M E T H O D O L O G Y
Open Access
The effectiveness of scoliosis screening programs:
methods for systematic review and expert panel
recommendations formulation
Marie Beauséjour
1,2*, Lise Goulet
2, Stefan Parent
1,3, Debbie Ehrmann Feldman
2, Isabelle Turgeon
1,
Marjolaine Roy-Beaudry
1, Jose Felix Sosa
1, Hubert Labelle
1,3and Members of the Quebec Scoliosis Society and of
the Canadian Paediatric Spinal Deformities Study Group
Abstract
Background: Literature on scoliosis screening is vast, however because of the observational nature of available data and methodological flaws, data interpretation is often complex, leading to incomplete and sometimes, somewhat misleading conclusions. The need to propose a set of methods for critical appraisal of the literature about scoliosis screening, a comprehensive summary and rating of the available evidence appeared essential. Methods: To address these gaps, the study aims were: i) To propose a framework for the assessment of published studies on scoliosis screening effectiveness; ii) To suggest specific questions to be answered on screening
effectiveness instead of trying to reach a global position for or against the programs; iii) To contextualize the knowledge through expert panel consultation and meaningful recommendations. The general methodological approach proceeds through the following steps: Elaboration of the conceptual framework; Formulation of the review questions; Identification of the criteria for the review; Selection of the studies; Critical assessment of the studies; Results synthesis; Formulation and grading of recommendations in response to the questions. This plan follows at best GRADE Group (Grades of Recommendation, Assessment, Development and Evaluation) requirements for systematic reviews, assessing quality of evidence and grading the strength of recommendations.
Conclusions: In this article, the methods developed in support of this work are presented since they may be of some interest for similar reviews in scoliosis and orthopaedic fields.
Keywords: Scoliosis, Mass screening, Adolescent, Program evaluation, Systematic review Background
The value of scoliosis screening programs was often de-bated and is still a controversial issue as indicated by the SOSORT 2007 positional statement, Plaszewski’s 2012 review and 2012 historical article by Linker [1-3]. In most cases, scoliosis screening was achieved through mass systematic examination of children, in the school environment, searching for back asymmetries. These programs are still in operation in some countries but
were discontinued in many others since the 1980s. Indeed, the British, American and Canadian Preventive task forces, who based their decisions on the best available evidence at the time, did not recommend the use of these programs. The two main issues raised by the Canadian task force were the ability of the detection procedure to detect the condition and the ability of the available treatment inter-vention to achieve a favourable outcome [4,5].
In 1993, the United States Preventive Services Task Force concluded that there was insufficient evidence to recommend for, or against, screening but, in 2004, it recommended against the routine screening for AIS, and maintained this position [6] despite its continuing support from medical bodies (American Academy of Orthopedic Surgeons, Scoliosis Research Society, Pediatric
* Correspondence:marie.beausejour@umontreal.ca
1Sainte-Justine University Hospital Center, Unité de recherche clinique en
orthopédie, 3175 Chemin Côte-Sainte-Catherine, Montréal, Québec H3T 1C5, Canada
2
School of Public Health, Université de Montréal, 7101 Avenue du Parc, 3rd floor, Montréal, Québec H3N 1X9, Canada
Full list of author information is available at the end of the article
© 2013 Beauséjour et al.; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Orthopedic Society of North America and American Academy of Pediatrics) and other interest groups [7]. The Canadian position (2003) is that insufficient evidence exists for a recommendation to be made [8].
Literature on scoliosis screening is vast. There are a few reviews and expert opinion papers, guiding the re-flection on the clinical benefits of such initiatives and also, possible burden and societal costs of the programs [9-12] However, published studies consist of mainly prevalence studies or reports on screening programs set-up and process with very few controlled trials and com-parative studies.
A meta-analysis published by Fong et al. [13] has shed light on the clinical effectiveness of scoliosis screening programs. This rigorous review focused on scoliosis prevalence, referral rates and positive predictive values of the tests as main outcomes, from 36 published
retrospective cohort studies. However, other dimensions of effectiveness should also be considered to get a more complete assessment. Sabirin et al. [14] conducted a sys-tematic review that was an interesting attempt to widen the scope of previous reviews by exploring four themes: effectiveness of scoliosis detection, consequences on sur-gical treatment, cost/cost-effectiveness and diagnostic accuracy. However, the review could have been more ex-tensive in terms of included studies and assessment of the study quality.
Because of the paucity of controlled trials in this field, the observational nature of available data and methodo-logical flaws, data interpretation is often complex, with the inherent risk of leading to incomplete and even mis-leading conclusions.
The need to propose a set of methods for critical appraisal of the literature about scoliosis screening, a
Formulation of the main research question
Selection of studies
Elaboration of the conceptual framework
Formulation of specific review questions
Definition of search criteria
Critical assessment of individual studies
Grading of the body of evidence (outcome-based quality assessment)
Preparation of Summary of Evidence (SoE) Tables
Formulation of conclusive statements on each question
Presentation of SoE Tables & statements to expert panel
Discussion and revision of the statements
Experts voting
Experts consensus
Final list of statements & grading of recommendations Yes
No
comprehensive summary and rating of the available evi-dence appeared essential. More specifically, our objec-tives were:
i) To propose a framework for the assessment of published studies on scoliosis screening effectiveness; ii) To suggest specific questions to be answered on
screening effectiveness instead of trying to reach a global position for or against the programs;
iii) To contextualize the knowledge through expert panel consultation and meaningful recommendations.
Methods
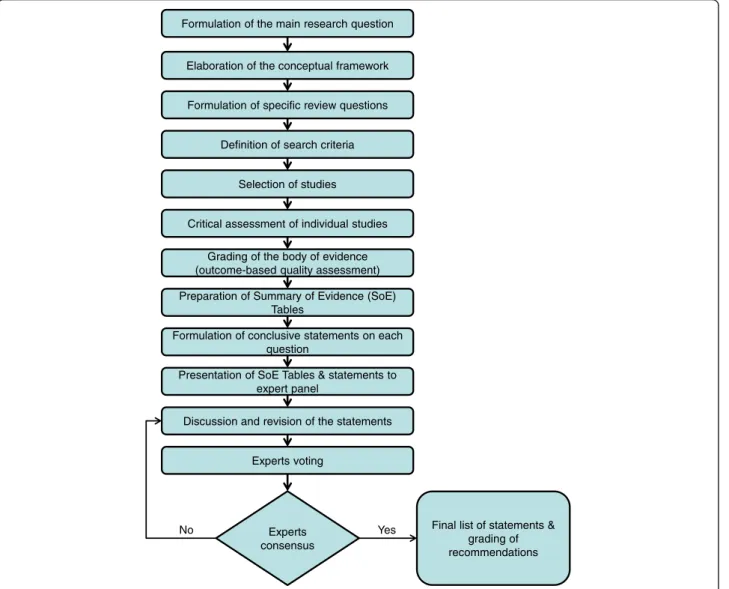
The general methodological approach proceeded through the following steps (Figure 1):
a) Elaboration of the conceptual framework; b) Formulation of the review questions; c) Identification of the criteria for the review; d) Selection of the studies;
e) Critical assessment of the studies; f ) Results synthesis;
g) Formulation and grading of recommendations in response to the questions.
This plan follows the GRADE Group (Grades of Recom-mendation, Assessment, Development and Evaluation) re-quirements for systematic reviews, assessing quality of evidence and grading of the strength of recommendations [15-17]. Some modifications to the tools were proposed because of the specific study context and available ma-terial but also in consideration of our capabilities as a research team and preferences of the involved experts. The intention was not to modify the GRADE approach (adopted by the Cochrane Collaboration [18]), that has proven its worth and usefulness, but, to describe, in our desire to stay as close to it as possible, the encountered
difficulties and alternative ways to proceed. The review protocol was developed in such a way to enable the au-thors to follow the PRISMA statement when reporting the review methodologies and results [19].
a) The conceptual framework
The main research question of the review was: What is the evidence in the literature on the effectiveness of
scoliosis screening programs in the adolescent
population?
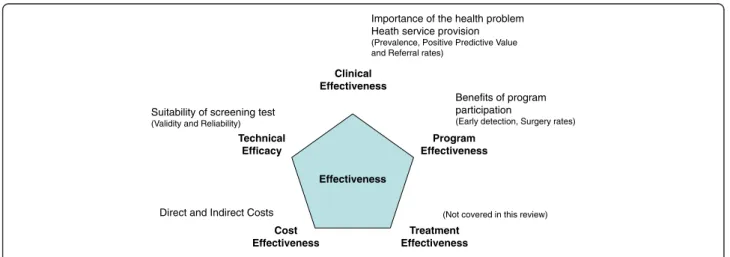
To conceptually define Effectiveness, we relied on Last’s definitions of Efficacy and Effectiveness. According to Last, Effectiveness is “the extent to which a medical intervention does what it is supposed to do”. In contrast, Efficacy concerns “the extent to which an intervention produces benefits under ideal circumstances” [20,21]. We referred to the classical Wilson and Jungner criteria for the appraisal of screening programs [22] and the reviewed criteria by the UK National Screening Commit-tee [23] to define five main dimensions of effectiveness: Technical Efficacy relates to the validity and reliability of the tests; Clinical Effectiveness describes the importance of the health problem and the consequences of screening on patient management and the health system; Treat-ment Effectiveness concerns the benefits for the patients of the available treatment modalities; Program Effective-ness refers to the benefits for the patients who adhere to the screening programs, and these benefits are balanced against costs for the society in Cost-Effectiveness. These dimensions are evaluated under regular practice circum-stances, except for Technical Efficacy which may be evaluated under experimental protocols on selected sam-ples of participants. Our conceptual framework of Effect-iveness is depicted in Figure 2.
This conceptual model was a posteriori empirically supported by the findings of what was actually available in the literature in this field.
Effectiveness Clinical Effectiveness Technical Efficacy Cost Effectiveness Program Effectiveness Treatment Effectiveness
Importance of the health problem Heath service provision
(Prevalence, Positive Predictive Value and Referral rates)
Benefits of program participation
(Early detection, Surgery rates)
(Not covered in this review)
Suitability of screening test
(Validity and Reliability)
Direct and Indirect Costs
It is important to mention that the assessment of Treatment Effectiveness, which would have been the 5th dimension of effectiveness to be considered based on the model, was not completed in this review. Even though the existence of an effective treatment is of capital im-portance in the decision to screen or not for the disease of interest, the authors considered that this topic would necessitate a systematic review on its own. Despite the need for such an evaluation [24], in the specific context of this review, it was decided to focus solely on the screening process.
b) Research questions
Seven specific questions were addressed, in relation to the main dimensions of effectiveness that were covered. The following questions were originally de-rived by the authors and were elaborated in corres-pondence to the criteria for program appraisal of the UK National Screening Committee [22,23] compris-ing characteristics of the condition, of the screencompris-ing tests and of the program.
Technical Efficacy:
▪ What is the best technique/tool for scoliosis screening in terms of validity and reliability?
Clinical Effectiveness:
▪ Is Adolescent Idiopathic Scoliosis a prevalent disease? ▪ What is the proportion of patients referred to
orthopaedics with suspected AIS from screening programs?
▪ What is the probability of actually having a diagnosed scoliosis if tested positive on screening?
Program Effectiveness:
▪ Are screen detected scoliosis patients younger and less severely affected at time of detection and diagnosis than otherwise detected patients?
▪ Are screen detected scoliosis patients less likely to be recommended for surgery than otherwise detected patients?
Cost-Effectiveness:
▪ What is the cost of screening for scoliosis and does it seem cost-effective/cost-beneficial?
c) Criteria for considering studies for this review Study design
All studies published from 1950 to mid-2010 related to screening programs for scoliosis were considered. This in-cluded all randomised controlled trials, controlled clinical
trials, comparative studies of any kind, evaluation and val-idation studies, as well as all sorts of epidemiologic studies (including prevalence studies).
Study population
The main target population was composed of adolescents aged between 10 and 18 years old. Programs focusing only on infantile or juvenile scoliosis were excluded. In addition, some programs that were designed to screen younger population were included if they provided separate data for the adolescent group.
Interventions
The interventions under consideration were all pro-grams designed to favour early detection of AIS by sys-tematic examination, of presumed healthy adolescents in the school or community setting, searching for back asymmetries. The following tests were considered: visual inspection in upright and/or forward bending position with/without objective measurement of back asymmet-ries using the scoliometer, an inclinometer, a plane and a ruler, or by analysis of Moiré topography fringe images. The test(s) could be performed either by a nurse, a physiotherapist, a sport instructor, a school doctor, a general practitioner, a paediatrician or an orthopaedist (including residents in these medical fields).
Comparisons
When available, “non-screened” patients or otherwise
detected patients were considered as control groups. Their cases may have been brought to the attention of the orthopaedist either by parent suspicion or detec-tion by another health professional. They were inciden-tal findings not recruited through a specific program targeting the early identification of scoliosis cases. They could also be historic controls before a program was established or geographic controls in regions where the program was not deployed.
Measures and outcomes
The measures used in this review were related to the di-mensions of Effectiveness previously defined (Figure 2). Studies included under the topic Technical Efficacy fo-cused on the value of the detection methods. Therefore, the measures of interest are intra and inter-observer reli-ability (assessed by the computation of intraclass correl-ation or kappa coefficients) as well as validity of the detection methods or tests which may be operationalized as sensitivity, specificity, positive and negative predictive values in test samples. Clinical Effectiveness, is the most commonly studied dimension in the scoliosis screening literature. In concordance with Fong et al. 2010 [13], we considered three main measures: scoliosis prevalence, re-ferral rate and positive predictive value as consequences of
screening programs (in real world settings). Studies classi-fied under the topic Program Effectiveness were those that focused on patient-oriented outcomes or the program benefits for the patients’ population in comparison to non participants. The two main outcomes were patient charac-teristics (maturity and curve severity) at time of detection and diagnosis, and reduction in the number of surgeries for scoliosis. Program costs reports (including detailed cost-effectiveness analysis if any) included: costs per child screened, per patient diagnosed and per patient treated and eventually cost-benefits/cost-effectiveness ratios. The considered costs were direct and/or indirect costs of pro-grams, for screening only and/or subsequent management. d) Search methods and selection of studies
A literature search using both MeSH words and free-text keywords was independently done by two content knowledgeable research assistants and validated by a li-brarian at Université de Montréal. Four databases were searched: Medline (1950 to July 2010), Embase (1980 to July 2010), CINAHL (1980 to July 2010) and the Cochrane Central Registry of Controlled Trials (EBM Reviews, Wolter Kluvers up to 2nd quarter 2010). In the searches, the subject has been described in accord-ance with the PICO method [25] using 4 concepts (the
comparisons were not included in the search strategies) linked together using logical operator“and”: the disease (Scoliosis, Spinal deformities, Back asymmetry, etc.), the population (Child, Adolescent), the intervention (Screen-ing program, Bend(Screen-ing test, Moiré topography, etc.) and the outcome (Prevalence, incidence, epidemiology, etc.), in all contexts (not restricted to school screening). In the queries, the synonyms or different terms describing the same concept or different spelling of these words were linked together using logical operator“or”. Detailed label-ling of a query example is presented in Table 1. No a priori language limits were used in the search queries. The bibliographies of all selected articles and task forces reports were searched for additional relevant references. References were imported into the software program database EndNote X3.
Two review authors evaluated the search results by reading titles and abstracts of all non redundant articles found. Papers that concern detection of non idiopathic scoliosis in related syndromes, genetic screening of scoli-osis, or scoliosis surgical treatment, were discarded. From this first selection, potentially relevant articles were re-trieved in full text for complete reading and eventually retained for further analysis. Although, the search strategy included all languages, only studies reported in English or French were considered for full text review (review of pub-lications of interest in other languages were limited to the abstract, which is a limitation of the study in terms of international coverage). In case of disagreements in the in-clusion of a study, a third review author was contacted to resolve the conflict.
The detailed algorithm for selection of studies is depicted in Figure 3. From the extensive search on the four databases with a validated query, a total of 107 non redundant relevant papers were identified and thoroughly analysed for the first four dimensions of effectiveness.
e) Critical appraisal of the studies
All selected studies were distributed for review to three reviewer teams, each consisting of two review authors with different backgrounds, an orthopaedist and an epi-demiologist. A standardized data extraction form was prepared from Excel spreadsheets. Its content was thor-oughly discussed for interpretation issues and pre-tested on three representative studies with all six review au-thors. Key findings were summarized in narrative format for each article and included: the study design, the sample size, the details of the specific intervention (tools, personnel, setting, repetitions,…), description of the main outcomes, measures of intervention effects (outcomes), the key message and the main conclusions by the original authors, the paper’s strengths and flaws, assessment of risk of bias as well as critical appraisal of Table 1 Example of search queries, Medline 1950 to
July 2010 (Lunched on July 23rd 2010)
Searches Results 1. Scoliosis/ 11886 2. Spinal Curvatures/ 403 3. screen*.mp. 362323 4. depistage.mp. 3288 5. Mass Screening/ 68020 6. Program Evaluation/ 35624 7. Child/ 1177573 8. Adolescent/ 1361381
9. (prevalence* or incidence* or epidemiolog* or detection* or adams or moire or scoliometer*).ab,ti.
1163122 10. (back adj5 (asym?etry or asym?etrical)).ab,ti. 46 11. (forward adj5 (bend or bends or bending)).ab,ti. 361
12. scolio*.mp. 14190 13. 1 or 2 or 10 or 12 14495 14. 3 or 4 or 5 or 6 or 9 or 11 1471753 15. 7 or 8 1911903 16. 13 and 14 and 15 1247 17. 13 and 14 1714
18. limit 17 to "all child (0 to 18 years)" 1291
19. 16 or 18 1291
Note: *=truncation symbol, ?=spelling variants, ab=abstract, ti=title, mp=abstract, title, author keywords and keywords plus, adj5=words in the same sentence.
the conclusions and clinical significance according to the review authors.
Assessment of methodological quality
Strength of evidence was assessed in two manners. First, from each study, the more recent version of Downs and Black tool [26] was used. It is a checklist for the assess-ment of the methodological quality of randomised and non-randomised studies of health care interventions with known satisfactory test-retest and inter-rater reli-ability [26]. Study assessment covers 4 topics: quality of reporting (10 items), internal validity (13 items), external validity (3 items) and power (2 items). This tool has been previously used by our team in the past [27-29]. Review authors clarified any item interpretation issues and inter-rater agreement was satisfactorily tested on three articles prior to this study.
As Sabirin et al. [14] suggested, effectiveness and diag-nostic studies may have different requirements for assess-ment. Therefore two questions from the original Downs and Black scale were modified. Items related to the meas-ure and adjustment for confounders and blinding of the intervention were replaced by review authors formulated questions about quality assessment of the reliability and validity experimental protocols regarding expertise of the screeners and standardization of the screening processes.
For each paper total score was obtained by consensus of two review authors. To give a more qualitative inter-pretation to the Downs and Black scores, we have pro-posed categorization of studies as high, moderate, low or very low qualityaccording to their scores. This was pre-viously suggested by others [30-32] who used quartiles distribution or equal-size intervals to interpret the scores. Here it was decided that the paper should at least clearly describe the characteristics of patients, the intervention and the main outcomes, use a representa-tive intervention in a representarepresenta-tive population, with accurate measures and appropriate statistical tests, with some consideration of confounding, and sufficient power. Moreover, using randomization, blindness, comparison groups recruited from the same population over the same period, having presented the distributions and proper ad-justment for confounders, and having explicitly reported a power calculation, would make the study high quality (maximum score on items 5, 14, 15, 22–25, 27). Under these criteria, the proposed categorization was: more than 20 = high quality, 15–20 = moderate, 6–14 = low and less than 6 = very low.
Secondly, we assessed overall quality of the evidence of the body of knowledge related to each measure/outcome as recommended by the GRADE system. According to GRADE, evaluating quality of evidence for health care
MEDLINE EMBASE 1291 1366 2657 1608 430 CINAHL EBM Reviews 309 90 71 4 524 474 107 4 Legend: Database Search results Fusion Suppression of duplicates Selection by relevance Unobtainable Inclusion for analysis
question is to determine the extent to which we are confident that an estimate of effect is correct for a par-ticular outcome [17,33]. GRADE defines eight criteria for quality of evidence assessment. For greater applicability in our review context, we have grouped the criteria under three main categories and used Ebell’s [34] approach to upgrade the level of evidence of the corpus based on “quality criteria”: strength of association, dose–response gradient, effect of bias and possible confounders, “quan-tity criteria”: number of studies, size of population, direct-ness of evidence and precision, and finally “consistency criteria” or homogeneity of results. The strength of evi-dence of the body of knowledge in this review was con-sidered to start as low (observational studies) and was upgraded or downgraded according to our interpretation of Ebell’s criteria.
f) Summary of findings
The GRADE group has proposed a general template for summary of findings (SoF) which is a convenient way of combining both main results and quality of evidence as-sessment in a table, to increase usability of the review and support decision making. Summary of findings ta-bles were compiled under each effectiveness dimen-sion that was evaluated, for each considered measure/ outcome, and for each comparison in intervention modalities available in the studies.
Based on their review, the authors proposed “recom-mendations” or more appropriately conclusive state-ments derived from the literature which could impact practice and also future research.
To provide clinical meaning to the conclusive state-ments, we recruited orthopaedic surgeons in active prac-tice with the paediatric population to participate in an expert panel modified Delphi session. Panel members were presented with the conceptual framework, the methods, the SoF tables and the proposed statements for each topic. SoF tables were clearly presented in an interactive manner using Power Point software. Upon request, detailed individual study evaluation and full text articles were provided prior to the panel session. Docu-mentation was provided by e-mail and through a dedi-cated Wikispace.
Panel members were invited to ask questions about the relevant evidence and openly discuss the content of each statement (one at a time). A moderator (one of the review authors) stimulated participation of members into the debate. Modifications were considered and inte-grated in real-time. Discussions continued until final agreement on the statements’ wording and content. g) Grading the recommendations
According to the GRADE system, recommendations may be considered as strong or weak and this decision
emerges from the consensus of an expert panel about the balance between benefits and downsides of the ad-herence to the proposed statements [16,17].
Upon agreement on a final version of the statements, panel members were invited to vote on the strength of the recommendations. Polls were conducted privately and anonymously, either on paper (first panel) and using an audience response system (Turning Point
Technologies – second panel). Two expert panels
ac-cepted to participate in this study. The first one was com-posed of 11 orthopaedic surgeons of the Quebec Scoliosis Societybrought together for a workshop session of the Annual meeting of the Society on October 2010 in Burlington, Vermont. The second panel was composed of 10 orthopaedic surgeons, members of the Canadian
Paediatric Spinal Deformities Study Group, attending
their bi-annual meeting in Quebec City in March 2011.
Discussion
In this work, there was concern to clearly define the research questions and especially the dimensions of the Ef-fectiveness concept in order to adequately cover the sub-ject and try to go further and above the work done by the task forces in the 1980s. Moreover, we aimed at providing answers to specific questions on elements of programs (screening modalities, effects on surgery rates,…) instead of a global statement for or against systematic screening. This approach is more likely to support serious reflection on secondary/tertiary prevention of scoliosis and elements that may be integrated into prevention programs and pri-mary care management of AIS patients.
A clear definition of the concepts under evaluation, and relying on a conceptual model of effectiveness appeared both sound on a theoretical basis and very helpful to sup-port search strategy, studies selection and computation of evidence.
We used a standardized tool, the Downs and Black checklist to grade the strength of evidence, which was recommended in West et al. and Deeks et al. reviews [35,36]. It was here adapted on two items for the assess-ment of screening tools. Although the Downs & Black tool is time-consuming to apply and requires consider-able epidemiology expertise, it has not been found diffi-cult to apply in this review. Unfortunately, the modified Cochrane Collaboration Risk of Bias tool for use in nonrandomized studies [37] was not ready to use when we started this work. Review authors were trained in the Downs and Black tool prior to data analysis. Working in mixed-teams of orthopaedic surgeons and epidemiolo-gists was of great benefit to put together complementary strengths and expertise, even though it needed some time
investment in the beginning to “speak the same
lan-guage”, especially on a subject which traditionally lead these professionals to opposite views [38].
The body of knowledge in this field is composed of observational studies only - a design that may suffer from many biases. Reported conclusions by the authors were then considered with caution.
The available data were not seen as appropriate for computation of pooled estimates. Therefore no statis-tical analysis was performed; neither did we conduct sensitivity or heterogeneity analysis of data. The pro-duction of a qualitative review is of course limited, but it was considered an appropriate way to proceed considering the observational nature of the available literature in the field.
Access to recognized effective treatment is a major concern in any decision about a screening program. We acknowledge the limitation of not having consid-ered scoliosis treatment, and brace management, in particular. The literature on the effectiveness of brace treatment is vast and requires a systematic review of its own. As a very good starting point, one could
consider the three published systematic reviews:
Negrini et al. 2010 [24], Lenssinck et al. 2005 [39] and Rowe et al. 1999 [40]. Despite the publication of numerous case series and a certain number of com-parative studies, best evidence on brace effectiveness is still pending. We believe that any serious effort to systematically summarize quality evidence on brace effectiveness should wait for the publication of the re-sults from current NIH clinical trial on bracing, the BRAiST study [41]. In addition, trials on scoliosis-specific exercise regimes are also in progress (e.g. [42]).
Finally, this work resulted in the elaboration of rec-ommendations, both for practice and for research. They are presented as a report of the current know-ledge and a position statement on the effectiveness of screening programs. They should not be perceived as clinical practice guidelines per se or program orienta-tions. We have compiled the evidence with great cau-tion and we are confident that the conclusions correspond directly with the results of the literature analysis. We wanted the process to be based on ex-haustive and rigorous appraisal of scientific knowledge but also to be contextualized through expert consult-ation. The strength of the evidence was clearly stated in the recommendations and therefore, the panel members considered the quality of the evidence when grading their confidence in the recommendations. There was no explicit evaluation of possible harms of the screening procedures and we relied on expert opinions for globally considering perceived harms. We believe that the submission of the recommendations to expert panels is a good way to ensure that recommen-dations have clinical meaning without being beyond the scope of the review.
Conclusions
The literature on scoliosis screening is vast. The need to propose a set of methods for critical appraisal of the literature about scoliosis screening, a comprehen-sive summary and rating of the available evidence appeared essential. The proposed methods include sev-eral innovations: i) A clear definition of the concepts under evaluation by relying on a conceptual model of effectiveness for sound theoretical basis and support for search strategy, studies selection and computation of evidence. ii) The formulation of focussed questions on specific elements of programs (screening modalities, effects on surgery rates,…) that the review intend to answer, instead of trying to get a global statement for or against systematic screening as the only endpoint. An approach that we believe is more likely to support serious reflection on secondary/tertiary prevention of scoliosis and elements that may be integrated into pre-vention programs and primary care management of AIS patients. iii) The first use of the GRADE Group approach in literature assessment in the field of scoli-osis screening. iv) The adaptation of the Downs & Black tool for the evaluation of effectiveness of
diag-nostic studies. v) The elaboration of
“recommenda-tions” or conclusive statements, both for practice and for research, derived from the literature review and contextualized by expert panels.
Methods developed in support of this work may be of interest for similar reviews in scoliosis and orthopaedic fields where the body of knowledge is mainly composed of observational studies.
Competing interests
The authors of this article have no financial or personal relationship with other people or organizations that could inappropriately influence (bias) their work, except for Hubert Labelle and Stefan Parent who have the following financial relationship to disclose: Stock ownership with Spinologics Inc. Authors’ contributions
MB conceptualized and designed the study, performed the literature search and was involved in literature assessment. She drafted the initial manuscript and approved the final manuscript as submitted. LG is the thesis director of MB. She supervised study design, especially in the adaptation of the evaluation tools, and was involved in literature assessment. She revised the manuscript and approved the final manuscript as submitted. SP was involved to the choice and validation of the evaluation tools. He was also involved in literature assessment. He revised the manuscript and approved the final manuscript as submitted. DEF contributed to the definition of the conceptual framework and was involved in literature assessment. She approved the final manuscript as submitted. IT is a research associate with the team. She coordinated data collection. She also managed the collaboration with all the other participants (members of the Quebec Scoliosis Society and the Canadian Paediatric Spinal Deformities Study Group). She approved the final manuscript as submitted. MRB is a research associate with the team. She contributed to the study design and literature search. She approved the final manuscript as submitted. JFS was involved in literature assessment and approved the final manuscript as submitted. Members of the Quebec Scoliosis Society and the Canadian Paediatric Spinal Deformities Study Group. As experts in scoliosis research and treatment, they were involved in the validation of the recommendation elaboration process and participated in the expert panels for the grading of recommendations. HL is the thesis co-director of MB. He
supervised study design, contributed to the definition of the conceptual framework and was involved in literature assessment. He also critically revised the manuscript, and approved the final manuscript as submitted. All authors read and approved the final manuscript.
Acknowledgements
Members of the Quebec Scoliosis Society and invited guests: John Braun, Lise Goulet, Guy Grimard, Hubert Labelle, Gaétan Langlois, Jean-Marc Mac-Thiong, Pierre Mercier, Stefan Parent, Benoit Poitras, James Sanders, Chantal Théorêt; and members of the Canadian Paediatric Spinal Deformities Study Group: Lauren Allen, Ron El-Hawary, Douglas Hedden, Jason Howard, James Jarvis, Hubert Labelle, Stephen Lewis, Paul Missuina, Stefan Parent, Reinhard Zeller. Research funding was received in support of this work by the Canadian Institutes of Health Research (CIHR) by three means: CIHR Research Operating Grants (2004–2007, 2008–2011); Canada Graduate Scholarships Doctoral Awards (MB) and CIHR MENTOR and AnEIS Strategic training programs doctoral awards (MB). Author details
1
Sainte-Justine University Hospital Center, Unité de recherche clinique en orthopédie, 3175 Chemin Côte-Sainte-Catherine, Montréal, Québec H3T 1C5, Canada.2School of Public Health, Université de Montréal, 7101 Avenue du Parc, 3rd floor, Montréal, Québec H3N 1X9, Canada.3Department of surgery,
Faculty of medicine, Université de Montréal, PO Box 6128, Succ. Centre-Ville, Montréal, Québec H3C 3J7, Canada.
Received: 8 June 2013 Accepted: 15 July 2013 Published: 24 July 2013
References
1. Grivas TB, Wade MH Negrini S, O’Brien JP, Maruyama T, Hawes MCm Rigo M, Weiss HR, Kotwicki T, Vasiliadis ES, Sulam LN, Neuhous T: Sosort Consensus paper: school screening for scoliosis. Where are we today? Scoliosis 2007, 2:17.
2. Plaszewski M, Nowobilski R, Kowalski P, Cieslinski M: Screening for scoliosis: different countries’ perspectives and evidence-based health care. Int J Rehabil Res 2012, 35:13–19.
3. Linker B: A dangerous curve. The role of history in America’s scoliosis screening programs. Am J Public Health 2012, 102:606–616. 4. Canadian Task Force on the Periodic Health Examination: The Periodic
Health Examination. Can Med Assoc J 1979, 121:1193–1254.
5. Goldbloom RB: Screening for Idiopathic Adolescent Scoliosis. In Canadian Task Force on the Periodic Health Examination: Canadian Guide to Clinical Preventive Health Care. Ottawa: Health Canada; 1994:346–354.
6. U.S. Preventive Services Task Force: The Guide to Preventive Services 2012, Recommendations of the U.S. Preventive Services Task Force. http://www. ahrq.gov/professionals/clinicians-providers/guidelines-recommendations/ guide/guide-clinical-preventive-services.pdf.
7. Richards BS, Vitale MG: Screening for idiopathic scoliosis in adolescents. An information statement. J Bone Joint Surg Am 2008, 90:195–8. 8. Canadian Task Force on Preventive Health C: New grades for recommendations
from the Canadian Task Force on Preventive Health Care. CMAJ 2003, 169:207–8.
9. Morrissy RT: School screening for scoliosis. Spine 1999, 24:2584–91. 10. Dickson RA, Weinstein SL: Bracing (and screening)– yes or no? J Bone
Joint Surg 1999, 81-B:193–8.
11. Bunnell WP: Selective screening for scoliosis. Clin Orthop Relat Res 2005, 434:40–5.
12. Magee JA, Kenney DM, Mullin E: Efficacy of and advocacy for postural screening in public schools. Orthop Nurs 2012, 31:232–5.
13. Fong DYT, Lee CF, Cheung KMC, Cheng JCY, Ng BKW, Lam TP, Mak KH, Yip PSF, Luk KDK: A Meta-analysis of the Clinical Effectiveness of School Scoliosis Screening. Spine 2010, 35:1061–1071.
14. Sabirin J, Bakri R, Buang SN, Abdullah AT, Shapie A: School scoliosis screening program: a systematic review. Med J Malaysia 2010, 65:261–267. 15. Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al:
GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336:924e6.
16. Guyatt GH, Oxman AD, Kunz R, Falck-Ytter Y, Vist GE, Liberai A, Schünemann HJ: GRADE: going from evidence to recommendations. BMJ 2008, 336:1049–51. 17. Schünemann HJ, Jaeschke R, Cook DJ, Bria WF, El-Solh AA, Ernst A, Fahy BF,
Gould MK, Horan KL, Krishnan JA, Manthous CA, Maurer JR, McNicholas WT,
Oxman AD, Rubenfeld G, Turino GM, Guyatt G: An Official ATS Statement: Grading the Quality of Evidence and Strength of Recommendations in ATS Guidelines and Recommendations. Am J Respir Crit Care Med 2006, 174:605–614.
18. The Cochrane Collaboration: Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0, Higgins JPT and Green S. ; 2011. http://handbook. cochrane.org/chapter_12/12_interpreting_results_and_drawing_conclusions.htm. 19. Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group: Preferred
reporting Items for systematic reviews and meta-analysis: The PRISMA statement. J Clin Epidemiol 2009, 62:1006–12.
20. Last JM: A dictionary of public health. New York: Oxford University Press; 2007:103.
21. The Cochrane Collaboration: The Cochrane glossary. http://www.cochrane. org/glossary/5#lettere.
22. Wilson JMG, Junger G: Principles and Practice of Screening for Disease. Public Health Papers #34. Geneva: World Health Organization; 1968.
23. UK National Screening Programmes web-based resources, UK Screening portal. www.screening.nhs.uk/criteria.
24. Negrini S, Minozzi S, Bettany-Saltikov J, Zaina F, Chockalingam N, Grivas TB, Kotwicki T, Maruyama T, Romano M, Vasiliadis ES: Braces for idiopathic scoliosis in adolescents. Spine 2010, 35:1285–93.
25. Sackett DL, Richardson WS, Rosenberg W, Haynes RB: Evidence-based medicine: How to practice and teach EBM. New York: Churchill Livingston; 1997. 26. Downs SH, Black N: The Feasibility of Creating a Checklist for the
Assessment of the Methodological Quality both of Randomised and Non-Randomised Studies of Health Care Interventions. J Epidemiol Community Health 1998, 52:377–384.
27. Parent S, Mac-Thiong JM, Roy-Beaudry M, Sosa JF, Labelle H: Spinal cord injury in the pediatric population: a systematic review of the literature. J Neurotrauma 2011, 28:1515–24.
28. Parent S, Barchi S, LeBreton M, Casha S, Fehlings MG: The impact of specialized centers of care for spinal cord injury on length of stay, complications, and mortality: a systematic review of the literature. J Neurotrauma 2011, 28:1363–70.
29. Parent S, Dimar J, Dekutoski M, Roy-Beaudry M: Unique features of pediatric spinal cord injury. Spine 2010, 35(21 Suppl):S202–8.
30. Hartling L, Brison RJ, Crumley ET, Klassen TP, Picket W: A systematic review of interventions to prevent childhood farm injuries. Pediatrics 2004, 114:483–496.
31. Hignett S: Systematic review of patient handling activities starting in lying, sitting and starting positions. J Adv Nurs 2003, 41:545–552. 32. Samoocha D, Bruinvels DJ, Elbers NA, Anema JR, van der Beek AJ: Effectiveness
of Web-based Interventions on Patient Empowerment: A Systematic Review and Meta-analysis. J Med Internet Res 2010, 12(2):e23.
33. Swiglo BA, Murad MH, Schünemann HJ, Kunz R, Vigersky RA, Guyatt GH, Montori VM: A case for clarity, consistency, and helpfulness: state-of-the-art clinical practice guidelines in endocrinology using the GRADE system. J Clin Endocrinol Metab 2008, 93:666–673.
34. Ebell MH, Siwek J, Weiss BD, Woolf SH, Susman J, Ewigman B, Bowman M: Strength of Recommendation Taxonomy (SORT): a Patient-Centered Approach to Grading Evidence in the Medical Literature. Am Fam Physician 2004, 69:548–56.
35. West SL, King V, Carey TS, Lhor KN, McKoy N, Sutton SF, Lux L: Systems to rate the strength of scientific evidence. Evidence Report/Technology Assessment No. 47. AHRQ Publication No. 02-E016. Rockville, MD: Agency for Healthcare Research and Quality; 2002.
36. Deeks JJ, Dinnes J, D’Amico R, Sowden AJ, Sakarovitch C, Song F, Petticrew M, Altman DG: Evaluating non-randomized intervention studies. Health Technol Assess 2003, 7:1–173.
37. Viswanathan M, Ansari MT, Berkman ND, Chang S, Hartling L, McPheeters LM, Santaguida PL, Shamliyan T, Singh K, Tsertsvadze A, Treadwell JR: Assessing the Risk of Bias of Individual Studies in Systematic Reviews of Health Care Interventions. Methods Guide for Comparative Effectiveness Reviews. AHRQ Publication No. 12-EHC047-EF. Rockville, MD: Agency for Healthcare Research and Quality; 2012. 38. Goldberg CJ, Dowling FE, Fogarty EE, Moore DP: School scoliosis screening
and the United States preventive Services Task Force. An examination of long-term results. Spine 1995, 20(12):1368–74.
39. Lenssinck ML, Frijlink AC, Berger MY, Bierma-Zeinstra SMA, Verkerk K, Verhagen AP: Effect of bracing and other conservative interventions in the treatment of idiopathic scoliosis in adolescents: A systematic review of clinical trials. Phys Ther 2005, 85(1):1329–39.
40. Rowe DE, Bernstein SM, Riddick MF, Adler F, Emans JB, Gardner-Bonneau D: A Meta-Analysis of the Efficacy of Non-Operative Treatments for Idiopathic Scoliosis. J Bone Joint Surg Am 1997, 79:664–674.
41. Dolan LA, Weinstein SL: BrAIST: planning and current status of Bracing in Adolescent Idiopathic Scoliosis Trial. In In proceedings of the 6th International Conference on Conservative Management of Spinal Deformities. Edited by de Mauroy JC, Grivas T, Knott P, Tager D. Lyon, France: Scoliosis; 2009. 4(supp 2): O42.
42. Parent EC, University of Alberta: Schroth Exercise Trial for Scoliosis (SETS). Trial NCT01610908. http://clinicaltrials.gov/show/NCT01610908.
doi:10.1186/1748-7161-8-12
Cite this article as: Beauséjour et al.: The effectiveness of scoliosis screening programs: methods for systematic review and expert panel recommendations formulation. Scoliosis 2013 8:12.
Submit your next manuscript to BioMed Central and take full advantage of:
• Convenient online submission
• Thorough peer review
• No space constraints or color figure charges
• Immediate publication on acceptance
• Inclusion in PubMed, CAS, Scopus and Google Scholar
• Research which is freely available for redistribution
Submit your manuscript at www.biomedcentral.com/submit