeakeras thiswillfacilitatecontinuousdialoguewiththedispatcher includ-ing(ifrequired)CPRinstructions.79ItseemsreasonablethatCPR
Fig.2.4.(Continued).
trainingshouldincludehowtoactivatethespeakerphone.80
Addi-tionalbystandersmaybeusedtohelpcalltheemergencyservices. Startingchestcompressions
InadultsneedingCPR,thereisahighprobabilityofaprimary cardiaccause.Whenbloodflowstopsaftercardiacarrest,theblood in thelungs and arterial systemremains oxygenatedfor some minutes.Toemphasisethepriorityofchestcompressions,itis rec-ommendedthatCPRshouldstartwithchestcompressionsrather thaninitialventilations.Manikinstudiesindicatethatthisis asso-ciatedwithashortertimetocommencementofCPR.81–84
Whenprovidingmanualchestcompressions: 1.Delivercompressions‘inthecentreofthechest’.
2.Compresstoadepthofatleast5cmbutnotmorethan6cm. 3.Compressthechestatarateof100–120min−1withasfew
inter-ruptionsaspossible.
4.Allowthechesttorecoilcompletelyaftereachcompression;do notleanonthechest.
Handposition
Experimental studies show better haemodynamic responses whenchestcompressionsareperformedonthelowerhalfofthe sternum.85–87Itisrecommendedthatthislocationbetaughtina
simplifiedway,suchas,“placetheheelofyourhandinthecentre ofthechestwiththeotherhandontop”.Thisinstructionshouldbe accompaniedbyademonstrationofplacingthehandsonthelower halfofthesternum.88,89
ChestcompressionsaremosteasilydeliveredbyasingleCPR provider kneeling by the side of the victim, as this facilitates movementbetweencompressionsandventilationswithminimal interruptions. Over-the-head CPR for single CPR providers and
straddle-CPRfortwoCPRprovidersmaybeconsideredwhenitis notpossibletoperformcompressionsfromtheside,forexample whenthevictimisinaconfinedspace.90,91
Compressiondepth
Fearof doingharm, fatigueand limitedmusclestrength fre-quentlyresultinCPRproviderscompressingthechestlessdeeply than recommended.Four observational studies,publishedafter the2010Guidelines,suggestthatacompressiondepthrangeof 4.5–5.5cminadultsleadstobetteroutcomesthanallother com-pressiondepthsduringmanualCPR.92–95Basedonananalysisof
9136patients,compressiondepthsbetween40and55mmwith apeak at46mm,wereassociatedwithhighestsurvivalrates.94
Thereisalsoevidencefrom oneobservationalstudysuggesting thatacompressiondepthofmorethan6cmisassociatedwithan increasedrateofinjuryinadultswhencomparedwithcompression depthsof5–6cmduringmanualCPR.96TheERCendorsestheILCOR
recommendationthatitisreasonabletoaimforachest compres-sionofapproximately5cmbutnotmorethan6cmintheaverage sizedadult.Inmakingthis recommendationtheERCrecognises thatitcanbedifficulttoestimatechestcompressiondepthandthat compressionsthataretooshallowaremoreharmfulthan compres-sionsthataretoodeep.TheERCthereforedecidedtoretainthe2010 guidancethatchestcompressionsshouldbeatleast5cmbutnot morethan6cm.Trainingshouldcontinuetoprioritiseachieving adequatecompressiondepth.
Compressionrate
Chestcompressionrateisdefinedastheactualrateof compres-sionsbeinggivenatanyonetime.Itdiffersfromthenumberofchest compressionsinaspecifictimeperiod,whichtakesintoaccount anyinterruptionsinchestcompressions.
rate of 100–120min , compared to >140, 120–139, <80 and 80–99min−1.Veryhighchestcompressionrateswereassociated with declining chest compression depths.97,98 The ERC
recom-mends,therefore,thatchest compressionsshouldbeperformed atarateof100–120min−1.
Minimisingpausesinchestcompressions
Delivery of rescue breaths, shocks, ventilations and rhythm analysisleadtopausesinchestcompressions.Pre-andpost-shock pausesoflessthan10s,andchestcompressionfractions>60%are associatedwithimprovedoutcomes.99–103 Pausesinchest
com-pressionsshouldbeminimised,byensuringCPRproviderswork effectivelytogether.
Firmsurface
CPRshouldbeperformedonafirmsurfacewheneverpossible. Air-filledmattressesshouldberoutinelydeflatedduringCPR.104
Theevidencefortheuseofbackboardsisequivocal.105–109Ifa
back-boardisused,takecaretoavoidinterruptingCPRanddislodging intravenouslinesorothertubesduringboardplacement.
Chestwallrecoil
Leaningonthechestpreventingfullchestwallrecoiliscommon duringCPR.110,111Allowingcompleterecoilofthechestaftereach
compressionresultsinbettervenousreturntothechestandmay improvetheeffectivenessofCPR.110,112–114CPRprovidersshould,
therefore,takecaretoavoidleaningaftereachchestcompression.
Dutycycle
Optimaldutycycle(ratioofthetimethechestiscompressed tothe total time from one compression tothe next) hasbeen studiedinanimalmodelsandsimulationstudieswithinconsistent results.115–123Arecenthumanobservationalstudyhaschallenged
thepreviouslyrecommendeddutycycleof 50:50bysuggesting compressionphases>40%mightnotbefeasible,andmaybe associ-atedwithdecreasedcompressiondepth.124ForCPRproviders,the
dutycycleisdifficulttoadjust,andislargelyinfluencedbyother chestcompressionparameters.119,124Inreviewing theevidence,
theERCacknowledgesthereisverylittleevidencetorecommend anyspecificdutycycleand,therefore,insufficientnewevidenceto promptachangefromthecurrentlyrecommendedratioof50%.
Feedbackoncompressiontechnique
TheuseofCPRfeedbackandpromptdevicesduringCPRin clin-icalpractice is intended toimprove CPRquality as a meansof increasingthechancesofROSCandsurvival.125,126Theformsof
feedbackincludevoiceprompts,metronomes,visualdials, numer-icaldisplays,waveforms,verbalprompts,andvisualalarms.
TheeffectofCPRfeedbackorpromptdeviceshasbeenstudied intworandomisedtrials92,127and11observationalstudies.128–138
Noneofthesestudiesdemonstratedimprovedsurvivaltodischarge withfeedback,andonlyonefoundasignificantlyhigherROSCrate inpatientswherefeedbackwasused.However,inthisstudy feed-backwasactivatedatthediscretionofthephysicianandnodetails ofthedecision-makingprocesstoactivateornotactivatefeedback wereprovided.136TheuseofCPRfeedbackorpromptdevices
dur-ingCPRshouldonlybeconsideredaspartofabroadersystemof carethatshouldincludecomprehensiveCPRqualityimprovement initiatives,138,139ratherthanasanisolatedintervention.
Innon-paralysed,gaspingpigswithunprotected,unobstructed airways,continuous-chest-compressionCPRwithoutartificial ven-tilationresultedinimprovedoutcome.140Gaspingmaybepresent
earlyaftertheonsetofcardiacarrestinaboutonethirdofhumans, thusfacilitatinggasexchange.48DuringCPRinintubatedhumans,
however,themediantidalvolumeperchestcompressionwasonly about40mL,insufficientforadequateventilation.141Inwitnessed
cardiacarrestwithventricularfibrillation,immediatecontinuous chest compressions tripledsurvival.142 Accordingly, continuous
chest compressions maybe most beneficial in the early, ‘elec-tric’and‘circulatory’phasesofCPR,whileadditionalventilation becomesmoreimportantinthelater,‘metabolic’phase.39
DuringCPR,systemic bloodflow,andthusblood flowtothe lungs,issubstantiallyreduced,solowertidalvolumesand respi-ratoryratesthannormalcanmaintaineffectiveoxygenationand ventilation.143–146 Whentheairway is unprotected,a tidal
vol-ume of 1L produces significantly more gastric inflation than a tidal volume of 500mL.147 Inflation durations of 1sare
feasi-blewithoutcausingexcessivegastricinsufflation.148Inadvertent
hyperventilationduringCPRmayoccurfrequently,especiallywhen usingmanualbag-valve-maskventilationin aprotectedairway. While this increasedintrathoracic pressure149 and peak airway
pressure,150acarefullycontrolledanimalexperimentrevealedno
adverseeffects.151
FromtheavailableevidencewesuggestthatduringadultCPR tidal volumes of approximately 500–600mL (6–7mLkg−1) are delivered.Practically,thisisthevolumerequiredtocausethechest torisevisibly.152CPRprovidersshouldaimforaninflation
dura-tionofabout1s,withenoughvolumetomakethevictim’schest rise,butavoidrapidorforcefulbreaths.Themaximum interrup-tioninchestcompressiontogivetwobreathsshouldnotexceed 10s.153Theserecommendationsapplytoallformsofventilation
duringCPRwhentheairwayisunprotected,including mouth-to-mouthandbag-maskventilation,withandwithoutsupplementary oxygen.
Mouth-to-noseventilation
Mouth-to-nose ventilation is an acceptable alternative to mouth-to-mouthventilation.154Itmaybeconsideredifthevictim’s
mouthisseriouslyinjuredorcannotbeopened,theCPRprovideris assistingavictiminthewater,oramouth-to-mouthsealisdifficult toachieve.
Mouth-to-tracheostomyventilation
Mouth-to-tracheostomyventilationmaybeusedforavictim withatracheostomytubeortrachealstomawhorequiresrescue breathing.155
Compression–ventilationratio
Animaldatasupporta ratioofcompressiontoventilationof greaterthan15:2.156–158 Amathematicalmodel suggeststhata
ratioof30:2providesthebestcompromise betweenbloodflow andoxygendelivery.159,160Aratioof30:2wasrecommendedin
Guidelines2005and2010forthesingleCPRproviderattempting resuscitationofanadult.Thisdecreasedthenumberof interrup-tionsincompressionandtheno-flowfraction,161,162andreduced
the likelihood of hyperventilation.149,163 Several observational
studieshavereportedslightlyimprovedoutcomesafter implemen-tationoftheguidelinechanges,whichincludedswitchingfroma compressionventilationratioof15:2–30:2.161,162,164,165 TheERC
continues,therefore,torecommendacompressiontoventilation ratioof30:2.
Compression-onlyCPR
Animalstudieshaveshownthatchest-compression-onlyCPR maybeaseffectiveascombinedventilationandcompressionin thefirstfewminutesafternon-asphyxialarrest.140,166Animaland
mathematicalmodelstudiesofchest-compression-onlyCPRhave alsoshownthatarterialoxygenstoresdepletein2–4min.158,167If
theairwayisopen,occasionalgaspsandpassivechestrecoilmay providesomeairexchange.48,141,168–170
Observationalstudies,classifiedmostlyasverylow-quality evi-dence,havesuggestedequivalenceofchest-compression-onlyCPR andchestcompressionscombinedwithrescuebreathsinadults withasuspectedcardiaccausefortheircardiacarrest.26,171–182
TheERChascarefullyconsideredthebalancebetween poten-tialbenefitand harmfrom compression-only CPRcompared to standardCPRthatincludesventilation.Ourconfidenceinthe equiv-alencebetweenchest-compression-onlyandstandardCPRisnot sufficienttochangecurrentpractice.TheERC,therefore,endorses theILCORrecommendations that allCPR providersshould per-formchest compressionsfor all patientsin cardiac arrest. CPR providerstrainedandabletoperformrescuebreathsshould per-formchestcompressionsandrescuebreathsasthismayprovide additionalbenefitforchildrenandthosewhosustainan asphyx-ialcardiacarrest175,183,184orwheretheEMSresponseintervalis
prolonged.179
Useofanautomatedexternaldefibrillator
AEDs are safe and effective when used by laypeople with minimalornotraining.185 AEDsmake itpossibletodefibrillate
many minutes before professional help arrives. CPR providers shouldcontinueCPRwithminimalinterruptionofchest compres-sionswhile attachinganAED andduringitsuse. CPRproviders shouldconcentrateonfollowingthevoicepromptsimmediately when they are spoken, in particular resuming CPR as soon as instructed, and minimizing interruptions in chest compression. Indeed,pre-shockandpost-shockpausesinchestcompressions shouldbeasshortaspossible.99,100,103,186StandardAEDsare
suit-ableforuseinchildrenolderthan8years.187–189
Forchildrenbetween1and8yearspaediatricpadsshouldbe used,togetherwithanattenuatororapaediatricmodeifavailable; ifthesearenotavailable,theAEDshouldbeusedasitis.Thereare afewcasereportsofsuccessfuluseofAEDSinchildrenagesless than1year.190,191Theincidenceofshockablerhythmsininfants
isverylowexceptwhenthereiscardiacdisease.187–189,192–195In
theserarecases,ifanAEDistheonlydefibrillatoravailable,itsuse shouldbeconsidered(preferablywithadoseattenuator). CPRbeforedefibrillation
Theimportanceof immediatedefibrillationhasalwaysbeen emphasisedinguidelinesandduringteaching,andisconsidered tohavea majorimpactonsurvivalfromventricularfibrillation. Thisconceptwaschallengedin2005becauseevidencesuggested thataperiodofupto180sofchestcompressionbefore defibrilla-tionmightimprovesurvivalwhentheEMSresponsetimeexceeded
4–5min.196,197Threemorerecenttrialshavenotconfirmedthis
survivalbenefit.198–200 Ananalysisofonerandomised trial
sug-gestedadeclineinsurvivaltohospitaldischargebyaprolonged periodofCPR(180s)anddelayeddefibrillationinpatientswith ashockableinitialrhythm.200 Yet,forEMSagencieswithhigher
baselinesurvival-to-hospitaldischargerates(definedas>20%for aninitialshockablerhythm),180sofCPRpriortodefibrillationwas morebeneficialcomparedtoashorterperiodofCPR(30–60s).201
The ERC recommends that CPR should be continued while a
defibrillatororAEDisbeingbroughton-siteandapplied,but defi-brillationshouldnotbedelayedanylonger.
Intervalbetweenrhythmchecks
The2015ILCORConsensusonSciencereportedthatthereare currentlynostudies that directlyaddress thequestionof opti-malintervalsbetweenrhythmchecks,andtheireffectonsurvival: ROSC;favourableneurologicalorfunctionaloutcome;survivalto discharge;coronaryperfusionpressureorcardiacoutput.
InaccordancewiththeILCORrecommendation,andfor consis-tencywithpreviousguidelines,theERCrecommendsthatchest compressionsshouldbepausedeverytwominutestoassessthe cardiacrhythm.
Voiceprompts
ItiscriticallyimportantthatCPRproviderspayattentiontoAED voicepromptsandfollowthemwithoutanydelay.Voiceprompts areusuallyprogrammable,anditisrecommendedthattheybeset inaccordancewiththesequenceofshocksandtimings forCPR givenabove.Theseshouldincludeatleast:
1.minimisepausesinchestcompressionsforrhythmanalysisand charging;
2.asingleshockonly,whenashockablerhythmisdetected; 3.avoicepromptforimmediateresumptionofchestcompression
aftertheshockdelivery;
4.aperiod of2minofCPRbeforethenextvoicepromptto re-analysetherhythm.
DevicesmeasuringCPRqualitymayinadditionprovide real-timeCPRfeedbackandsupplementalvoice/visualprompts.
The duration of CPR between shocks, as well as the shock sequenceandenergylevelsarediscussedfurtherintheAdvanced LifeSupportChapter.1
Inpractice,AEDsareusedmostlybytrainedrescuers,where thedefaultsettingofAEDpromptsshouldbeforacompressionto ventilationratioof30:2.
If(inanexception)AEDsare placedina settingwhere such trainedrescuersareunlikelytobeavailableorpresent,theowner ordistributormaychoosetochangethesettingstocompression only.
Fully-automaticAEDs
Havingdetectedashockablerhythm,afullyautomaticAEDwill deliverashockwithoutfurtheractionfromtheCPRprovider.One manikinstudyshowedthatuntrainednursingstudentscommitted fewersafetyerrorsusingafullyautomaticAEDcomparedwitha semi-automaticAED.202Asimulatedcardiacarrestscenarioona
manikinshowedthatsafetywasnotcompromisedwhenuntrained layCPRprovidersusedafullyautomaticAEDratherthana semi-automaticAED.203Therearenohumandatatodeterminewhether
thesefindingscanbeappliedtoclinicaluse. Publicaccessdefibrillation(PAD)programmes
Theconditionsforsuccessfulresuscitationinresidentialareas arelessfavourablethaninpublicareas:fewerwitnessedarrests, lowerbystanderCPR ratesand,asa consequence,fewer shock-ablerhythmsthaninpublicplaces.Thislimitstheeffectiveness ofAED usefor victimsathome.204 Moststudiesdemonstrating
able,victimswere defibrillatedmuch sooner and witha better chanceof survival.16,209 However, anAED delivereda shock in
only 3.7%209 or 1.2%16 of all cardiac arrests.There wasa clear
inverserelationshipintheJapanesestudybetweenthenumber ofAEDsavailable persquare km andthe intervalbetween col-lapseandthefirstshock,leadingtoapositiverelationshipwith survival.
PublicaccessAEDprogrammesshould,therefore,beactively implementedinpublicplaceswithahighdensityandmovement ofcitizenssuchasairports,railwaystations,busterminals,sport facilities,shoppingmalls,officesandcasinoswherecardiacarrests areusuallywitnessedand trainedCPRproviderscanquicklybe onscene. Thedensity and location of AEDsrequired for a suf-ficientlyrapid responseisnotwellestablished,especially when cost-effectivenessisaconsideration.Factorssuchasexpected inci-dence of cardiac arrest, expected number of life-years gained, andreduction inresponsetime ofAED-equippedCPR providers comparedtothatoftraditionalEMSshouldinformthisdecision. PlacementofAEDsinareaswhereonecardiacarrestper5years canbeexpectedis consideredcost-effectiveand comparableto othermedicalinterventions.210–212Forresidentialareas,past
expe-rience may help guide AED placement, as may neighbourhood characteristics.213,214RegistrationofAEDsforpublicaccess,sothat
dispatcherscandirect CPRproviderstoanearbyAED,mayalso helptooptimiseresponse.215Costsavingisalsopossible,asearly
defibrillationand on-siteAEDdefibrillationmayresultinlower in-hospitalcost.216,217
ThefullpotentialofAEDshasnotyetbeenachieved,because theyare mostly used in public settings, yet60–80% of cardiac arrestsoccurathome.TheproportionofpatientsfoundinVFis lowerathomethaninpublicplaces,howevertheabsolute num-berofpotentiallytreatablepatientsishigherathome.204 Public
accessdefibrillation(PAD)rarelyreachesvictimsathome.208
Dif-ferentstrategies,therefore,arerequiredforearlydefibrillationin residentialareas.Dispatchedfirstresponders,suchaspoliceand firefighterswill,ingeneral,havelongerresponsetimes,butthey havethepotentialtoreachthewholepopulation.17,36Thelogistic
problemforfirstresponderprogrammesisthattheCPRprovider needstoarrive,not justearlier thanthetraditionalambulance, butwithin5–6minoftheinitialcall,toenableattempted defi-brillationintheelectricalorcirculatoryphaseofcardiacarrest.39
With longerdelays, the survival benefit decreases: a few min-utes gain intime will haveless impact whena first responder arrivesmorethan10minafterthecall.34,218 DispatchedlayCPR
providers, local to the victim and directed to a nearby AED, mayimprovebystanderCPRrates33andhelpreducethetimeto
defibrillation.40
WhenimplementinganAEDprogramme,communityand pro-gramme leaders should consider factors such as development of a team with responsibility for monitoring, maintaining the devices,trainingandretrainingindividualswhoarelikelytouse theAED,andidentificationofagroupofvolunteerindividualswho arecommittedtousingtheAEDforvictimsofcardiacarrest.219
Fundsmust beallocatedona permanent basisto maintainthe programme.
ProgrammesthatmakeAEDsavailableinresidentialareashave onlybeenevaluatedforresponsetime,notforsurvivalbenefit.40
Theacquisition ofan AEDfor individual useathome,even for those considered at high risk of sudden cardiac arrest is not effective.220
Thespecialcircumstanceschapterprovidestheevidence under-pinningtheERCrecommendationthatAEDsshouldbemandatory onboardallcommercialaircraftinEurope,includingregionaland low-costcarriers.221
simple and clearsignageindicating thelocation ofan AEDand the fastest way to it is important. ILCOR has designed such an AED sign that may be recognised worldwide and this is recommended.222
In-hospitaluseofAEDs
Therearenopublishedrandomisedtrialscomparingin-hospital useofAEDswithmanualdefibrillators.Twoolder,observational studiesof adultswithin-hospital cardiacarrestfrom shockable rhythmsshowedhighersurvival-to-hospitaldischargerateswhen defibrillationwasprovidedthroughanAEDprogrammethanwith manual defibrillation alone.223,224 A more recent observational
studyshowedthatanAEDcouldbeusedsuccessfullybeforethe arrivalofthehospitalresuscitationteam.225 Threeobservational
studiesshowednoimprovementsinsurvivaltohospitaldischarge for in-hospital adult cardiac arrest when using an AED com-paredwithmanualdefibrillation.226–228Inoneofthesestudies,226
patientsintheAEDgroupwithnon-shockablerhythmshadalower survival-to-hospital discharge rate compared withthose in the manualdefibrillatorgroup(15%vs.23%;P=0.04).Anotherlarge observational study of 11,695patients from 204hospitals also showed that in-hospital AED use was associated with a lower survival-to-dischargeratecomparedwithnoAEDuse(16.3%vs. 19.3%;adjustedrateratio[RR],0.85;95%confidenceinterval[CI], 0.78–0.92;P<0.001).229Fornon-shockablerhythms,AEDusewas
associatedwithlowersurvival(10.4%vs.15.4%;adjustedRR,0.74; 95%CI,0.65–0.83;P<0.001),andasimilarsurvivalratefor shock-ablerhythms,(38.4%vs.39.8%;adjustedRR,1.00;95%CI,0.88–1.13; P=0.99).This suggeststhat AEDs maycause harmful delays in starting CPR,orinterruptions inchest compressionsin patients with non-shockable rhythms.230 Only a small proportion (less
than20%)ofin-hospitalcardiacarrestshaveaninitialshockable rhythm.229,231,232
WerecommendtheuseofAEDsinthoseareasofthehospital wherethereisariskofdelayeddefibrillation,233 becauseit will
takeseveralminutesforaresuscitationteamtoarrive,andfirst respondersdonothaveskillsinmanualdefibrillation.Thegoalis toattemptdefibrillationwithin3minofcollapse.Inhospitalareas wherethereisrapidaccesstomanualdefibrillation,eitherfrom trainedstafforaresuscitationteam,manualdefibrillationshould beusedinpreferencetoanAED.Whicheverdefibrillationtechnique ischosen(andsomehospitalsmaychoosetohavedefibrillators thatofferbothanAEDandmanualmode)aneffectivesystemfor trainingandretrainingshouldbeinplace.232,234Sufficient
health-careprovidersshouldbetrainedtoenablethegoalofproviding thefirstshockwithin3minofcollapseanywhereinthehospital. Hospitalsshouldmonitorcollapse-to-firstshockintervalsandaudit resuscitationoutcomes.
RiskstotheCPRproviderandrecipientsofCPR
RiskstothevictimwhoreceivesCPRwhoisnotincardiacarrest ManyCPRprovidersdonotinitiateCPRbecausetheyare con-cernedthatdeliveringchestcompressionstoavictimwhoisnotin cardiacarrestwillcauseseriouscomplications.Threestudieshave investigatedtheriskofCPRinpersonsnotincardiacarrest.235–237
Pooleddatafromthesethreestudies,encompassing345patients, foundanincidenceofbonefracture(ribsandclavicle)of1.7%(95% CI0.4–3.1%),painintheareaofchestcompression8.7%(95%CI 5.7–11.7%),andnoclinicallyrelevantvisceralinjury.BystanderCPR extremelyrarelyleadstoseriousharminvictimswhoare even-tuallyfoundnottobeincardiacarrest.CPRprovidersshouldnot,
therefore,bereluctanttoinitiateCPRbecauseofconcernofcausing harm.
RiskstothevictimwhoreceivesCPRwhoisincardiacarrest Asystematicreviewofskeletalinjuriesaftermanualchest com-pressionreportsanincidenceofribfracturesrangingfrom13%to 97%,andofsternalfracturesfrom1%to43%.238 Visceralinjuries
(lung,heart,abdominalorgans)occurlessfrequentlyandmayor maynotbeassociatedwithskeletalinjury.239Injuriesaremore
commonwhenthedepthofchestcompressionexceeds6cminthe averageadult.96
RiskstotheCPRproviderduringtrainingandduringreal-lifeCPR ObservationalstudiesoftrainingoractualCPRperformanceand casereportshavedescribedrareoccurrencesofmusclestrain,back symptoms,shortnessofbreath,hyperventilation,pneumothorax, chestpain,myocardialinfarctionandnerveinjury.240,241The
inci-denceof theseeventsis verylow, and CPR trainingand actual performanceissafeinmostcircumstances.242Individuals
under-takingCPRtrainingshouldbeadvisedofthenatureandextentofthe physicalactivityrequiredduringthetrainingprogramme.Learners andCPRproviderswhodevelopsignificantsymptoms(e.g.chest painorsevereshortnessofbreath)duringCPRtrainingshouldbe advisedtostop.
CPRproviderfatigue
Severalmanikin studies have foundthat chest compression depthcandecrease assoonastwo minutesafterstarting chest compressions.243Anin-hospitalpatientstudyshowedthat,even
whileusingreal-time feedback,themeandepthofcompression deterioratedbetween1.5and3minafterstartingCPR.244Itis
there-forerecommendedthatCPRproviderschangeoverabouteverytwo minutestopreventadecreaseincompressionqualityduetoCPR providerfatigue.ChangingCPRprovidersshouldnotinterruptchest compressions.
Risksduringdefibrillation
ManystudiesofpublicaccessdefibrillationshowedthatAEDs canbeused safelyby laypeopleand firstresponders.185 A
sys-tematic review identified eight papers that reported a total of 29 adverse events associated with defibrillation.245 The causes
includedaccidentalorintentionaldefibrillatormisuse,device mal-functionandaccidentaldischargeduringtrainingormaintenance procedures. Four single-case reports described shocks to CPR providersfromdischargingimplantablecardioverterdefibrillators (ICDs),inonecaseresultinginaperipheralnerveinjury.No stud-ieswereidentified whichreportedharmtoCPRprovidersfrom attemptingdefibrillationinwetenvironments.
AlthoughinjurytotheCPRproviderfromadefibrillatorshock isextremelyrare,ithasbeenshownthatstandardsurgicalgloves donotprovideadequateprotection.246–249CPRproviders,
there-fore,shouldnotcontinuemanualchestcompressionsduringshock delivery,andvictimsshouldnotbetouchedduringICDdischarge. DirectcontactbetweentheCPRproviderandthevictimshouldbe avoidedwhendefibrillationisperformed.
Psychologicaleffects
One large, prospective trial of public access defibrillation reportedfewadversepsychologicaleffectsassociatedwithCPRor AEDusethat requiredintervention.242 Twolarge, retrospective,
questionnaire-basedstudiesfoundthatbystanderswhoperformed CPR regarded theirintervention as a positive experience.250,251
Family members witnessing a resuscitation attempt may also derivepsychologicalbenefit.252–254Therareoccurrencesofadverse
psychologicaleffectsinCPRprovidersafterperformingCPRshould berecognisedandmanagedappropriately.
Diseasetransmission
TheriskofdiseasetransmissionduringtrainingandactualCPR performanceisextremelylow.255–257WearingglovesduringCPR
isreasonable,butCPRshouldnotbedelayedorwithheldifgloves arenotavailable.
Barrierdevicesforusewithrescuebreaths
Threestudiesshowedthatbarrierdevicesdecrease transmis-sionofbacteriaduringrescuebreathingincontrolledlaboratory settings.258,259 No studies were identified which examinedthe
safety,effectivenessorfeasibilityofusingbarrierdevices(suchas afaceshieldorfacemask)topreventvictimcontactwhen per-formingCPR.Neverthelessifthevictimisknowntohaveaserious infection(e.g.HIV,tuberculosis,hepatitisBorSARS)abarrierdevice isrecommended.
Ifabarrierdeviceisused,careshouldbetakentoavoid unneces-saryinterruptionsinCPR.Manikinstudiesindicatethatthequality ofCPRissuperiorwhenapocketmaskisusedcomparedtoa bag-valvemaskorsimplefaceshield.260–262
Foreignbodyairwayobstruction(choking)
Foreign body airway obstruction (FBAO) is an uncommon but potentially treatable cause of accidental death.263 Asmost
chokingeventsareassociatedwitheating,theyarecommonly wit-nessed. Asvictims initiallyare consciousand responsive,there areoftenopportunitiesforearlyinterventionswhichcanbelife saving.
Recognition
Becauserecognitionofairwayobstructionisthekeyto success-fuloutcome,itisimportantnottoconfusethisemergencywith fainting,myocardialinfarction,seizureorotherconditionsthatmay causesuddenrespiratorydistress,cyanosisorlossofconsciousness. FBAOusuallyoccurswhilethevictimiseatingordrinking. Peo-pleatincreasedriskofFBAOincludethosewithreducedconscious levels,drugand/oralcoholintoxication,neurologicalimpairment withreducedswallowingandcoughreflexes(e.g.stroke, Parkin-son’sdisease),respiratorydisease,mentalimpairment,dementia, poordentitionandolderage.264
Fig.2.5 presentsthetreatmentalgorithm for theadult with FBAO. Foreign bodies may cause either mild or severe airway obstruction.Itisimportanttoasktheconsciousvictim“Areyou choking?”Thevictimthatisabletospeak,coughandbreathehas mildobstruction.Thevictimthatisunabletospeak,hasa weak-eningcough,isstrugglingorunabletobreathe,hassevereairway obstruction.
Treatmentformildairwayobstruction
Coughinggenerateshighandsustainedairwaypressuresand mayexpeltheforeignbody.Aggressivetreatmentwithbackblows, abdominalthrustsandchestcompressions,maycauseharmand canworsentheairwayobstruction.Thesetreatmentsshouldbe reservedforvictimswhohavesignsofsevereairwayobstruction. Victimswithmildairwayobstructionshouldremainunder contin-uousobservationuntiltheyimprove,assevereairwayobstruction maysubsequentlydevelop.
Treatmentforsevereairwayobstruction
Theclinicaldataonchokingarelargelyretrospectiveand anec-dotal. For conscious adults and children over one year of age
Fig.2.5.(Continued).
withcompleteFBAO,casereports havedemonstratedthe effec-tiveness of back blows or ‘slaps’, abdominal thrusts and chest thrusts.265 Approximately50%ofepisodesofairwayobstruction
arenotrelievedbyasingletechnique.266 Thelikelihoodof
suc-cessisincreasedwhencombinationsofbackblowsorslaps,and abdominalandchestthrustsareused.265
Treatmentofforeignbodyairwayobstructioninanunresponsive victim
Arandomisedtrialincadavers267 and twoprospective
stud-iesinanaesthetisedvolunteers268,269showedthathigherairway
pressurescan begenerated using chest thrusts compared with abdominalthrusts.Bystanderinitiationofchestcompressionfor unresponsiveorunconsciousvictimsofFBAOwasindependently associatedwithgoodneurologicaloutcome(oddsratio,10.57;95% CI,2.472–65.059,P<0.0001).270Chestcompressionsshould,
there-fore,bestartedpromptlyifthevictimbecomesunresponsiveor unconscious.After30compressionsattempt2rescuebreaths,and continueCPRuntilthevictimrecoversandstartstobreathe nor-mally.
Aftercareandreferralformedicalreview
FollowingsuccessfultreatmentofFBAO,foreignmaterialmay neverthelessremain in the upper or lower airways and cause complications later. Victims with a persistent cough, difficulty swallowingorthesensationofanobjectbeingstillstuckinthe throatshould,therefore,bereferredforamedicalopinion. Abdom-inalthrustsandchestcompressionscanpotentiallycauseserious internalinjuries and all victimssuccessfully treated withthese measuresshouldbeexaminedafterwardsforinjury.
Resuscitationofchildren(seealsoRecognitionofCardiac Arrestsection)andvictimsofdrowning(seealsoTheChain ofSurvivalsection)
Manychildrendonotreceiveresuscitationbecausepotential CPRprovidersfearcausingharmiftheyarenotspecificallytrained inresuscitationforchildren.Thisfearisunfounded:itisfarbetter tousetheadultBLSsequenceforresuscitationofachildthanto donothing.Foreaseofteachingandretention,laypeopleshould betaughtthattheadultsequencemayalsobeusedforchildren whoarenotresponsiveandnotbreathingnormally.Thefollowing minormodificationstotheadultsequencewillmakeitevenmore suitableforuseinchildren:
• Give5initialrescuebreathsbeforestartingchestcompressions. • GiveCPRfor1minbeforegoingforhelpintheunlikelyeventthe
CPRproviderisalone.
• Compressthechestbyatleastonethirdofitsdepth;use2fingers foraninfantunderoneyear;use1or2handsforachildover1 yearasneededtoachieveanadequatedepthofcompression.
Thesamemodificationsof5initialbreathsand1minofCPRby theloneCPRproviderbeforegettinghelp,mayimproveoutcome forvictimsofdrowning.Thismodificationshouldbetaughtonly tothosewhohaveaspecificdutyofcaretopotentialdrowning victims(e.g.lifeguards).
Collaborators
LeoL.Bossaert,UniversityofAntwerp,Antwerp,Belgium,
AntonioCaballero,EmergencyDepartment,HospitalUniversitario VirgendelRocío,Sevilla,Spain,
PascalCassan,GlobalFirstAidReferenceCentre,International Fed-erationofRedCrossandRedCrescent,Paris,France,
CristinaGranja,EmergencyandIntensiveCareDepartment, Hospi-taldeFaro,CentroHospitalardoAlgarve,Porto,Portugal,
Claudio Sandroni, Department of Anaesthesiologyand Intensive Care,CatholicUniversitySchoolofMedicine,Rome,Italy,
DavidA.Zideman,ImperialCollegeHealthcareNHSTrust,London, UK,
Jerry P. Nolan, Department of Anaesthesia and Intensive Care Medicine,RoyalUnitedHospital,Bath,UK,
IanMaconochie, PaediatricEmergency Medicine and NIHR BRC, ImperialCollege,London,UK,
RobertGreif,Department ofAnaesthesiologyandPainMedicine, UniversityHospitalBernandUniversityBern,Bern,Switzerland.
Conflictsofinterest
GavinD.Perkins EditorResuscitation JasmeetSoar EditorResuscitation
AnthonyJ.Handley MedicaladvisorBA,Virgin,Placesfor people,LifesavingSocieties,Trading CompanySecretaryRCUK
GiuseppeRistagno ExpertadviceZOLL:ECGinterpretation MaaretCastren MedicaladvisoryBoardFalckFoundation RudolphW.Koster MedicaladvisorPhysioControland
HeartSine,ResearchgrantsPhysioControl, Philips,Zoll,CardiacScience,Defibtech, Jolife
VolkerWenzel Researchgrants,Medicaladvisor,Speakers honorarium“AOPOrphan”Pharma Jan-ThorstenGräsner Noconflictofinterestreported KoenraadG.Monsieurs Noconflictofinterestreported MichaelA.Smyth Noconflictofinterestreported TheresaMarieroOlasveengen Noconflictofinterestreported ViolettaRaffay Noconflictofinterestreported
linesforresuscitation2015section3adultadvancedlifesupport.Resuscitation 2015;95:99–146.
2.ZidemanDA, De Buck EDJ, Singletary EM, etal. EuropeanResuscitation Councilguidelinesforresuscitation2015section9firstaid.Resuscitation 2015;95:277–86.
3.PerkinsGD,TraversAH,ConsidineJ,etal.Part3:Adultbasiclifesupport andautomatedexternaldefibrillation:2015InternationalConsensuson Car-diopulmonaryResuscitationandEmergencyCardiovascularCareScienceWith TreatmentRecommendations.Resuscitation2015;95:e43–70.
4.BerdowskiJ,BergRA,TijssenJG,KosterRW.Globalincidencesof out-of-hospitalcardiacarrestandsurvivalrates:systematicreviewof67prospective studies.Resuscitation2010;81:1479–87.
5.GrasnerJT,HerlitzJ,KosterRW,Rosell-OrtizF,StamatakisL,BossaertL. Qual-itymanagementinresuscitation–towardsaEuropeancardiacarrestregistry (EuReCa).Resuscitation2011;82:989–94.
6.GrasnerJT,BossaertL.Epidemiologyandmanagementofcardiacarrest:what registriesarerevealing.BestPractResClinAnaesthesiol2013;27:293–306. 7.CobbLA,FahrenbruchCE,OlsufkaM,CopassMK.Changingincidenceof
out-of-hospitalventricularfibrillation,1980–2000.JAMA2002;288:3008–13. 8.ReaTD,PearceRM,RaghunathanTE,etal.Incidenceofout-of-hospitalcardiac
arrest.AmJCardiol2004;93:1455–60.
9.VaillancourtC,Verma A,TrickettJ, etal. Evaluatingthe effectivenessof dispatch-assistedcardiopulmonary resuscitationinstructions. Acad Emerg Med2007;14:877–83.
10.Agarwal DA, Hess EP, Atkinson EJ, White RD. Ventricular fibrilla-tion in Rochester, Minnesota: experience over 18 years. Resuscitation 2009;80:1253–8.
11.RinghM,HerlitzJ,HollenbergJ,RosenqvistM,SvenssonL.Outofhospital car-diacarrestoutsidehomeinSweden,changeincharacteristics,outcomeand availabilityforpublicaccessdefibrillation.ScandJTraumaResuscEmergMed 2009;17:18.
12.Hulleman M,Berdowski J, de Groot JR,et al. Implantable cardioverter-defibrillatorshavereducedtheincidenceofresuscitationforout-of-hospital cardiacarrestcausedbylethalarrhythmias.Circulation2012;126:815–21. 13.BlomMT,BeesemsSG,HommaPC,etal. Improvedsurvivalafter
out-of-hospitalcardiacarrestanduseofautomatedexternaldefibrillators.Circulation 2014;130:1868–75.
14.CumminsR,ThiesW.AutomatedexternaldefibrillatorsandtheAdvanced CardiacLifeSupportProgram:anewinitiativefromtheAmericanHeart Asso-ciation.AmJEmergMed1991;9:91–3.
15.WaalewijnRA,NijpelsMA,TijssenJG,KosterRW.Preventionofdeterioration ofventricularfibrillationbybasiclifesupportduringout-of-hospitalcardiac arrest.Resuscitation2002;54:31–6.
16.WeisfeldtML,SitlaniCM,OrnatoJP,etal.Survivalafterapplicationof auto-maticexternaldefibrillatorsbeforearrivaloftheemergencymedicalsystem: evaluationintheresuscitationoutcomesconsortiumpopulationof21million. JAmCollCardiol2010;55:1713–20.
17.BerdowskiJ,BlomMT,BardaiA,TanHL,TijssenJG,KosterRW.Impactofonsite ordispatchedautomatedexternaldefibrillatoruseonsurvivalafter out-of-hospitalcardiacarrest.Circulation2011;124:2225–32.
18.NolanJ,SoarJ,EikelandH.Thechainofsurvival.Resuscitation2006;71:270–1. 19.MullerD,AgrawalR,ArntzHR.Howsuddenissuddencardiacdeath?
Circula-tion2006;114:1146–50.
20.WaalewijnRA,TijssenJG,KosterRW.Bystanderinitiatedactionsin out-of-hospital cardiopulmonary resuscitation: results from the Amsterdam ResuscitationStudy(ARRESUST).Resuscitation2001;50:273–9.
21.SassonC,RogersMA,DahlJ,KellermannAL.Predictorsofsurvivalfrom out-of-hospitalcardiacarrest:asystematicreviewandmeta-analysis.CircCardiovasc QualOutcomes2010;3:63–81.
22.NehmeZ, AndrewE, Bernard S,Smith K.Comparisonof out-of-hospital cardiacarrestoccurringbeforeandafterparamedicarrival:epidemiology, sur-vivaltohospitaldischargeand12-monthfunctionalrecovery.Resuscitation 2015;89:50–7.
23.TakeiY,NishiT,KamikuraT,etal.Doearlyemergencycallsbeforepatient collapseimprovesurvivalafterout-of-hospitalcardiacarrests?Resuscitation 2015;88:20–7.
24.ValenzuelaTD,RoeDJ,CretinS,SpaiteDW,LarsenMP.Estimatingeffectiveness ofcardiacarrestinterventions:alogisticregressionsurvivalmodel.Circulation 1997;96:3308–13.
25.HolmbergM,HolmbergS,HerlitzJ,GardelovB.Survivalaftercardiacarrest outsidehospitalinSweden.SwedishCardiacArrestRegistry.Resuscitation 1998;36:29–36.
26.HolmbergM,HolmbergS,HerlitzJ.Factorsmodifyingtheeffectofbystander cardiopulmonaryresuscitationonsurvivalinout-of-hospitalcardiacarrest patientsinSweden.EurHeartJ2001;22:511–9.
27.WissenbergM,LippertFK,FolkeF,etal.Associationofnationalinitiativesto improvecardiacarrestmanagementwithratesofbystanderinterventionand patientsurvivalafterout-of-hospitalcardiacarrest.JAMA2013;310:1377–84. 28.Hasselqvist-AxI,RivaG,HerlitzJ,etal.Earlycardiopulmonaryresuscitationin
out-of-hospitalcardiacarrest.NEnglJMed2015;372:2307–15.
29.ReaTD,FahrenbruchC,CulleyL,etal.CPRwithchestcompresssionsaloneor withrescuebreathing.NEnglJMed2010;363:423–33.
diopulmonaryresuscitation:ameta-analysis.Lancet2010;376:1552–7. 32.ValenzuelaTD,RoeDJ,NicholG,ClarkLL,SpaiteDW,HardmanRG.Outcomes
ofrapiddefibrillationbysecurityofficersaftercardiacarrestincasinos.NEngl JMed2000;343:1206–9.
33.RinghM,RosenqvistM,HollenbergJ,etal.Mobile-phonedispatchoflaypersons forCPRinout-of-hospitalcardiacarrest.NEnglJMed2015;372:2316–25. 34.LarsenMP,EisenbergMS,CumminsRO,HallstromAP.Predictingsurvival
from out-of-hospital cardiac arrest: a graphic model. Ann Emerg Med 1993;22:1652–8.
35.NolanJP,SoarJ,CariouA,etal.EuropeanResuscitationCouncilandEuropean SocietyofIntensiveCareMedicineGuidelinesforPost-resuscitationCare2015. Section5Post-resuscitationcare.Resuscitation2015;95:201–21.
36.vanAlemAP,VrenkenRH,deVosR,TijssenJG,KosterRW.Useof auto-matedexternaldefibrillatorbyfirstrespondersinoutofhospitalcardiacarrest: prospectivecontrolledtrial.BrMedJ2003;327:1312.
37.FothergillRT,WatsonLR,ChamberlainD,VirdiGK,MooreFP,WhitbreadM. Increasesinsurvivalfromout-of-hospitalcardiacarrest:afiveyearstudy. Resuscitation2013;84:1089–92.
38.PerkinsGD,LallR,QuinnT,etal.Mechanical versusmanualchest com-pressionforout-of-hospitalcardiacarrest(PARAMEDIC):apragmatic,cluster randomisedcontrolledtrial.Lancet2015;385:947–55.
39.WeisfeldtML,BeckerLB.Resuscitationaftercardiacarrest:a3-phase time-sensitivemodel.JAMA2002;288:3035–8.
40.ZijlstraJA,StieglisR,RiedijkF,SmeekesM,vanderWorpWE,KosterRW. LocallayrescuerswithAEDs,alertedbytextmessages,contributetoearly defibrillationinaDutchout-of-hospitalcardiacarrestdispatchsystem. Resus-citation2014;85:1444–9.
41.KerberRE,BeckerLB,BourlandJD,etal.Automaticexternaldefibrillatorsfor publicaccessdefibrillation:recommendationsforspecifyingandreporting arrhythmiaanalysisalgorithmperformance,incorporatingnewwaveforms, andenhancingsafety.AstatementforhealthprofessionalsfromtheAmerican HeartAssociationTaskForceonAutomaticExternalDefibrillation, Subcom-mitteeonAEDSafetyandEfficacy.Circulation1997;95:1677–82.
42.CallePA,MpotosN,CalleSP,MonsieursKG.Inaccuratetreatmentdecisionsof automatedexternaldefibrillatorsusedbyemergencymedicalservices person-nel:incidence,causeandimpactonoutcome.Resuscitation2015;88:68–74. 43.BahrJ,KlinglerH,PanzerW,RodeH,KettlerD.Skillsoflaypeopleinchecking
thecarotidpulse.Resuscitation1997;35:23–6.
44.NymanJ,SihvonenM.Cardiopulmonaryresuscitationskillsinnursesand nurs-ingstudents.Resuscitation2000;47:179–84.
45.TibballsJ,RussellP.Reliabilityofpulsepalpationbyhealthcarepersonnelto diagnosepaediatriccardiacarrest.Resuscitation2009;80:61–4.
46.TibballsJ,WeeranatnaC.Theinfluenceoftimeontheaccuracyofhealthcare personneltodiagnosepaediatriccardiacarrestbypulsepalpation. Resuscita-tion2010;81:671–5.
47.MouleP.Checkingthecarotidpulse:diagnosticaccuracyinstudentsofthe healthcareprofessions.Resuscitation2000;44:195–201.
48.BobrowBJ,Zuercher M,EwyGA, etal. Gaspingduringcardiacarrestin humans is frequent and associated with improved survival. Circulation 2008;118:2550–4.
49.PerkinsGD,StephensonB,HulmeJ,MonsieursKG.Birminghamassessmentof breathingstudy(BABS).Resuscitation2005;64:109–13.
50.PerkinsGD,WalkerG,ChristensenK,HulmeJ,MonsieursKG.Teaching recog-nitionofagonalbreathingimprovesaccuracyofdiagnosingcardiacarrest. Resuscitation2006;70:432–7.
51.BreckwoldtJ,SchloesserS,ArntzHR.Perceptionsofcollapseandassessmentof cardiacarrestbybystandersofout-of-hospitalcardiacarrest(OOHCA). Resus-citation2009;80:1108–13.
52.SteckerEC,ReinierK,Uy-EvanadoA,etal.Relationship betweenseizure episodeandsuddencardiacarrestinpatientswithepilepsy:a community-basedstudy.CircArrhythmElectrophysiol2013;6:912–6.
53.KuismaM,BoydJ,VayrynenT,RepoJ,Nousila-WiikM,HolmstromP. Emer-gencycallprocessingandsurvivalfromout-of-hospitalventricularfibrillation. Resuscitation2005;67:89–93.
54.BerdowskiJ,BeekhuisF,ZwindermanAH,TijssenJG,KosterRW.Importanceof thefirstlink:descriptionandrecognitionofanout-of-hospitalcardiacarrest inanemergencycall.Circulation2009;119:2096–102.
55.HewardA,DamianiM,Hartley-SharpeC.DoestheuseoftheAdvanced Med-icalPriorityDispatchSystemaffectcardiacarrestdetection?EmergMedJ 2004;21:115–8.
56.EisenbergMS,HallstromAP,CarterWB,CumminsRO,BergnerL,PierceJ. Emer-gencyCPRinstructionviatelephone.AmJPublicHealth1985;75:47–50. 57.StipulanteS,TubesR,ElFassiM,etal.ImplementationoftheALERTalgorithm,a
newdispatcher-assistedtelephonecardiopulmonaryresuscitationprotocol,in non-AdvancedMedicalPriorityDispatchSystem(AMPDS)EmergencyMedical Servicescentres.Resuscitation2014;85:177–81.
58.CastrenM, Kuisma M,Serlachius J, Skrifvars M.Do health care profes-sionals report sudden cardiac arrest better than laymen? Resuscitation 2001;51:265–8.
59.HallstromAP, Cobb LA,JohnsonE, CopassMK.Dispatcher assisted CPR: implementation and potential benefit. A 12-year study. Resuscitation 2003;57:123–9.