FACULTY
OF
MEDICINEUi
/9XS
C 33S
A THESIS
PRESENTED
TO THE SCHOOL OF GRADUATE STUDIES
OF LAVAL
UNIVERSITYFOR
THE DEGREE
OF DOCTOR OF PHILOSOPHY (Ph.D.)
BY
MARCOS CASAS-CORDERO
MASTER OF SCIENCE
FROM
THE
UNIVERSITY OF OTTAWA
COMPARATIVE ULTRASTRUCTURAL STUDY OF CQNDYLOMATOUS AND
DYSPLASTIC LESIONS OF THE HUMAN UTERINE CERVIX
RÉSUMÉ
Les condylomes acuminés peuvent se définir comme des lésions intraépithéliales,
causées par une infection virale du papillome humain.
Ces lésions se développpent dans l'épithélium pavimenteux de la région ano-génitale.
Bien qu'ayant toujours été présents au col utérin, ils ont été rarement rapportés.
En 1976, le col utérin a été reconnu comme un endroit propice au développement des
lésions condylomateuses surtout lorsqu'il s'agit de surfaces planes par opposition aux
surfaces papillaires.
L’examen cytologique des lésions condylomateuses fait voir là présence de deux types
de cellules: les koilocytes et les dyskérotocytes.
Les condylomes plans ont des caractéristiques propres:
- parmi les lésions intraépithéliales, ils se trouvent le plus fréquemment au col
utérin;
- le groupe de personnes les plus affectées est relativement jeune (21-25 ans);
- dans le passé, ces lésions étaient diagnostiquées comme des dysplasies;
- et l'examen cytologique démontre que les cellules provenant des lésions planes
ont la même cy to morphologie que le condylome acuminé.
À cause de sa morphologie cellulaire et la structure plane de la surface de l'épi
thélium, ces lésions ont été appelées condylomes plans pour les distinguer du condy
lome papillaire classique.
La proposition voulant que les lésions planes soient des condylomes suppose évidem
ment que l'agent étiologique soit le virus du papillome et que ce dernier pourrait jouer
un rôle important dans le développement du cancer du col utérin.
Au début, une telle affirmation faisait place à une grande incertitude quant à la
terminologie, l'identification histologique et l'étiologie des lésions condylomateuse du
col utérin.
La présente étude se propose comme objectif principal de vérifier si la lésion plane
est d’étiologie virale; d'établir les critères morphologiques qui pourraient aider à faire
un diagnostic qui permettrait de distinguer le condylome de la dysplasie dans le col
utérin.
Des observations au microscope électronique de lésions condylomateuses ont révélé la
présence de particules virales dans 58.88% des condylomes et 3440% des cas où le
condylome était associé avec la dysplasie. La structure des particules virales
correspondait à la morphologie du virus du papillome humain.
La présence d'antigènes du virus du papillome humain détectés à l'aide de la technique
peroxydase-antiperoxydase, a confirmé le type de virus présent dans les lésions
condylomateuses. L'antigène du virus du papillome humain fut trouvé dans 62.63% des
cas de condylome et dans 20.40% des cas de condylome associé à de la dysplasie.
L'interaction virus-cellule épithéliale se manifeste par une altération de la différen
ciation cellulaire. Cette différenciation anormale est manifestée par la formation de
trois cellules distinctes: les koilocytes qui sont des cellules montrant une zone
perinucléaire claire entourée d'une zone dense composée de tonofilaments; les
dyskérotocytes étant des cellules avec un cytoplasme dense et très kératinisé; et
occasionnellement des cellules "foncées" ayant une apparence fusiforme avec un
cytoplasme dense.
Les altérations morphologiques causées par l'effet cytopathique du virus nous ont
permis d'établir des critères histologiques permettant de différencier le condylome de
la dysplasie.
Le condylome est une infection génératrice de virus du papillome humain dans lequel
on observe l'effet cytopathique des virus (koilocytes), les particules virales et où
l'antigène viral peut être détecté.
La dysplasie ne montre pas de koilocytes. Elle est dépourvue de particule virale et on
note une absence d'antigène viral.
Le condylome associé avec la dysplasie est décrit comme un troisième type de lésion.
Il comprend 34.02% de toutes les lésions condylomateuses étudiées. La morphologie
de ce type de lésions correspond à une association des caractéris tiques du condylome
et de la dysplasie. Il est considéré comme une étape intermédiaire dans la progression
du condylome vers la dysplasie.
L'ensemble de toutes ces observations renforce l'idée que des lésions condylomateuses
du col utérin peuvent être considérées comme une première étape dans la séquence
des altérations qui précèdent le carcinome envahissant du col utérin.
TABLE OF CONTENTS
11Page
TABLE OF CONTENTS... ii
LIST OF TABLES... vi i
LIST OF FIGURES... ... i x
ACKNOWLEGMENTS... i vx
PREFACE... xvi
CHAPTER I:INTRODUCTION...
11.0 Normal uterine cervix... . . 1
1. 1 General... 1
1.2 Histology... 1
1.2.1 Squamocol umnar junction... ■... 4
1.3 Ultrastructure of normal cervix... 4
1.3.1 Exocervical epithelium... 4 1.3. 1.1 Basal zone. ... ... ... . 5 1.3. 1.2 Intermediate zone... 7 1.3. 1.3 Superficial zone... 8 1.3. 1.4 Clear cells... 9 1.3.2 Endocervical epithelium. ... 10
.1— ■ (Z} Li U H d V 1 U fîl d ... 2.1 History... ... ... 2.2 Cytology... ... .
2
.3 C r i t eria t o i dent i f y c: o n d y 1 om a t o u s .s. ’. .s Histology. ... ... ... 2. 3. 2. 1 F' a p i 11 a r y c o n d y loma... . 2.3.2.2 Fl at condylorna. ... . . 2.3.2.3 Inverted condyloma... 2.3.2.4 Atypica1 condyloma. ... s", n •—1 . FolpOSOOpy. n . . . H n n . n . o n n n . n n n . a 2 „ 3. '3. 1P
a. pill a r y c o n d y loma... 2.3.3.2 Spi kecl condyl orna. ... 2.3. 3, '3 Flat condyloma... ... . . « 0 II y s g 1 a. s x c:i... ... ...•0*... (._■ y t o J. o çiy... ... ... 3.3 Histology... ... . . . 3.4 Utrastr uctu.re ... .
4.0 Virus and cancer
4. 1 General.... . .
111Page
10 10 17 -SU ■-■crO
6
28
28
29
30
3037
434::
IV
Page
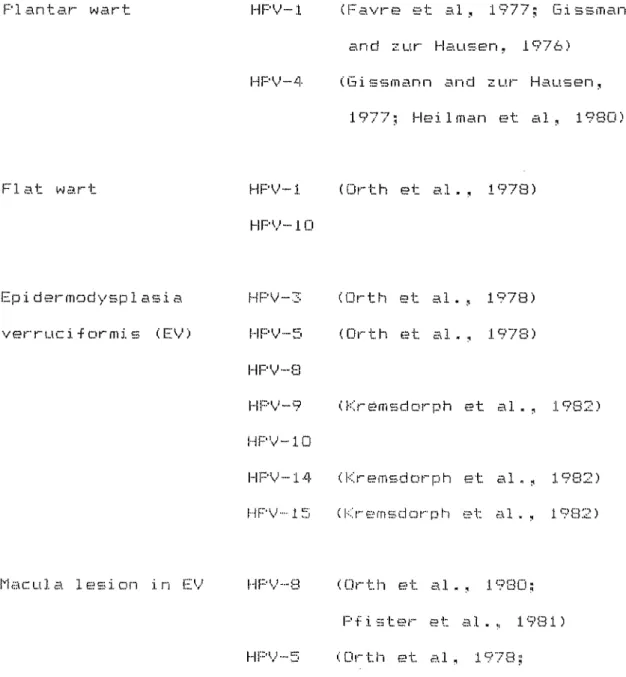
5.0 Human papi 11 ornavi rus (HPV)... . 46
5. 2 Structure... ... ... . 49
5.3
Types
o-f HPV... ... ... . 506.0 Human papi 11omaviruses and ma1 i g nan t
c on ver
ei on ... ... ... . 54
6. 1 General... ... . . 54
6.2 Epidermodysplasia verruciformis... 56
6.3 Laryngeal pa.pi 1 lama, ... . 60
6.4 Condyloma acuminatum... ... . 62
7.0 HPV and associ ated f actors in the
squamous carcinoma
of theuterine
cervix...,
648.0 Virus-host interaction. ... . 67
CHAPTER II: MATERIALS AND METHODS...
'0
1.0 G e n e i a1 2.0
Bi
ops y... . 3. 0 El e c tr on m i c: r o s c o p e t e c h n i q u e. . 3. 1 Fixati
on... . 3, 2 Post-fix ati on ... 3.3 Embedding... .3.4 Block trimmin g and sectioning.
70
78
V
Pape 4.0 Periodic acid schiff (PAS)... ...
5.0 Peroxidase-antiperoxidase reaction (PAP). 5.1 General ... ... 5.2 Immunoperoxidase method. ... 6.0 G a 3.1 o y
i
g 1 u. c:ose technique... ...CHAPTER III: RESULTS. ...
1.0 General ... ... 2.0 Condyl omatous 1 esi one . ... .
2.1 General ... .
2.2 L i g h t m i c rose o p e obs e r v ations... . 2.2. 1 Koi 1 ocytoti c: one. ... 2.2.2 Deep ep i thel i al zone... . 2.3 E3 ectron microscope observations... 2.3. 1 General ... ... ... . 2.3.2 Pure condyloma. ... 2.3.2.1 Koi1ocytotic zone... ... II I' . .!. . 1 I O i 3 O 1 e ■ n n . . . n « . u e u ■ e . n 2.3.2. 1.2 Dyskeratocytes... . 2.3.2. 1.3 Virus particles... 2.3. 2. 2 Deep epithelial zone... ... •it «■ v* li ■>!. u >it n .1. /TO Z?. .t"> C?. .1 .L “il I 11 Ü. I~1 i?, iinuuuaponnKannaN 2.3.2.2.2 Deep epithelial zone... 2. 3.2.2.3 Per i n u.c 1 ear c 1 ear z one... .
84
84
88
9194
9497
97’
99
100103
103
103
104
1 05
108
1 10113
113
1 14
1 16
VI
» 0 D ]' 1 3 ~ 1 I4, b n i ■ > K » n i nan ...na a a a a a
3. 1 Li g h t m i c r o s c: o p e
a
b s e r v a t ions. . . . 3.2 E1 sctran micras cope abservations.3a 2. 1 General. ... Page 1 17 117
118
1 18
3.2.2 U1trestructure of
epithelial
cells... 1133.2.3 Ultrastructure of basal lamina... 123
4.0 Condyloma associated with dysplasia... 124
4. 1 General ... ... ... . 124
4, 2 Koi 1 ocytot i c: zone. ... ... 125
4.3 Deep ep i thel i al z one.. ... ... . 125
4.3. 1 Dark cells... ... ... . 127
5 „0 P e r i o d i c a c i d s c: h iff ( P A S ) on
epon
thicksections... ...
1296.0
Per
o x i d a s e-an
t i p63
roxidase reaction... ...
130
7.0 Gal lot an ic acid technique. . ... . 132CHAPTER
IV;DISCUSSION
191CHAPTER V;
CONCLUSION. ...
CHAPTER VI BIBLIOGRAPHY....
213
215
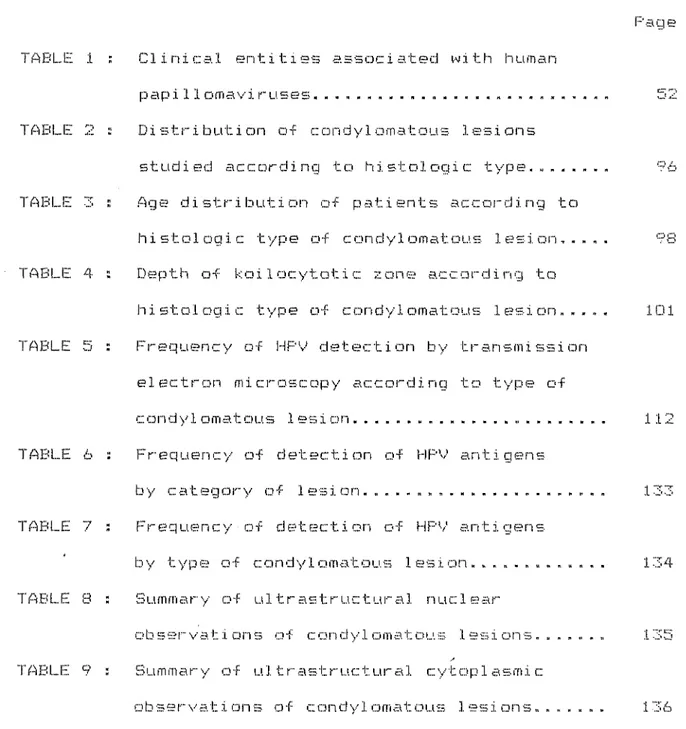
TABLE 1 TABLE 2 TABLE 3 TABLE 4 TABLE 5
TABLE 6
TABLE
7TABLE 8
TABLE 9
LIST
OFTABLES
Clinica1 entitiss associated with human
paxpi 11 ornavi ruses. ... ... . . . Dis t r i b u t ion of c: o n d y 1 o m a t o u s 1 osions
studied according to histologie type... .. Age distrib ution of patien ts according to hi s t o 1 o g i c t y p e o f c o n d y 1 orna t o u s 1 e s i on. . . „ . D e p t h o f k oil o c y t o t i c z o n e
a
c c o r d i n g t oli i s t o 1 o g i c t y p e o f c o n d y 1 ornat
o
u s 1 e s i on....
Frequency of HPV detection by transmission electron mi c: roscop y according to typ e o f c o n d y 1 o m a t ou s lésion... . . Frequency of detection of HPV antigens
by
category oflesion... ...
Frequen cy of detection o f HPV antigen
s
by
type of candy I amatau.slesion. ...
Summar y of u1
trastructural
nuciearobservati ans of candy1omatous
lesions....
S u m m a r y o f u. 11 r a s t r u c t u r a 1 c y t o p 1 a s m i c o b s 91-" v a t i o
n
s o f c o n d y 1 o m a t o u s .1. e si
o ns. ... .VII
'age 101 112134
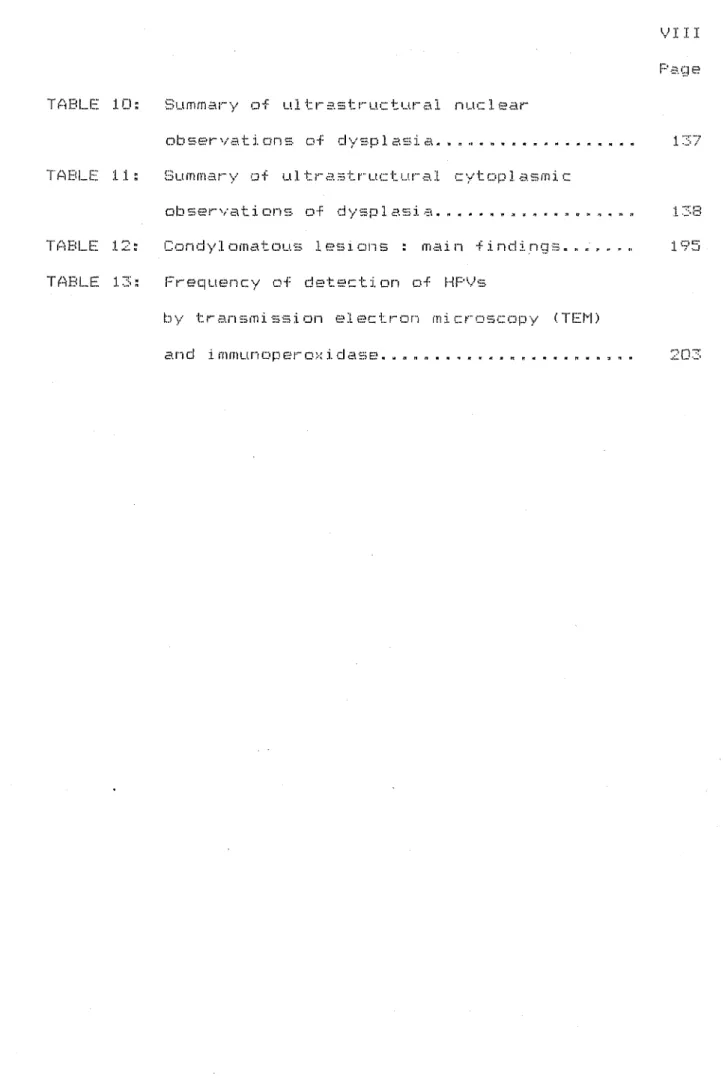
VIII
TABLE 10: Summary of ultrastructural nuclear
observations of
dysplasia
... »... 137 T A B L E; 11 :S
u m m a r ya
f u 11 r astrue t u r a 1 c y t o p 1 a s m i cobservations of dysplasia... ... 138 TABLE 12: Condyl omatous .lesions : main findings... 195 TABLE 13:
Frequency
of detection of HPVsby transmission elect non microscop y (TEM)
LIST OF FIGURES
IX Page
FIGURE 1 : Outline at methods followed in the study... 71
FIGURE 2 : Peroxidase-antiperoxidase procedure... 86
FIGURE 3 : Schematic illustration of the depth of the koilocytotic zone... . 102
FIGURE 4 : Schematic illustration of types of condyloma... ... ... 139
FIGURE 5 : Histology of condyloma acuminatum... .140
Figure 6 : Hi gher magnification of Fipure 5... 140
FIGURE 7 : Histology pure condyloma... 141
FIGURE 8 : Higher magnification from Figure 7... 141
F1G U RE 9 : Histology of mi:-: t u. r e o f condylo m
a
t ypes_____ 14 2 FIGURE 10 ; Higher magnification from Figure 9... 142FIGURE 11 : Higher magnification from Figure 9... 142
FIGURE 12 : Higher magnification from Figure 9... 142
FIG UREE 13 : H i s t ol ogy of n o r mal c o n t r o 1 t issue... 14 3 FIGURE 14 : Histology of normal epithelium and FIGURE 15 : Epon
section
of pure condyloma. ... 144FIGURE 16 : Higher magnification from Figure 15... . 144
X
FIGURE 18
FIGURE 19FIGURE 20
FIGURE 21
FIGURE 22
FIGURE 23
FIGURE 24
FIGURE 25
FIGURE 26
FIGURE 27
FIGURE 28FIGURE 29
FIGURE 30
FIGURE 31
FIGURE 32
FIGURE 33
FIGURE
34FIGURE
35FIGURE 36
FIGURE 37
FIGURE 38
Electron micrograph of control tissue... El Bctron micrograph of pure condyloma... Higher magnification of Figure 19... . Electron micrograph of pure condy1oma... Elec t r o n mi c r o g r a p h o f c o n d y.l oma
associated with dysplasia... Electron micrograph of pure condyloma... Elect ron micrograph of pure condy1oma... Elect ron microg raph of vi i- us p artici es... Histology of pure condyloma.. ... .
Electron micrograph of dysksratocytss... Electron micrograph of pure condyloma... Electron micrograph of pure condyloma... Higher magnification from Figure 29... Electr
a
n mic ra
graph of condy1 ornaassociated with dysplasia. ... . .. ... Electron micrograph of control tissue... Electron micrograph of a koilocyte... Electron micrograph of koilocytes.. . . Electron micrograph of condy1oma
associated with dyspl asi a... ... ... E1 e c t r on mi c r o g r a p h o f c o n d y 1 c m a
associated with dysplasia... ... Electron micrograph of a koi1ocyte. ... E1ectron micrograph of contro1 tissus...
Page
145
146
146
147147
148
149
149
150
150
151
152
152
153
154
155
155
156
157
159
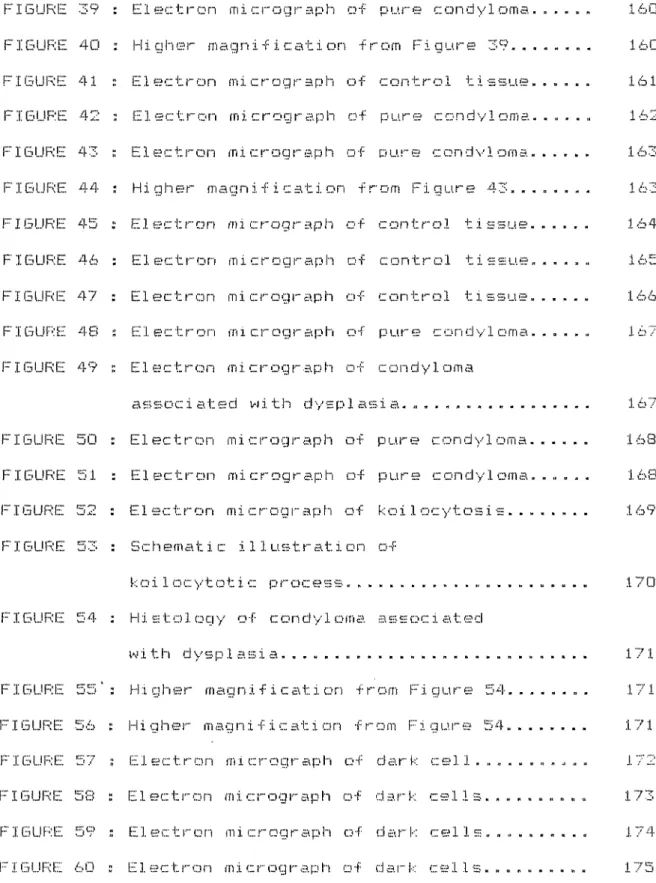
FIGURE FIGURE FIGURE FIBURE FIGURE
FIGURE
FIGURE FIGURE FIGUREFIGURE
FIGURE
FIGURE
FIGURE
FIGURE
FIGURE
FIGURE
FIGURE
FIGURE
FIGURE FIGURE FIGURE FIGUREXI
Page 39 Electron micrograph of p u. r e c o n d y 1 o m a . " - " » " 160 40 : Hig her magn1fication f rom Figure 39... - " " " - 160 41 : E1ectron micrograph o f c o n t r o I t i s s u e. ° “ " “ “ 161 42 E1 e c t r o n m i c r o g r a p h o f p u r e c o n d y 1 o m a. - " " ■ " 162 43 : Eî 1 e c t r o n m i c r o g r a p h o f p u. r e c o n d v 1 n m a. 163 44•
H i g h e r m a g n i f i c a t i o n f rom Figure 43... " * " " " 163 45 ■ E1ectron micrograph o f contro1 tiesue. " “ 1 • " 164 4 6 : E1 e c t r o n m i c r o g r a p h o f control tissue. - - " a " 165 47 : E-! 1 e c t r a n m i c r o g r a p h o f c o n t r o 1 t i s s u e. - ■ - 166C
O
N
: EE 1 e c t r o n m i crog r a p h o f pure condyloma. - - ” " " 167 49 : E1 e c t r o n m i. c r o g r a p h o f candy1 orna
associated with dyspla - - " " “ 167 50 ; Elect i" o n mi c r o g r a p h o f p u. r e c o n d y 1 o m a. ° “ « - ■ 168 51 “ E1 e c: t r o n m i c r o g r a p h o f p u r e c o n d y 1 orna. " a " 168 52 : E1 e c t r o n m i c r o g r a p h o f k oi1 ocytosis... ■ ■ " ■ ■ 169 : S c h e m a t i c il 1 u. s t r a t ion of k o i 1 o c y t o t i. c p r o cess. .
170
54 : H i s t o 1 o g y o f c o n cl y 1 o m a associated w i th
d y s p 1 a s i a... . . 171 55': Higher magnification from Figure 54... .. 171 Higher ma.gni f i c at i on f r am Fi gure 54... 17157 : Electron micrograph of dar k
58 :
Electron micrograph ofdark
173 59 : Electron micrograph of dar k C- S 1 J. S" un»un«<t>i»Ei 174FIGURE FIGURE FIGURE FIGURE FIGURE
FIGURE
FIGURE
FIGURE
FIGUREFIGURE
FIGURE
FIGURE
FIGURE
FIGURE
FIGURE
FIGUREFIGURE
FIGURE
FIGURE
FIGURE
FIGURE FIGUREFIGURE
FIGURE Page61 : Histology
of normal controltissue.... 176
6 2
:
H i stolo gy
o fn
a
r rn a 1 a n d d y s p 1 a s t i ctiss
u e. .
17 6 63 : Epon section of dysplasi a... 177 64 : Higher magnification from Figure 63.... 177 65 s Higher magnification from Figure 63... 177 66 : Eponsection
of normaltissue and dysplasia
178XII
67 : Higher magnification from Fi g ure 66 6 8 : H i g hi e r m a
gnific
a t. i o n f r o m F i g u r e o 6 6? : Hietology
of condylomaassociated
withdysplasia...
70 i Higher magnification from Figure 69 71 : E pon s e c t i o n o f p u. r e c o n d y 1
oma. . . . .
72 : Higher mag nificatia
n f rom Figure 7173
: Eponsection
ofdysplasia. ...
74 H i g h e r m a g n i f i c a t i
a
n from Figur e 775
;
El e c t r o n m i c r o g ra
p hof dysplasi a. »
76 " Electron micr
ograp
hof
dysplasi ân t;
E .1 e c t r o n m i c r o g r a p hof dysplasi
a. «78
■
H i g he r m a g n i -f i c a 't i o n from Figur e 7'79
: E1 e c t r o n micro g r a p hi ofdysplasi
a. a a80
*
H i g h e r m a g n i f i c a t i o n from Figur e 7( 81-
E1eatron microgr
aph of dysplasi a. ■ »82
: Electra
n micrographof dysplasi
a, a83
•
Electron micrograph ofdysplasi
a ■ u84
H i g h e r m a g n i f i c a t ia
n from Figur s- y..178
178
1 79180
180
180
180181
182
183
183
184
.1. 84185
186
187
187
XIII
FIGURE FIGUREFIGURE
FIGURE
FIGURE
FIGURE
FIGURE FIGUREFIGURE
FIGURE
FIGURE
FIGURE
FIGURE
Page85 : Epon section normal tissue with PAS. ... 188
86 :
Epon section pure condyloma with PAS.... 18887 : Hig her magnific ation from Figure 86... 188
88
:
Higher magnification from Fi gure 86. ... . 18889 : Purs condyloma with peroxidase-antiperoxidase. ... 189
90 : Higher magnification from Figure 89.... . 189
91 : Pure condyloma with immunoperoxidase. ... 189
92 : Higher magnification from Figure 91... 189
93 : Condy1oma associated with dysp1 asia, immunoperoxidase... 190
94 : Higher magnification from Figure 93... . . 190
95 : Condy1oma associat ed with dysplasia, immunoperoxidase. ... 190
96 : Higher magnification from Figure 95. ... 190
IVX
ACKNOWLEDGMENTS
I sincerely thank Dr. Alexander Meisels, Professor and Head of the Department of Laboratory Medicine, for providing the
opportunity for me to undertake this study, and for his
encouragement, guidance and support throughout the progress of this work.
I gratefully acknowledge Carol Morin for his constructive critisism and generous advice in reviewing the manuscript.
Special thanks to Doctors Michel Roy and Michel Fortier for suppling the biopsies used in this study,
For their competent and generous technical assistance I am much obliged to Mme
Claire
For.land, Miss Linda Chevalier, MmeSuzamne Martel and Mme Lisset Bertran.
I greatly appreciated the excellent assistence of Aristides F'ouster 1 a with the electron microscope technique.
The
material
and financial support of the National Cancer I netitute of Canada is thankful1 y ac know!edged.X
I
amvery
grateful to Ms Mary Hilton for her efficient and ess e ntia 1 w or k in t h e? c: o r recti o n a nd revi s ion of t h emanuseript.
My deepest gratitude to rny wife Susan, without whose hard work and
moral
support this thesis could not have been finished.Special thanks to my
sons
Marc andRene,
for all theinterruptions in my work to remind me that life is not only in books, and that there are also other
parts
of the the bodyas
PREFACE
Since the mid-1970s when the characteristic cellular pattern of condy1omatous lesions of the human cervix was first described by Meisels and Fortin
(1976)
.in observations of Papanicolaou smears, the squamous epithelium of the cervix has beenrecognized as the main tissue
target for
the development of condy1omatous lesions. The cytologic pattern of condylomatous lesions as reportedby the
authors was characterized by the presence of two distinct typesof
cells: koi1ocytes and dyskeratocyt.es.A year after that study appeared, two
research
groups, one from Canada (Meisels et al.,1977)
and one from Finland (F'urola and Savia,1977),
reported the existence of flat epithelial lesions in the human cervix. These lesions were observed to havedistinctive characteristics: they occurred more frequently than any other type of intraepithelial lesion
of
thecervix;
they occurred in a relatively young age-group (21-25years); they
had previously been diagnosed
as dysplasia;
and the cytological examination showed that the cells fromthese
new flat lesions had the same cytomorphology as the cells from condylomata a cuminata. Bec a u s e o f t h e s i m i 1 a r c e 1 1 m o r p h o 1 o g y ai n d theirXVII
•flat surface, these lesions were called flat condylomata to distinguish them from papillary and classical condyloma
acuminatum, which for many years have been considered
as
rare pathologic entities in the human cervix. The assumption that flat lesions are also condylomata suggests that a condyloma virus could be the étiologie agent and that the virus could be involved in the development of cancer of the cervix.At the time the present study began, there
was
still much uncertainty concerning the proper histological identification and the true etiology of flat condylomatous lesions of thecervix. These uncertainties gave rise to misinterpretations and the use of inconsistent terminology, which of course made it difficult to settle on the appropriate treatment. Thus,
research to clarify the nature of the flat lesion appeared to be justified.
I therefore decided to undertake the present study.
My
purpose was to search for the true viral etiologyof
flat lesions, and establish morphological criteria that would assist in making a differential diagnosis between condylomata and dysplasia of the uterine cervix.Since it was assumed that flat condylomata were lesions of a viral origin, it followed that virus particles and/or viral antigens would be seen or identified in the tissue from such
XVIII
lesions. To confirm these assumptions, two basic techniques were used for the purposes of this study: the electron
microscope and the peroxidase-immunoperoxidase technique. The electron microscope was used to look for human papillomavirus particles in ultrathin tissue sections and to describe the ultrastructural features of flat condylomatous lesions as compared with dysplasia. The peroxidase-immunoperoxidase
technique was used to assist in the identification of the human papillomavirus antigens in paraffin sections.
While this study was in progress, several research groups published similar studies. At the same time, partial results from this thesis have been reported in a number of
CHAPTER I
INTRODUCTION
1.0 NORMAL UTERINE CERVIX
1.1 General
The cervix uteri is a tubular structure located
at
the narrow, lower end of the uterus. Itmeasures
approximately 4 cm in length and 3 c:m in diameter. The cervixconsists
of two se
g me
n t s, t h e e ndoc e r v i a n d t h e e x o c e r v i x . E m b r yo.logically, the endocervixderives
from the paramesonephric area, and the exocer vix f rom t he urogen it a1 sinus (Forsherg, 1973; Jor dan and Singer,1976).
1.2 Histology
The histology
of
thecervix
corresponds to the general planfor
hoi 1ow organs described in histol
ogy
textbooks (Rhodin, 1981). The structure of thecervix resembles
the remainder of theuterus. It consists of a mucosa composed of an epithelium and a 1 a mina prop ria. The
se
gment of mucosa t hats
how sbranc
hinqglandular folds on its surface is the endocervix. It is lined by a single layer of mucus-producing columnar epithelium, composed of tall clear cells. Occasional cells
are
ciliated. The exocervix is the portion of the mucosa that projects into the vagina; it is lined by a stratified squamous epithelium similar to that of the vagina.The lamina propria is a framework of reticular fibers and
stroma with more fibers than cells. The squamous epithelium is joined with the lamina propria by a basement membrane; this membrane has been demonstrated by transmission electron microscope (Dougherty and Low, 1958; Ashworth et al., 1961; Younes et al., 1965). The mucosa rests upon the myometrium, which is composed chiefly of bundles of smooth muscle with intervening strands of connective tissue. An outer, more longitudinal layer of muscle continues
into
the vagina.According to observations made in the light microscope by Dierk (1927), Papanicolaou, Traut and Marchetti (1943), Papanicolaou (1954), Fluhmann (1961), and Davies and Woolf (1963), the
normal cervical squamous epithelium is composed of four cellular zones:
1. Basal zone or stratum germinativum
This
layer consists
of a singlerow
of columnar cells thatrests
on the cervical stroma. The cells have prominent nuclei and small amounts of cytoplasm. The epithelium margin borderingthe stroma and the basement membrane fold into the epithelium forming structures into which the stroma extends deeply
as
"pegs" or papillae.
2.
Parabasal zoneor
stratum spinosum profundumThis zone is made up of several rows of polyhedral cells with numerous intercellular bridges. The intercellular spaces become more clearly marked toward the superficial layer. The cytoplasm of some cells stains delicately with the Periodic Acid Schiff
(PAS) method.
3. Intermediate zone or stratum spinosum superficiale
This zone is composed of five to twelve rows of cells. They show progressive changes in shape, becoming flattened on the surface. Heavy deposits of
glycogen
are found in the cells of this zone. Some of the cells contain two nuclei.4. Superficial zone or stratum superficiale
This zone consists of several rows of flattened cells lying parallel to the surface. Here the nuclei are pyknotic and
remain in situ until the cells are desquamated, in contrast to the epidermis, which has a superficial stratum of non-nuc1eated keratinized cells called squame (s).
4
1.2.1 The squamocolumnar junction
The area of the cervical epithelium where the squamous epithelium joins the columnar epithelium is called the
squamocolumnar junction. During
certain
periods of life this area showsdynamic cellular
changes known asmetaplasia,
in which, by aphysiological or pathological process,
the columnar epithelium ispartially replaced by
squamous epithelium.Several authors
(Reagan
and Patten,1962;
Johnson et al., 1973; Koss, 197?)clearly
statethat metaplastic
changesmake the
squamoco1umnar
junction
an area with marked ne
op1 asticpotenti al
Singer and Jordan(1976
} believe 1::hat met apiasticchanges "
introducean
el ementof
instabill
tyto
the junctionalinterface
between the twoepi
thel ial types".
1,3 U ]. t r a s t r u c t u r e of an o r m
a
1 c e r v i x 1.3.1Exocervical
epithelium I n studyir
'9 t h eme
>rp that t h e c er vice 1 ep harm ones,p tr~' C I ci i iy
■for
ex amp 1 e, i nd n umber of
ce
1 1 ]. ■er t h i c i: n esso
fthe epi
hology of
the cervix
it must be rememberedithelium responds to the stimulation of
of estrogen
andprogesterone. Estrogen,
cell differentiation,
which increases the
s, at
the same
timeincreasing
thethelium.
For thisreason
it is tobe
n -3 c I" cj rl •{•• .tthe
numberan
ickness of
1 1 a
ire of
the epithelium may
vary
somewhat.Because changes resulting from cell differentiation are
gradual, it is impossible to identify all the layers described under the optic microscope. However, observation of the
epithelium in an electron microscope (Dierks et al.,
1927;
Ashworth et. a!^1960; Hackemann et al., 1968; make it possible to distinguish only a clear division between three zones. The zones described are: the basal zone or stratum germinativum, the intermediate zone or stratum spinosum, and the superficial zone or stratum functionalis.
1.3.1.1 Basal zone or stratum germinativum
The cells in the basal zone are elongated, with the long axis perpendicular to the basal membrane. Desmosomes are
observed
on the upper border connecting the basal cells with the parabasal cells. On the lateral border, the desmosomes are relatively scanty compared with the cells of the intermediate zone. The structure of desmosomes is the classic type described in the squamous epithelium (Fawcett, 1966). The desmosome consists of two dense plaques in the plasma membrane ofthe
adjacentcells;
each plaque is joined to the inner leaflet of the cell
membrane. These plaques
are
attachment sites for converging tonofilaments. The intercellularspaces
are varied in widthand
6
The basal cells are joined to the basal lamina by a large
number of hemidesmosomes (half- desmosomes), which form several electron-opaque pyramid-shaped areas. The bases of the pyramids are contiguous. Cytoplasmic tonof i 1 aments converge above the pyramids. Pinocytoti c: vesicles in various stages of development are usually observed between the hemi desmosomes (Younes et al.,
1965).
The nucleus occupies about a third of the cell. The nuclear sap (nuclear matrix or karyoplasma) contains a homogeneous
background of fine granules of chromatin (euchromatin) and some small, patchy areas of coarsely granular material
(heterochromatin). The nucleolus is clearly visible and usually eccentrically placed in the nucleus and sharply demarcated from the surrounding nuclear
sap.
The cytoplasm contains multiple organelles. The Golgi complex is well developed; it is usually found in the superior pole
of
the nucleus. There
are
many mitochondria concentrated close to the inferior pole of the nucleus. Some of them containirregular dense bodies, (600 to 800 A) in diameter. Small segments of endoplasmic reticulum are
observed
between the ribosome granules. Lysosomes are present mainly in thecytoplasmic
zoneclose
to the basal lamina. Tonofilaments arescattered
throughout the cytoplasm in a random arrangement. The 1 argest coneentratia
n usua11 y converges on the desmosomes.
The stratum germinativum is joined with the stroma of
connective tissue by the basement membrane, which is made up of the lamina lucida (300 to 350
A)
and the lamina densa (300 to 400 A). Underneath the lamina densa there is a zone ofconnective tissue made up of collagen fibers. Some of the fibers are thick (600 to 700 A in diameter), others are fine
(250 to 300 A in diameter), and still others are packages of fibrils (150 to 200 A in diameter).
1.3.1.2 Intermediate zone or stratum spinosum
The cells in the intermediate zone are larger than those in the basal layers. Their shape is polygonal but they become
progressively flatter and more elongated, with the long axis parallel to the surface.
The intercellular spaces are often wider here than in the basal layer, but they may be similar or sometimes narrower. In
general, they narrow toward the surface. Desmosomes are present in large numbers. Another type of junction, called the nexus or gap junction, has also been described in large numbers in this zone (Scott et al., 1971). The cells of the lower part of this zone show numerous long, prominent, fine cytoplasmic processes.
8
The cytoplasm shows the same organelles observed in the cells of the stratum germinativum, but they are arranged in a random manner. The cytoplasmic tonofilaments appear to be thicker and densely stained. Mitochondria are spares in the cytoplasm
instead of concentrated at a specific point in the cytoplasm.
The most prominent feature in the cytoplasm is the glycogen. It is generally displayed in small granular concentrations in the deep layers, and as large areas (lake zones) in the superficial zones, where the abundant glycogen granules occupy nearly
two-thirds of the cell.
The nuclei of cells in the intermediate zone are round to oval with smooth borders; they become slightly smaller closer to the
surface. The nuclear-cytoplasmic ratio is reduced. The nuclear sap contains fine granules of chromatin homogeneously
dispersed. The nucleoli are prominent.
1.3.1.3 Superficial zone or stratum functionalis
The cytoplasm of the nuclei of this zone is considerably •flattened. The cell sap is usually devoid of organelles.
Degenerating 1ysosome-like bodies and mitochondria often fill the cytoplasm. There is an increased quantity of tonofilaments, which are coarser and more densely stained. Sometimes small granules of keratohyalin with high electron density are
9
embedded in the tonofibrils. Desmosomes appear distorted, poorly differentiated, with a marked electron density. The nuclei are small and pyknotic.
1.3. 1.4 Clear cells
A few clear cells are observed throughout the epithelium.
Usually they are observed isolated in the stratum germinativum and the stratum spinosum profundum. This type of cell,
described in 1968 by Hackemann et al., is characterized
by
a relatively clear cytoplasm. The cell sap contains the classic organelles, such as endoplasmic reticulum, aggregates of ribosomes, and a large number of smooth-walled vesicles. The Golgi complex is well developed. The most distinct feature of these cells is the presence of numerous, striated vesicles with rounded ends. Some of these vesicles are expanded at one end in the shape of a tennis racket. Often the expansion is central or subterminal. Generally the vesicles are located in theendoplasmic zone, and occasionally they appear attached to the cytoplasmic membrane. The nuclei have irregular outlines. Clear cells are considered to correspond to the Langerhans cells
depicted by Birbeck et al.
(1961)
in the squamous epithelium of the skin.1.3.2 Endocervical epithelium
The epithelium of the endocervical segment is lined by a single layer of columnar cells. It is for the most part a
pseudostratified layer, in which the nuclei lie at varying levels of the epithelium. The bases of the columnar cells are attached to the basal lamina by hemidesmosomes. Adjacent cells are connected with junctional comp 1 ex (Fawcett, 1966).
The cytoplasmic sap shows abundant ribonucleic-like granules, mitochondria and small vacuoles of the endoplasmic reticulum. The apical part of the cytoplasm is packed with large droplets of mucus, which appear flocculent. Usually present in this apical area are cytoplasmic microvi11ae.
2.0
CONDYLOMA
According to the definition and description given in
standard
pathology books (Anderson, 1971), condylomata are wart-type lesions characterized by papillary-like proliferations
occurring on the skin and mucosa of the urogenital tract and sometimes involving the anal area.
2.1 Hi story
11
something like "round tumor". This general term appears to have been used by the ancient Romans and Greeks to identify the
proliferative exophytic lesions that develop mainly in the anogenital area (Bafverstedt, 1967).
At that time condy1omatous lesions were the focus of attention of medical and classical writers. In Latin, the words "ficus" and "thymus" were used to describe the macroscopic morphology of this disease. "Ficus" comes from the Greek term "sykon" which means "fig", and "thymus" comes from the Greek, "thymos, thymi ons".
At the beginning of the first century A.D., Celsus described in a medical writing the disease called thymi on:
But that which is named thymi on projects above
the surface like a little wart, narrow near the skin, wider above, hardish and at the top very rough.
The top in colour is like flowers of thyme, whence its name, and there it is readily split and made to bleed;,..Sometimes one is alone, generally several grow together,
either on the palms or soles of the feet.
The worst, howewer, are situated upon the genitals, and there they bleed the most.
that have long been considered as characteristic of condylomatous lesions.
The term "fig" used in those times was considered obscene because a person who had "fig" was believed to be a pederast Probably for this reason, Celsus avoided using the term. As usual, classical literature was a reflection of
society,
as see in the Martial Satires and Epigrams (Bafverstedt, 1967) which one of the writers makes special refererence to the Familia ficosa (fig family):Father and mother, daughter and son-in-law and grandchild all have the fig; not even the steward or the bailiff and the serfs in the field are spared the shameful complaint. When each and every one has the fig, is it not strange that not a fig grows in a single field !
This epigram strongly suggests that sexual (and incestuous) relationships allow the transmission of condyloma.
The classical
view
of condylomata indicated the warty nature and suggested the venereal transmissionof
this pathologic entity.we i n
1
respectable diagnosis, began to disappear from medical and classical literature. However, "ficus" or fig, which was kept outside of refined language, survived and was still in use until the late 19th century.
Later studies show that condylomata acuminatum was included in the pathologic term called papilloma. Since 1921 several
papillary lesions have been reported, but few were located in the cervix. Wharton (1921) described three cases of exophytic lesion, one of which was a typical example of condyloma
acuminatum. Wharton commented on the rarity of the lesion. The same year, Meyer (1921), reviewing the German literature, found four cases of condyloma acuminatum; one case showed an invasive carcinoma at its base. In the cases observed in Meyer's own laboratory, two of the lesions were found in pregnant women, and one papilloma had transformed to a low-grade malignancy. Meyer stated that endocervical polyps with squamous metaplasia were not to be considered papillomata. He also said that the location of the base of the growth would help to differentiate the two lesions.
In 1952, Marsh reported a compilation of cases of cervical
papillomatous lesion from literature published between 1922 and 1950. Of 31 cases, ten were diagnosed as condyloma acuminatum, six of which were found in pregnant women ; only three of the ten were considered to be malignant. During this period, the patho1ogy textbooks had al
read
y a11
empted
to define papilloma;14
Ewing stated in 1940 that papilloma was a benign tumor of pavement epithelium with supporting tissue in normal
arrangement. Marsh in 1952 emphasized that the definition of papilloma had excluded the benign tumor of the columnar
epithelium, as well as those composed of both columnar and stratified squamous epithelium, and epithelial growth such as hypertrophy and hyperplasia. Marsh revived the controversy about the papillomatous lesion and the condylomatous lesion. Finally, he suggested that papilloma be defined as a "benign epithelial neoplasm usually composed of pavement epithelium with supporting connective tissue and frequently papillary in structure"; then he added, "in regard to the cervix, the term papilloma should be limited to benign epithelial neoplasm of stratified squamous epithelium with supporting connective
tissue, frequently but not necessarily papillary in structure". Marsh also recognized that the true nature of condyloma
acuminatum was still obscure, although earlier Sutton and
Sutton (1949) and Ormsby and Montgomery (1948) had suggested a viral etiology for lesions in association with pregnancy and some histologic atypi a.
Up to that time, the literature indicated great confusion concerning the description and terminology of papilloma and
condyloma
lesions. However, a\ few years later,Raftery and
Payne (1954) used data compiled from the literature to define condyloma acuminatum as a cauliflower growth characterized by:
(a) thick papillary stratified squamous epithelium with : -acanthosis
-parakeratosis
-spongiosis with cytoplasmic vacuolization and intranuclear inclusion bodies
(b) fine dermal fronds that are: -few in number
-diffusely and focal 1 y infiltrated by chronic inflammatory cells.
Using the above criteria, Raffery and Payne reviewed 587
biopsies of the uterine cervix. The conclusion of their study was that condyloma acuminatum was a relatively common lesion
(3% of all cervical biopsies); it was found that the age range was
18 to
32years
old; it was also pointed out that clinically and histologically condyloma may beconfused
with squamous cell carci noma.Around the
same
time, Goforth (1952) and Kister and Hertig (1952)suggested
that condyloma acuminatum could bedistinguished from squamous papilloma because it was a
disease
transmissible
from
patient to patient, probablyof
viral etiology, and with no causal relationship to neoplasticdisease.
16
morphology of squamous papillary lesions, there was still confusion in defining condyloma and papilloma of the cervix.
It was not until 1958 that Woodruff and Peterson put end to the disagreement by establishing criteria to diagnose condyloma acuminatum. These authors reported that the most important histological characteristics of cervical condyloma acuminatum were "elongation and thickening of the rate pegs, marked
acanthosis, parakeratosis, papillomatosis, mild, and
cytoplasmic vacuolization". Although there is a degree of overlapping of certain features, these criteria validate diagnosis. The same authors also stressed that although malignant changes were rare in these lesions, such changes could make it difficult to arrive at a differential diagnosis.
For several decades it was believed that condylomata acuminata or genital wart lesions had a viral origin (Ciuffo, 1907). This idea
was
never proved, although for long a time several authors shared the opinion that the common wart, juvenile wart, and genital wart were caused by the same virus (Waelsch andHabermann, 1924; Young, 1964; Rowson and Mahy, .1967; Lever and Schaumburg- Lever, 1975).
The presence of intranuclear virus particles in condyloma acuminatum was confirmed by Dunn and Ogilvie (1968) and Oriel and Almeida (1970) with the transmission electron microscope. These virus particles were morphologically similar to the human
17
papillomavirus (HF'V) observed in wart lesions in the squamous epithelium of the skin.
The HF'V virus attracted attention as a possible new virus to be related to the development of cancer of the external genitalia. Nevertheless it was already known that condyloma acuminatum was rare in the human cervix, compared with the external genitalia, where it was very common pathology.
2.2 Cytology
It is widely accepted in the field of cytology that
Papanicolaou smears provide a highly effective method and an indispensable tool for the detection of cervical lesions
(Quizibash, 1974; Meisels and Morin, 1984
In the study of cervical condylomata the observation of cells in smears was important in establishing criteria for
differentiating the lesions.
Using cytologic
smears
from the uterine cervix, George Papanicolaou (1960) was the first to describe cellsoriginating from condylomata acuminata. He found that the cells showed nuclear enlargements and that hyperchromasi a was a
18
cells were well differentiated with an abundant cytoplasmic supply. Papanicolaou
also
warned that these cells could be confused with cells from malignant squamous lesions, and he noticed that some cells had a perinuclear halo.Cells with a perinuclear halo, however, have been studied since the late 1940. Ernest Ayre (1949) was the first to point out the? morphology of certain cells observed in the Papanicolaou smears. These cells were characterized by the presence of a perinuclear clear zone, which Ayre plainly illustrated in his publication. The morphology shown in Ayre's illustration leaves no doubt that those cells today would quickly be identified as typical of the condyloma.
A few years later in another publication about cancer cytology of the uterus, Ayre (1951) again presented excellent pictures of cells with a\ cytoplasmic clearing which he named "halo cells". In addition he illustrated a few sections of tissue from a flat zone of condyloma, similar to those that would be described two decades 1 ateh
as
flat condylomata (Mei sel s et al., 1977; Purola and Savia, 1977). Ayre thought that themorphologic changes such as "halos" should be considered to be the precursor of preinvasive cancer. Thus he called these
lesions
"nearocarcinoma" (Greek "nearo" = earliest stage).George Papanicolaou (1954) also focused attention on a type of cell that
showed
features similar to those of the cells19
described
previously by Ayre. He stated that one of the patients whose smears showed these particular cells had a biopsy showing epidermoid carcinoma in situ, thus suggesting that thecells
with a perinuclear clear zone may have some kindof
relationship with genital cancer. In the same publication Papanicolaou used the term "perinuclear halo" to describe a perinuclear clear zone that was usually observed in smears from cases of vaginal trichomoniasis.The fact that "peri nuclear halo" (Papanicolaou) and "halo cell" (Ayre) were similar in appearance brought confusion and a
variety of interpretations among clinicians. Two years later, Koss and Durfee (1956) defined the perinuclear cytoplasmic clearing as koilocytotic atypi a, described as an "unusual pattern of the squamous epithelium of the uterine cervix",
which histologically was characterized by the presence of large cells with small, irregular and hyperchromâtic nuclei.
Surrounding the nuclei was a clear cytoplasmic zone, which gave the impression that the nucleus was suspended in an empty
space. By means of this description, Koss and Durfee could help clinicians to avoid confusing koilocytotic atypi a with other cervical lesions. Furthermore they concluded that although the role of koilocytotic atypi a in the earlier stages
of
thedevelopment of cervical cancer was not clear, the possibility that some of these lesions could progress to cancer could not be excluded.
The illustrations of cells and tissue published by Ayre (1949 and 1951) strong1 y show that the "halo cell" corresponds to epithelial cells with koilocytotic atypi a reported by Koss and Durtee (1956).
Several causes of koi1ocytosis have been suggested in the past. Sagiroglu (1959) speculated that the peri nuclear cavity could
be a mechanically produced artifact, caused by scraping the epithelium of the cervix with a wooden spatula used to collect the exfoliative cells. Similar cytoplasmic alterations were reported as a result of topical applications of podophyl1in on the cervix (Saphir
et
al., 1959). Electron microscope studies made by Okagaki et al. in 1973 have depicted koi1ocytosis as an abnormal karyopyknosis, possibly caused by abnormalphysicochemical dynamics of the cells. De Giroi ami, Ayre and Claudatus (1959) considered koi1ocytosis a "nuclear disease" in which the nuclear membrane was the outside border of the
cavity. At that time no one had even pointed out a possible manifestation of viral disease, until Ayre (I960) in an exceptional paper described the "halo cell" as a cell
characterized by a perinuclear translucent area surrounding the nucleus, mainly in cells
of
superficial or intermediate origin. The-? perinuclear area is well defined by a sharp, dark, andintense border. What was very interesting in light of today's knowledge was Ayre's early idea, which deserves special
21
The thought is, then, that halo cells represent the earliest manifestation of malignancy in human cells, that they are caused by some nucleic
acrid-viral infectious activity in an estrogenic environment which produces derangement of cell metabolism and orderly replication of cells, and that they are probably a mutant deviation towards malignant cell growth.
A year later Naib and Masukawa (1961) published a paper in which they depicted cells from a classical condyloma
acuminatum. The cells reported were large intermediate squamous cells that appeared swollen and edematous with a thick, clear, basophilic, poorly keratinized cytoplasm and ill-defined
borders. The chromatin pattern was bland; the nucleolus was usually prominent. Intranuclear basophilic inclusion bodies varying in number, shape, and size were sometimes seen. Cytoplasmic degenerative vacuoles, perinuclear halo,
bi nuci eation, karyorrhexis and nuclear pyknosis were considered as secondary characteristics. The authors did not find any
morphological criteria to indicate malignant changes. Their description making reference to intranuclear basophilic inclusion bodies appears more likely to be derived from the lesion known to be produced by herpesvirus II.
In 1963, in studying perinuclear alterations, Sagiroglu
clear area of 5 u large at the most surrounding the nucleus (Koss and Wolinska, 1959; De Giro! ami, .1.967), and commonly seen in inflammation by trichomonad infestation, from the
"paranuclear halo", corresponding to
the
clear zone but usually ■formedat one
sideof
the nucleus. At that timethis
alteration was still consideredby
Sagiroqlu to be a mechanically produced artifact.A few years later, on the basis
of
accurate observations of cells with perinuclear clearings. De Girolami (1967) attemptedto
clarify the agents that produced the perinuclear halo. He concluded that this halo was associated withacute
and chronic cervi citis, especi a11 y due to trichomonas vaginalis, and that koi1 ocytot ic atypi a was not associated with such infections, but was a manifestationof
marked dysplasia,possibly
of viral origin.Several
studies have been done since Papanicolaou (1960) made thefirst observations
of cellsamples
showing condylomaa c
u
minatum. However , adiagnostic
c: y tologic p a t tern o f t h i s lesion was not correctly identified until recently when Me i sels and Fortin (1976) described the characteristic cytomorphology o f c o n d y 1 o m a t o us
.1.esio
n s o f t h e c e r vi x
. In a sec o n d p a p e r , Meiselset
al.(1977)
made a correlation study bymeans
of c: y t ology,
his t o 1 o g y a n d c o 1 p oscopy.The
a u t h o r s d e s c r i b eel t h e"flat" condylomatous lesion, which had never before been recognized in the
cervix.
The sameyear
two Finnish authors,F'urol a and
Savia (1977),
reported almost identical conclusions.These flat condylomatous lesions were observed to have
distinctive characteristics: they ocurred in
a
relatively young age-group (21-25years);
they ocurred more frequently than any other type of intraepithelial lesion of the cervix; thecytological examination showed that the cell showed the same cytomorphology as the cell from condyloma acuminatum; and they had previously been diagnosed as dysplasia.
Since this discovery, research focused on this "new" pathologic entity has steadily been increasing (Syrjanen, 1979; 1980; Reid et al., 1980; Walker et al., 1983; Crum et al., 1983; Mei sels et al., 1983; Zuna, 1984; Coleman and Ri chman, 1985.
2.3 Criteria to identify condylomatous lesions in the cervix
The criteria to identify condylomatous lesions of the uterine cervix will be described here under three main headings:
Cytology,
Histology and Colposcopy.2.3.1
Cytology
The cellular pattern of condylomatous lesions
of
the cervix described by Meisels and Fortin (1976) and F'urol a and Savia24
have been proved to occur more frequently than the classical exophytic type. According to Meisels, "The smear was usually clean, with few or no inflammatory cells. The cell population consisted of intermediate and superficial cells. " Two types of cells were observed to be peculiar to condylomata — the
dyskeratocyte and the koilocyte.
Dyskeratocytes
These are isolated cells, or more often small aggregates of cells showing dyskeratotic changes with a dense yellowish or orangiophi1ic cytoplasm and small, slightly irregular, dense nuclei of the size normally found in intermediate cells.
Koi1 ocytes
The "balloon cell"
(Meieel's
term) is an intermediate cell, often quite enlarged, containing one or two and occasionally several hyperchromât.ic, slightly irregular nuclei. Thechromatin is dense and may be coarsely granular. Nucleoli are either absent or inconspicuous. The nucleus is surrounded by an irregular clear area, which may vary in size from a small halo to a large empty space, occupying most of the cytoplasmic area. Peripheral to the nuclear clearing, the cytoplasm is quite
dense, almost
glassy
in appearance and shows a characteristic amphophilic staining.It is important to point out that the "balloon cells"
correspond to the cells that were previously described by Koss and Durfee (1956) as "koi1ocytotic atypia" and as early cancer cells by Ayre (1960).
2.3.2 Histology
According to recent histopathological descriptions (Meisels and Fortin, 1977; F'urola and Savia, 1977; Meisels et al.,1981),
•four different histologic types of lesion are diagnosed as
condyloma in the cervix: papillary or exophytic, flat, inverted or endophytic, and atypical.
2.3.2.1 The papillary condyloma (Figures 4, 5)
This exophytic lesion corresponds to the classical type previously described in the literature respecting the vulva
(Gardner and Kaufman 1965) and the cervix (Woodruff and
Peterson, 1958). Woodruff and Peterson described the histologic features of the papillary cervical condyloma:
- a marked degree of acanthosis, considered to be the most prominent feature of the papillary condyloma. The prickle-cell layer is hypertrophic, but the epithelium usually appears with an orderly arrangement and, as a rule, neoplasia can be readily dismissed.
26
- cytoplasmic vacuolization in the acanthotic zone of the epithelium is frequently seen, but is considered of rather secondary importance for the diagnosis.
- parakeratosis is consistently noted to a varying degree. However, hyperkeratosis rarely occurs.
- elongation and thickening of the rete pegs. They are
interconnected and may thus present a confusing picture to the inexperienced observer. This is especially true when tangential sections of the tissue are made.
- papillomatosis (exophytic papillary proliferation) produces the typical papillary or tree-like architecture. The papillae are narrow and often edematous with a chronic inflammatory infi1trate.
2.3.2.2 The flat condyloma (Figures 6, 7)
This lesion was described by Meisels and Fortin (1977) and F'urola and Savia (1977). It is characterized by ax virtually unaltered architecture and lacks the classical exophytic
morphology of the condyloma acuminatum. The squamous epithelium may be of normal thickness, often increased thickness or
occasionally very thin. The papillae of the connective tissue and small vessels are elongated and widened. Usually there is a flat focus of acanthotic epithelium with
27
mildly accentuated rete pegs. The cells of the basal layers are dense, with abundant cytoplasm, in contrast to the superficial cells. The basal cells maintain normal polarization. The upper
layer of the epithelium displays marked perinuclear cytoplasmic clearing (koi1ocytosis) that gives to the superficial zone of the lesion its characteristic appearance. The surface layers often show keratinization or dyskeratotic changes. The nuclei of the deeper cell layers are relatively large and display finely dispersed chromatin, whereas the nuclei of the upper layers are retracted, hyperchromatic, rather large and
sometimes pyknotic or karyorrhectic. There is bi- and
multi nuci eation. Nucleoli are generally very visible. Sometimes the flat lesions show small
spikes
on the surface of theepithelium, which becomes irregular. This variation of the flat condyloma is called the spiked condyloma.
2.3.2.3 The inverted condyloma (Figures 8, 9, ID)
The inverted condyloma was also described by Meisels and Fortin in 1977. It was depicted
as
a flat lesionthat
resembles the inverted papilloma of the nose. The main feature is a papi liar- proliferation into the glandular neck, obliterating and taking theplace
of the columnar epithelium. The histologic2.3.2.4 Atypical condyloma
In 1981, Meisels et al. reported that some condylomatous
lesions (atypical condyloma) showed marked nuclear atypia. Such lesions have the same general morphology as the flat condyloma. The authors state that around 9 % of atypical condyloma show indisputable evidence of progression to dysplasia and carcinoma in situ. This capacity to progress to a malignant lesion gave the authors the idea that atypical condyloma represents a further step in the evolution toward cervical cancer. The
authors also warn that these lesions can easily
be
misdiagnosed as dysplasia or even carcinoma in situ.2.3.3 Colposcopy
Condyloma acuminatum is a lesion that most clinicians agree is easy to identify with the naked
eye.
However, the morphology of the flat condyloma described by Meisels et al. (1977) issimilar to that of the dysplastic
lesion.
For thisreason,
both these lesions are difficult to distinguish using a col poseope.Three types of lesion (papillary, spiked and flat condylomata) can be identified with the colposcope (Meisels et al.,
1977,
1979; Roy et al., 1981, 1983).
1 The papillary or exophytic condyloma
It is observed as a raised, dense, thick, white lesion with finger-like projections resulting in an irregular surface
contour. Capillary loops are usually seen in the stroma of each projection. Hyperkeratosis is a common finding that sometimes masks the capillary vessels.
2.3.3.2 The spiked condyloma
It is a flat, white
area
characterized by the presence of small projections that look like spikes. Usually there is nocapillary loop visible in the spikes. This type of lesion was originally called "early condyloma" (Meisels et al., 1977) but
in a subsequent publication, Roy et. al. (1981) stated that it was more reasonable to
call
it "spiked condyloma" because there was no proof yet that it would eventual 1 y develop into a florid 1esion.2.3.3.3 The flat condyloma
The surface is flat and frequently shows a
mosaic
pattern. It appears as a white lesion with a somewhat granular surface. Usually no capillary vessels are seen in the flat condyloma. Often the surface reveals some dotted areas. The flat condyloma observed with the colposcope cannot be distinguished from0 DYSPLASIA
3.1 History
When the early studies on the origin of cervical cancer
appeared, several investigators thought that a surface lesion with the histologic characteristics of malignancy could be? “early" carcinoma (Schawenstein, 1909; Schot1 sender, 1908; Rubin 1910, and Schott1aender and Kermanner, 1912), Later, Schiller (1927), and Meyer (1941) stated that cancer of the? cervix developed in two stages: a long latent period or noninvasive stage, and a later period, the?
“invasive
stage". addition, these investigators thought that tumor malignancy appeared as a fully developed cancer with no intermediate stage, and that it extended along the epithelial surface by transforming the neighbouring normal cells (Schiller, 1927) oi adjacent tissue (Meyer, 1941).Subsequent studies by Younger and Hertig
(1949),
Fundet
al. (194-8), Stoddar (1952), Reagan(1953),
Mackay et al.(1959),
and Fluhmann (1961) indicated that malignant
cells
graduallyevolved
fromareas
in which the cellsshowed obvious
atypi a. These authors also said that thetype of
atypi a differed markedly from the one observed in a fully developed cervical carcinoma.31
Further studies based an data from several sources (Reagan, 1964) stated that certain morphologic differences could be discerned among preneoplastic lesions: those in which the epithelium showed slight alterations, and those characterized by the presence of a uniform population of small cells showing anaplastic changes. The second group was named "carcinoma in situ", and lesions with fewer abnormalities were called
dysplasia. Today cancer in situ is a widely accepted term that was first suggested by Schott 1aender and Kermauner in 1912.
The word dysplasia comes from the Greek language (dys = bad, plasia - moulding). The use of this name in cytology was
suggested by Papanicolaou (1949), although it was Reagan et al, (1953) who introduced it into the terminology used in
gynecologic pathology. The concept of dysplasia was rapidly adopted by clinicians to characterize some abnormalities of the squamous epithelium that were believed to be earlier neoplastic changes than the ones described as carcinoma in situ. Perhaps because the preneoplastic changes progressed through stages of advancing severity until the invasion took place, a multitude of terms have been used to describe these changes:
leucoparakeratosis or hyperkeratosis (Schiller 1938) , atypi a (Hoffman, 1949), atypical (Hinselmann, 1949; Bechtold and Reicher, 1952) , restless, (Held, 1952), unquiet (Bajardi,
1961), basal cell hyperactivity (Galvin et al., 1949),
and Te Linde, 1949; Novak and Galvin, 1951), atypical
hyperplasia (Figge et al., 1962; Mckay, 1959; Reagan et al., 1955) , anaplasia (Mckay et al., 1959; Younge and Hertig, 1949), dissociated intraepithelial anaplasia (Fund and Lacy, 1951), precancerous metaplasia (Carson and Go'll, 1954), koilocytotic atypi a (Koss and Dur-fee, 1956), atypical condyloma (Meisels et al., 1981), atypical immature metaplasia (Crum et al., 1983).
Reagan and Hamonic (1956) subclassified dysplasia into three groups: mild, moderate, and severe. In 1969, Patten introduced an additional subdivision of dysplasia — keratinizing,
non-keratinizing and "metaplastic. Thus, the above terms could be made even longer and more complex thanks to a choice of
six
further additional adjectives.
The differences in terminology are due mainly to the broad
histological spectrum seen in tissue that is gradually changing as the lesion evolves, and to the lack of clear morphologic criteria on which to base diagnoses. The use of varying
terminology has resulted in confusion in interpreting cervical lesions. Indeed, a group of prominent pathologists and
clinicians came together in an effort to obtain much-needed uniformity of internationally accepted terminology for
lesions
of the uterine cervix (International Agreement on Histological Terminology for Lesions of the Uterine Cervix, 1962).
The members of this group agreed to define dysplasia in the following terms :