TECHNICAL NOTES
Transvenous Biopsy of Cavo-Atrial Tumors with the Quick-Core
Needle
Lukas Hechelhammer,
1Thomas Schertler,
1Jo¨rg D. Seebach,
2Michael O. Kurrer,
3Borut Marincek,
1Thomas Pfammatter
11Institute of Diagnostic Radiology, University Hospital, Zu¨rich, Switzerland 2Department of Internal Medicine, University Hospital, Zu¨rich, Switzerland 3Institute of Diagnostic Pathology, University Hospital, Zu¨rich, Switzerland
Abstract
A variant application of the renal Quick-Core needle in 3 patients with cavo-atrial tumors is reported. In all 3 patients either a tran-sjugular or transfemoral venous biopsy approach with this device yielded sufficient tissue for histological diagnosis at the first at-tempt. Bioptic diagnoses were confirmed either by surgery or radiological and clinical response to a specific chemotherapy. There were no procedure-related complications.
Key words: Cavo-atrial tumor—Transvenous biopsy—Quick-Core
needle
The differential diagnosis of masses extending from the superior or inferior vena cava to the right atrium or vice versa includes benign conditions such as thrombus or myxoma as well as primary or secondary malignant neoplasms of the vena cava or the heart [1]. Although CT- or MR-imaging and echocardiography provide ac-curate assessment of the size, location and point of attachment of these tumors, tissue characterization is not possible [2, 3]. There-fore, a variety of transluminal techniques such as forceps biopsy [4, 5], brushing [6], aspiration [7, 8] or scoop biopsy [9] have been utilized to obtain tissue for histological or cytological examination of cavo-atrial tumors. However, there are several known causes of erroneous or non-diagnostic samplings associated with some of these techniques including superficial apposition clots, low cellu-larity of the lesion or crushing artefacts.
A high diagnostic yield combined with a low complication rate has been repeatedly reported for transjugular liver or kidney biop-sies using a specifically designed automated tru-cut needle (Quick-Core Liver or Kidney Access and Biopsy Set, Cook Europe, Bjaeverskov, Denmark) [10 –13].
Biopsy with this device achieved a high diagnostic yield due to better tissue penetration and an excellent specimen quality. Accord-ingly, we used the same transvenous Quick-Core needle to establish a diagnosis in 3 patients with cavo-atrial tumors. Bioptic diagnoses
were confirmed by surgery in 2 patients and by the response to a specific chemotherapy in the third patient.
Case 1
A 76-year-old woman with a history of an intraocular B-cell-lymphoma presented with a 2-month history of night sweat, loss of appetite and weakness. The chest CT showed a mass within the superior vena cava and the right atrial cavity (Fig. 1). To exclude a secondary neoplasm, a biopsy was performed. After local anesthesia, the right internal jugular vein was punctured and a 9-French sheath was introduced. A superior cavogram was obtained with a pigtail catheter in two planes to guide fluoroscopy-guided biopsy using soft tissue and bony landmarks. The next steps of the proce-dure were the same for all patients. The diagnostic pigtail catheter was removed over a 0.035” stiff guidewire (Amplatz stiff wire guide). Then, the angled 14-gauge metallic guiding cannula was assembled with the 7-French outer protection sheath of the biopsy set and introduced over the guidewire. After bringing the sheated cannula into the desired position, the guidewire was withdrawn. The final location was fluoroscopically confirmed by con-trast injection through the cannula. Finally, the transjugular renal Quick-Core needle (Cook Europe, Bjaeverskov, Denmark), which is a 19-gauge, blunt-tipped tru-cut needle with a 2 cm throw length, was advanced through the cannula. In this case, two passes were performed, obtaining 3 tissue cores with a maximal length of 11 mm. The histology confirmed a relapse of the non-Hodgkin’s lymphoma. Chemotherapy with cyclophosphamid, vincristin, doxorubicin and prednison was started, leading to rapid clinical and radiological improvement.
Case 2
A 51-year-old woman with a history of a breast carcinoma and left nephrec-tomy for trauma presented with retrosternal pressure lasting for one year. After cardiac causes were ruled out, a chest CT was performed to exclude pulmonary embolism. Surprisingly, a mass expanding from the hepatic vena cava segment to the right atrium was found but no evidence of pulmonary emboli. Gadolinium-enhanced magnetic resonance imaging showed a lob-ular tumor which seemed to either infiltrate locally or originate from the dorsal caval wall at the level of the uncinate processus of the pancreas. To plan further treatment, a transvenous biopsy was performed.
Right transfemoral venous access was chosen, as we felt the attachment point was next to the pancreas, in order to reduce tumor manipulation and avoid biopsy of a possible apposition clot. After local anesthesia, a 9-French sheath was introduced, a 5-French pigtail catheter was advanced into the inferior vena cava and a digital subtraction cavography was performed in 2 planes. Attention was paid to obtain also the intravenous digital subtraction
Correspondence to: T. Pfammatter, M.D.
C
ardio
V
ascular
and
I
nterventional
R
adiology
© Springer-Verlag New York, LLC. 2004 Cardiovasc Intervent Radiol (2004) 27:251–253
arteriogram for renal artery localization in order to avoid inadvertent renal arterial puncture (Fig. 2). The cavogram showed filling defects beginning at the level of the right renal vein reaching into the right atrium. Under fluoroscopic guidance the renal Quick-Core needle was easily steered trans-femorally to the tumor, using bony landmarks and contrast. Three passes were performed, yielding tissue cores with a maximal length of 8 mm. Histological examination of the biopsy revealed a highly differentiated leiomyosarcoma. A diagnosis which was confirmed histologically after resection of the tumor.
Case 3
A 75-year-old woman presented with a 8-month history of dyspnea and signs of a superior vena cava syndrome. CT scanning demonstrated on occlusive tumor in the superior vena cava in continuity with a right atrial
intracavitary mass and evidence of acute pulmonary embolism. The echo-cardiographical findings were atypical for an atrial myxoma leading to superior caval thrombosis, therefore a preoperative biopsy was requested.
As both innominate veins were occluded, a transfemoral route was selected. The right atriogram showed a lobular spherical mass attached to the mouth of the superior vena cava. Visualization of the mass under fluoroscopy was facilitated by the pooling of the contrast agent in the corrugated tumor surface (Fig. 3). Using a hepatic 18-gauge Quick Core needle, two passes were performed. After removal the Quick Core Needle was replaced by an endomyocardial biopsy forceps (5.5 Fr), Cordis, Miami, FL, USA) and 2 additional biopsy specimens were obtained. The Quick-Core-specimen had a maximal length of 12 mm whereas the forceps specimen was only 3 mm in the biggest dimension. In contrast to the forceps specimen showing fibrin with a few dispersed cells of an adenocarcinoma,
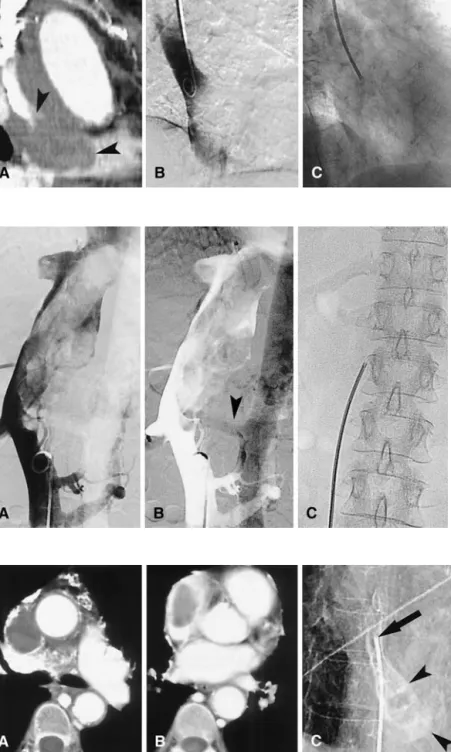
Fig. 1. Case 1. Sagittal reconstruction of the
cardiac multidetector-row CT showing mass protruding into the right atrial cavity (arrowheads) (A). Corresponding venogram with a pigtail catheter in the superior vena cava (B). Transjugular biopsy guiding cannula directed anteriorly towards the mass (C). Histology revealed non-Hodgkin’s lymphoma.
Fig. 2. Case 2. Digital subtraction cavogram
demonstrates expansile filling defect in the suprarenal segment (A). In the late phase the aorta and right renal artery (arrowhead) are opacified. The left kidney had been removed years before because of trauma (B). Transfemorally inserted 14-gauge angulated stiffening cannula providing directional control. The coaxially passed Quick-Core needle is not seen (C). Histology revealed highly differentiated leiomyosarcoma.
Fig. 3. Case 3. Transversal CT scan at the
aortic root showing an occlusion of the superior vena cava (A). The homogeneous nonenhancing mass extends into the right atrium (B). Cine-spot-image after atriography with intracavitary floating mass (arrowheads) and tip of transfemorally inserted biopsy cannula at the attachment of the mass (arrow)
(C). Histology revealed adenocarcinoma.
in the tru-cut biopsy specimen cardial myocytes with bands of loose con-nective tissue were also visible by light microscopy. A day after the procedure the patient complained of right shoulder pain and paresis of the right arm and a destructive process in the fifth cervical vertebral body with compression of the medulla was demonstrated by a CT of the neck. A surgical resection of the cavo-atrial tumor and the cervical metastasis was performed, and, the operative specimen confirmed the diagnosis of an adenocarcinoma.
The patient died 3 weeks later, and postmortem examination revealed a 0.4 cm pancreatic adenocarcinoma which most likely represented the origin of the metastatic disease.
The coagulation parameters for all 3 patients were within normal limits. There were no biopsy-related complications immediately after the proce-dure and during the following time of hospital stay. The Institutional Review Board did not require approval for the procedure.
Discussion
High diagnostic yield, ease of the procedure, cost-effectiveness and safety are important determinants of any biopsy technique. Al-though cavo-atrial tumors are rare, a variety of biopsy techniques ranging from percutaneous CT-guided fine needle aspiration to more complex procedures such as transesophageal echocardio-graphically-guided transfemoral forceps biopsy have been de-scribed [8, 14]. As the pertinent literature consists mostly of case reports, no conclusion can be drawn regarding the technique that should be chosen for cavo-atrial tumors. Moreover, as these tumors are often coated with appositional clots, a false-positive diagnosis of thrombus may mask an underlying malignant tumor [6, 9, 15, 16]. To our knowledge, transcaval biopsy of an inferior vena caval tumor was first reported in 1972 using a gastroscopic biopsy for-ceps [4]. A complication rate of 6% and a mortality rate of 0.3% has been reported for transvenous right ventricular endomyocardial forceps biopsy in a large series of patients with cardiomyopathy [17]. Myocardiac perforation resulting in tamponade was the cause of biopsy-related death in 2 cases. Therefore, procedures yielding even larger samples such as the Quick-Core needle require good steerability to minimize complications due to unintentional perfo-ration of the vena cava or the right atrium. Successful transjugular Quick-Core biopsy of an inferior vena caval tumor has been de-scribed in a single case [18]. In our experience the Quick-Core needle could be directed equally well from a jugular or femoral venous access towards the desired cavo-atrial biopsy site. The angulation of the tru-cut needle can be modified by bending or straightening the metallic guiding cannula. The modifications made by the manufacturer to adapt the liver system for renal biopsies (19-gauge, blunt-tip) may further reduce possible complications.
A small risk of tumor cell seeding is inherent to any tumor manipulation including biopsies. However, as tissue specimens are encapsulated at withdrawal the probability of tissue embolization might even be lower using the Quick-Core needle in comparison to forceps-assisted procedures.
The biopsies obtained with the Quick-Core needle reported here in 3 cases of cavo-atrial tumors contained sufficient tissue for histological diagnosis at the first attempt. Consequently thoracot-omy, which hitherto was performed for diagnosis of cardiac non-Hodgkin’s lymphoma, could have been be avoided in case 1 [19]. Further, retrospectively, thoracotomy should also have been de-ferred in the patient with metastatic adenocarcinoma of unknown
origin (Case 3) in the light of the transvenous Quick-Core biopsy result.
In conclusion, there were no biopsy-related complications in 3 consecutive cases of cavo-atrial tumors of unknown origin. The histological results of the biopsies were essential to the establish-ment of a diagnosis and influenced treatestablish-ment. Therefore, our lim-ited experience suggests that transfemoral or transjugular biopsies using a Quick-Core needle represent a safe, expeditious and reliable sampling procedure for cavo-atrial tumors.
References
1. Burke A, Virmani R (1996) Tumors of the heart and great vessels. In: Atlas of tumor pathology, 3rd series, fasc 16. Washington DC. Armed Forces Institute of Pathology 1–11, 221–223
2. Grebenc ML, Rosado-de-Christenson ML, Green CE, et al. (2002) Cardiac myxoma: imaging features in 83 patients. Radiographics 22(3): 673– 689
3. Blum U, Wildanger G, Windfuhr M, et al. (1995) Preoperative CT and MR imaging of inferior vena cava leiomyosarcoma. Eur J Radiol 20(1):23–27
4. Robins JM, Bookstein JJ (1972) Percutaneous transcaval biopsy tech-nique in the evaluation of inferior vena cava occlusion. Radiology 105(2):451– 452
5. Adachi K, Tanaka H, Toshima H, et al. (1988) Right atrial angiosar-coma diagnosed by cardiac biopsy. Am Heart J 115(2):482– 485 6. Mills SR, Doppman JL, Head GL, et al. (1978) Transcatheter brush
biopsy of intravenous tumor thrombi. Radiology 127(3):667– 670 7. Wendth AJ Jr., Garlick WB, Pantoja GE, et al. (1976) Transcatheter
biopsy of renal carcinoma invading the inferior vena cava. J Urol 115(3):331–332
8. Moriarty AT, Nelson WA, McGahey B (1990) Fine needle aspiration of rhabdomyosarcoma of the heart. Light and electron microscopic find-ings and histologic correlation. Acta Cytol 34(1):74 –78
9. Kishi K, Sonomura T, Terada M, et al. (1997) Scoop biopsy of intra-caval tumor thrombi: a preliminary report of a minimally invasive technique to obtain large samples. Eur J Radiol 24(3):263–268 10. Little AF, Zajko AB, Orons PD (1996) Transjugular liver biopsy: a
prospective study in 43 patients with the Quick-Core biopsy needle. J Vasc Interv Radiol 7(1):127–131
11. Banares R, Alonso S, Catalina MV, et al. (2001) Randomized con-trolled trial of aspiration needle versus automated biopsy device for transjugular liver biopsy. J Vasc Interv Radiol 12(5):583–587 12. Cluzel P, Martinez F, Bellin MF, et al. (2000) Transjugular versus
percutaneous renal biopsy for the diagnosis of parenchymal disease: comparison of sampling effectiveness and complications. Radiology 215(3):689 – 693
13. Sofocleous CT, Bahramipour P, Mele C, et al. (2002) Transvenous transjugular renal core biopsy with a redesigned biopsy set including a blunt-tipped needle. Cardiovasc Intervent Radiol 25(2):155–157 14. Rubin DC, Ziskind AA, Hawke MW, et al. (1994) Transesophageal
echocardiographically guided percutaneous biopsy of a right atrial cardiac mass. Am Heart J 127(4 Pt 1):935–936
15. Nitta R, Sakomura Y, Tanimoto K, et al. (1998) Primary cardiac angiosarcoma of the right atrium undiagnosed by transvenous endocar-dial tumor biopsy. Intern Med 37(12):1023–1026
16. Withers CE, Casola G, Herba MJ, et al. (1988) Intravascular tumors: transvenous biopsy. Radiology 167(3):713–715
17. Deckers JW, Hare JM, Baughman KL (1992) Complications of trans-venous right ventricular endomyocardial biopsy in adult patients with cardiomyopathy: a seven-year survey of 546 consecutive diagnostic procedures in a tertiary referral center. J Am Coll Cardiol 19(1):43– 47 18. D’Altorio RA, Elliott JZ, Reiser M, et al. (2001) Transjugular biopsy of
inferior vena caval tumor. J Urol 165(6 Pt 1):1988 –1989
19. Chalabreysse L, Berger F, Loire R, et al. (2002) Primary cardiac lymphoma in immunocompetent patients: a report of three cases and review of the literature. Virchows Arch 441(5):456 – 461