UOJM | www.uojm.ca November 2017 | Volume 7 | Issue 2
27
Keywords: Emergency Contraceptions; IUDs; Canada
Objectives: Post-coital insertion of the Copper-T intrauterine device (IUD) is the most effective method of emergency contracep-tion (EC). However, few women use this method of pregnancy prevencontracep-tion in Canada. Our study aimed to explore Ontario pharma-cists’ knowledge of the IUD as EC and interest in a hypothetical “same day referral” program that would provide women seeking progestin-only EC with information about and a timely referral for post-coital IUD insertion.
Methods: We received 198 mailed surveys from representatives of Ontario pharmacies and conducted 17 in-depth interviews with a subset of respondents in 2015. We analyzed the survey data using descriptive statistics and interviews for content and themes using both deductive and inductive techniques.
Results: Our results suggest that Ontario pharmacists underestimate the efficacy of the IUD as EC and lack awareness of the proto-cols for use. Survey respondents and interviewees expressed support for a “same day referral” program in Ontario and believe more effective methods of EC should be easily accessible. Interviewees discussed current barriers to the use of IUDs as EC, including the up-front costs associated with insertion and a general lack of awareness about EC among health professionals and communities.
Discussion: There is a significant need for continuing education on the full range of EC methods among pharmacists. Consider-able enthusiasm exists for undertaking efforts to expand access to more effective EC methods. Developing a pilot project to facili-tate timely referrals for post-coital IUD insertion appears warranted.
Andréanne Chaumont, MSc
1, Angel M. Foster, DPhil, MD, AM
2,3*1 Faculty of Medicine, University of Ottawa 2 Faculty of Health Sciences, University of Ottawa 3 Institute of Population Health, University of Ottawa * Corresponding author
ABSTRACT
Objectifs: L’insertion postcoïtale d’un dispositif intra-utérin (DIU) au cuivre est la méthode la plus efficace de contraception d’urgence (CU). Toutefois, peu de femmes au Canada utilisent cette méthode de prévention de la grossesse. Notre étude visait à ex-plorer les connaissances des pharmacien(ne)s ontarien(ne)s sur le DIU utilisé comme CU, ainsi que leur intérêt pour un programme hypothéque d’orientation du même jour, qui fournirait en temps opportun de l’information et une insertion postcoïtale d’un DUI aux femmes désirant une CU à progestatif seul.
Méthodes: Nous avons reçu 198 sondages par la poste de la part de représentants de pharmacies ontariennes, et avons mené 17 entrevues détaillées avec un sous-ensemble des répondants en 2015. Nous avons analysé les données de l’enquête à l’aide de statis- ques descriptives, ainsi que le contenu et les thèmes des entrevues au moyen de méthodes déductives et inductives.
Résultats: Nos résultats indiquent que les pharmacien(ne)s de l’Ontario sous-estiment la capacité du DIU utilisé comme CU et ne con- naissent pas les protocoles nécessaires. Les répondants à l’enquête et les sujets interrogés ont exprimé leur soutien au pro-gramme d’orientation du jour même en Ontario et croient que des méthodes plus efficaces de CU devraient être facilement acces-sibles. Les personnes interrogées ont discuté des obstacles actuels à l’utilisation du DIU utilisé comme CU, incluant les coûts initiaux associés à l’insertion, et le manque général de connaissances sur la CU parmi les professionnels de la santé et les communautés. Discussion: Il existe un besoin important de formations professionnelles continues pour les pharmacien(ne)s sur la gamme com-plète de CU. Plusieurs démontrent un enthousiasme considérable quant au déploiement d’efforts pour améliorer l’accès à des mé-thodes plus efficaces de CU. Il semble justifié d’instaurer un projet pilote qui faciliterait l’orientation pour la pose postcoïtale d’un DIU, et ce, en temps opportun.
RÉSUMÉ
Introducing a “same day referral” program for
post-co-ital IUD insertion in Ontario: A mixed-methods study
with pharmacists
UOJM | www.uojm.ca November 2017 | Volume 7 | Issue 2
28
U
nintended pregnancies continue to be a majorpublic health issue in Canada; nearly one in three Canadian women experience an unintended preg-nancy over the course of their reproductive lives [1]. Methods of long-acting reversible contraception (LARC), including the hormonal intrauterine device (IUD), the Copper-T IUD, and implants, are safe and extremely effective at prevent-ing pregnancies for 3-10 years [2]. In addition, the post-coital insertion of the Copper-T IUD is the most effective method of emergency contraception (EC) [3-5]. Insertion of the IUD within 7 days of unprotected or under-protected sexual intercourse represents an important option for women who not only want to prevent pregnancy after a specific event but also desire high-ly effective, ongoing contraception [5,6].
In Canada, the IUD remains underused for both contraceptive and EC purposes [7,8]. A number of factors likely influence this dynamic, including lack of awareness and misinformation about the device, the up-front costs associated with insertion, and the limited availability of heath care professionals trained in insertion and removal. Indeed, a study conducted in Ontario found that a limited number of family medicine residents felt adequately prepared to perform an IUD insertion [9]. Although overarching trends suggest that the use of the IUD, in general, is increasing, use of the IUD as EC is minimal [4].
Progestin-only emergency contraceptive pills (ECPs) have long been available in Canada and are the most widely used method of post-coital pregnancy prevention [10]. In Ontario, progestin-only ECPs (commprogestin-only referred to by the brand name Plan B®) have been available directly from pharmacies for more than a decade [11]. However, a number of studies suggest that there are barriers to “real world” access [12-14]. Further, some evi-dence suggests that progestin-only ECPs may be less effective when used by women weighing 165 pounds or more [15]. Consequently, health professionals have repeatedly identified developing mechanisms to increase access to the IUD as EC as a priority. Currently, there are four brands of IUDs that can be used for EC, Flexi-T®, Liberté UT®, Mona Lisa®, and Nova-T® [16]. In recent years, a team in British Columbia developed a pilot project to explore the possibility of implementing a timely re-ferral program [17]. This program trained pharmacists to offer women seeking progestin-only ECPs the option of being re-ferred for an IUD and created a network of area providers that would then be able to schedule an insertion within seven days
[18]. Participating pharmacists and clinicians found the initia-tive acceptable and the program successfully improved the ac-cessibility of IUDs for post-coital contraception [17].
To date no similar projects have been undertaken in Ontario. However, pharmacists play a critical role in EC service deliv-ery in the province and as the most available, accessible, and approachable health care professionals they could play a cen-tral role in increasing timely access to the IUD as EC. Using a mixed-methods approach, we explored Ontario pharmacists’ EC knowledge, attitudes, and provision practices; in a previous publication we presented the results related to progestin-only ECPs [19]. In this paper, we specifically focus on the findings related to the IUD as EC and explore pharmacists’ opinions re-garding a hypothetical “same day referral” program similar to that which was implemented in British Columbia.
METHODS
As we have detailed previously [19], our study comprised two components—a mailed survey to a representative sample of retail pharmacists in Ontario and in-depth interviews with a sub-set of survey respondents. We received ethics approval from the Research Ethics Boards at the University of Ottawa to conduct this study (File#H03-14-20 and File#02-15-12).
Component I: Mailed survey
Based on a questionnaire developed by Dunn and colleagues [10], we developed a 56-item survey to explore Ontario phar-macists’ EC knowledge, attitudes, and provision practices. Our survey included five primary sections: 1) demographic ques-tions about the respondent and the pharmacy; 2) knowledge of different modalities of EC; 3) EC provision practices; 4) atti-tudes toward EC and patients seeking EC; and 5) a free space for additional comments. Six questions specifically focused on the IUD as EC. We piloted the survey instrument, in both English and French, with 13 pharmacists in the greater Ottawa region and integrated feedback into the final instrument.
We used the Ontario College of Pharmacists (OCP) database to identify our sample of retail pharmacies. Using a stratified random selection process, we selected 1,428 pharmacies—or roughly one third of retail pharmacies in the province for in-clusion; we intentionally oversampled independent pharma-cies and pharmapharma-cies located in rural and Franco-Ontarian communities in order to capture a range of perspectives and experiences. We invited the head pharmacist—or the
UOJM | www.uojm.ca November 2017 | Volume 7 | Issue 2
29
sitioned person at the pharmacy—to complete the survey. Wefielded our four-contact survey over a four-month period (June 2015-September 2015). We initiated the study by mailing a full bilingual survey package including the instruction letter, sur-vey instrument, stamped return envelope, and lottery and key informant interview response card to pharmacies in our sample. We used unique identifiers to track respondents and sent a re-minder postcard, a second survey package, and a final post-card reminder to non-respondents at 2-4 week intervals. After accounting for incorrect addresses and returns, we ultimately contacted 1,396 pharmacies. We included all surveys received before the end of the 2015 calendar year in our analysis. Component II: In-depth interviews
We invited all survey respondents to participate in a follow-up in-depth interview (IDI). AC, who at the time was a master’s stu-dent in the Interdisciplinary Health Sciences program at the Uni-versity of Ottawa, conducted all telephone/Skype interviews in English or French after being trained by her thesis supervisor (AMF), a medical doctor and medical anthropologist. The semi-structured interview guide comprised a series of questions re-lated to initiatives to improve and expand evidence-based EC service delivery practices. We presented participants with infor-mation about a hypothetical “same day referral” program, mod-elled after the BC initiative, and asked interviewees about their interest in the program and to comment on perceived facilita-tors and barriers to establishing a program in Ontario. The IDIs averaged 35 minutes and occurred between July and October 2015; with the permission of interviewees, we audio-recorded and later transcribed all interviews. In addition AC took inten-sive notes during the interview and formally memoed shortly after. As a small token of our appreciation, we gave all partici-pants a CAD20 gift certificate to Amazon.ca.
DATA ANALYSIS
We entered survey data into FluidSurveys and later exported the information to IBM Statistics SPSS 23.0. We analyzed the demographic, knowledge, and attitudinal data using descrip-tive statistics and performed cross tabulations to explore differ-ences in knowledge and attitudes by region and rural/urban lo-cation. We used ATLAS.ti to manage the IDI notes, memos, and transcripts. AC developed an initial codebook based on the in-terview guide and added and defined new codes that emerged from the data. AMF reviewed the codebook and a sample of coded transcripts, and discussed the findings regularly with AC. We analyzed the two project components separately and in the
final phase reviewed both components for concordance and discordance. We have removed or masked all identifying infor-mation of both participants and their pharmacies.
RESULTS
Description of survey participants
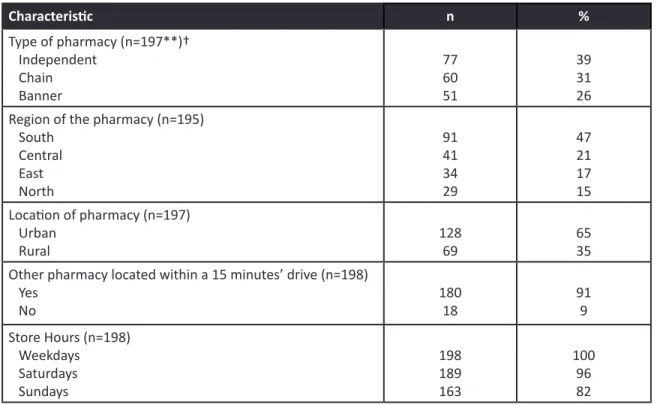
Of 1,396 pharmacies in Ontario that we contacted, represen-tative from 198 returned the questionnaire, for a response rate of 14.2%. Close to two thirds of respondent pharmacies (65%) were located in an urban area of Ontario. Respondents reported that all pharmacies were open weekdays, almost all (95%) on Saturdays, and the overwhelming majority (82%) on Sundays. One out of 10 pharmacies was located more than a 15 minute drive from another pharmacy. We present demographic information about the pharmacies of our survey respondents in Table 1.
Survey participants’ knowledge of and attitudes toward the IUD as EC
Results from surveys indicate that pharmacists’ knowledge of the IUD as EC is limited. Survey respondents incorrectly re-sponded to the recommended timeframe for the post-coital insertion of the IUD, as well as the number of years for which the IUD could provide ongoing contraceptive benefit. Indeed, only 36% (n= 69) knew that the IUD could be used for up to 10 years. Our respondents correctly reported a Copper allergy as a contraindication to use (75%) but also incorrectly reported other contraindications, including history of ectopic pregnancy (45%). A significant minority (22%) incorrectly reported that use of the IUD increases the risk of ectopic pregnancy. Phar-macy representatives generally underestimated the efficacy of the IUD for both post-coital and ongoing pregnancy preven-tion; only 40% knew that the Copper IUD is the most effective EC modality. Finally, 14% of respondents (n=28) indicated that they lacked knowledge of the IUD as EC entirely. We detail these results in Table 2. Finally, survey participants expressed considerable interest in continuing education dedicated to EC (n=166, 86%) and nearly two thirds (n=122, 64%) reported that they would participate in a project dedicated to post-coital IUD referrals (data not shown).
Description of in-depth interview participants and their phar-macies
We conducted 17 IDIs with Ontario pharmacists, 15 in Eng-lish and two in French. The majority of our participants were women, worked in urban areas, and had been practicing for
UOJM | www.uojm.ca November 2017 | Volume 7 | Issue 2
30
Table 1. Characteristics of the pharmacies reported on by survey respondents (N=198)*Table 2. Survey respondents’ knowledge of the IUD as EC (N=198)*
RESEARCH
P a g e 4 | U O J M e P u b | J u n e 2 0 1 7R e s e a r c h
Characteristic n % Type of pharmacy (n=197**)† Independent Chain Banner 77 60 51 39 31 26 Region of the pharmacy (n=195)South Central East North 91 41 34 29 47 21 17 15 Location of pharmacy (n=197) Urban Rural 128 69 65 35 Other pharmacy located within a 15 minutes’ drive (n=198)
Yes No 180 18 91 9 Store Hours (n=198) Weekdays Saturdays Sundays 198 189 163 100 96 82 Table 1: Characteristics of the pharmacies reported on by survey respondents (N=198)*
*We have presented information contained in this table in a previous publication [19].
**The overall number of respondents was 198; however, the number provided denotes how many respondents answered that
particu-lar question.
†These questions included an “other” response that allowed participants to write-in information. We have not presented those results
in Table 1.
Knowledge statement Number and percentage of correct answers
n %
The IUD is the most effective modality of emergency contraception (n=188*) [Correct answer: Yes]
78 42
IUDs increase the risk of ectopic pregnancy (n=186) [Correct answer: No]
40 22
Both the Copper-T IUD and the levonorgestrel-releasing IUD (the Mirena®) can be used as EC (n=186)
[Correct answer: No]
100 54
In Ontario, the Copper-T IUD must be inserted by a physician (n=189) [Correct answer: Yes]
149 79
Table 2: Survey respondents’ knowledge of the IUD as EC (N=198)*
*We provide the number of responses to each question in parentheses and the correct answer to each knowledge statement in brack-ets. P a g e 4 | U O J M e P u b | J u n e 2 0 1 7
Re s e a rc h
Characteristic n % Type of pharmacy (n=197**)† Independent Chain Banner 77 60 51 39 31 26 Region of the pharmacy (n=195)South Central East North 91 41 34 29 47 21 17 15 Location of pharmacy (n=197) Urban Rural 128 69 65 35 Other pharmacy located within a 15 minutes’ drive (n=198)
Yes No 180 18 91 9 Store Hours (n=198) Weekdays Saturdays Sundays 198 189 163 100 96 82 Table 1: Characteristics of the pharmacies reported on by survey respondents (N=198)*
*We have presented information contained in this table in a previous publication [19].
**The overall number of respondents was 198; however, the number provided denotes how many respondents answered that
particu-lar question.
†These questions included an “other” response that allowed participants to write-in information. We have not presented those results
in Table 1.
Knowledge statement Number and percentage of correct answers
n %
The IUD is the most effective modality of emergency contraception (n=188*) [Correct answer: Yes]
78 42
IUDs increase the risk of ectopic pregnancy (n=186) [Correct answer: No]
40 22
Both the Copper-T IUD and the levonorgestrel-releasing IUD (the Mirena®) can be used as EC (n=186)
[Correct answer: No]
100 54
In Ontario, the Copper-T IUD must be inserted by a physician (n=189) [Correct answer: Yes]
149 79
Table 2: Survey respondents’ knowledge of the IUD as EC (N=198)*
*We provide the number of responses to each question in parentheses and the correct answer to each knowledge statement in brack-ets. P a g e 4 | U O J M e P u b | J u n e 2 0 1 7
R e s e a r c h
Characteristic n % Type of pharmacy (n=197**)† Independent Chain Banner 77 60 51 39 31 26 Region of the pharmacy (n=195)South Central East North 91 41 34 29 47 21 17 15 Location of pharmacy (n=197) Urban Rural 128 69 65 35 Other pharmacy located within a 15 minutes’ drive (n=198)
Yes No 180 18 91 9 Store Hours (n=198) Weekdays Saturdays Sundays 198 189 163 100 96 82 Table 1: Characteristics of the pharmacies reported on by survey respondents (N=198)*
*We have presented information contained in this table in a previous publication [19].
**The overall number of respondents was 198; however, the number provided denotes how many respondents answered that
particu-lar question.
†These questions included an “other” response that allowed participants to write-in information. We have not presented those results
in Table 1.
Knowledge statement Number and percentage of correct answers
n %
The IUD is the most effective modality of emergency contraception (n=188*) [Correct answer: Yes]
78 42
IUDs increase the risk of ectopic pregnancy (n=186) [Correct answer: No]
40 22
Both the Copper-T IUD and the levonorgestrel-releasing IUD (the Mirena®) can be used as EC (n=186)
[Correct answer: No]
100 54
In Ontario, the Copper-T IUD must be inserted by a physician (n=189) [Correct answer: Yes]
149 79
Table 2: Survey respondents’ knowledge of the IUD as EC (N=198)*
*We provide the number of responses to each question in parentheses and the correct answer to each knowledge statement in brack-ets.
UOJM | www.uojm.ca November 2017 | Volume 7 | Issue 2
31
2-10 years. We present basic demographic information in Table3. Seven pharmacists in the interview component of the study reported that they currently had a Copper-T IUD in stock; seven additional pharmacists reported that they did not have any type of IUD in stock but would order one on request.
Interviewees evinced limited knowledge of the IUD as EC Consistent with the findings from the survey, our interviewees were interested in the IUD as EC but generally lacked knowl-edge about this modality of post-coital contraception. Nine pharmacists were able to provide some information about the provision of an IUD as EC but had incomplete knowledge regarding the timeframe for use or the type of IUD that could be used. These pharmacists explained that they gained this knowledge on the job. As Pharmacist #8 commented, “I think that we did not cover this at all in school. As a recent grad, I remember exactly what happened. And we did not cover using IUDs as [emergency contraception].”
Participants were generally positive about the prospect of a “same day referral” program
Only one pharmacist in the interview component of the study had heard of efforts to provide “same day referrals.” However, once we described a hypothetical initiative, participants re-sponded positively. Pharmacists indicated the need for intro-ducing and promoting more effective EC methods in the prov-ince, efforts that could be supported with the introduction of a referral system. As Pharmacist #11 asserted, “Yes, like it is definitely an option for people to consider…probably have a higher chance of preventing pregnancy…a prime over Plan B®.” Several interviewees also noted the advantages of having an
automatic bridge to an ongoing contraceptive that is more ef-fective than daily oral contraceptive pills.
All of our interviewees expressed the view that community pharmacists are accessible health service professionals and excellent resources for patients seeking information and ad-vice. Participants practicing in smaller communities and rural areas noted that sometimes pharmacists in these settings are the only accessible provider. As a consequence, interviewees felt that pharmacists, once trained and informed, were well positioned to participate in a referral program and facilitate in-creased access to timely IUD insertion by working with clinics and physicians.
Perceived facilitators and barriers to same day referrals
Interviewees believed that pharmacists have the appropriate skills, in general, to participate in a “same day referral” program. A number of participants specifically mentioned that pharma-cists already serve as trained and autonomous health service professionals and are well-positioned to initiate discussions, counsel patients, and ultimately make referrals. As explained by Pharmacist #7, “That sort of thing, [that] is a huge role for pharmacists that we already do. We have the knowledge and we have the expertise to be able to educate people about [the IUD as EC]…and we are accessible and have the resources.” In-terviewees view pharmacists as having key responsibilities in educating, counseling, and screening potential patients; some interviewees also noted that pharmacists could play an impor-tant role in following-up with the patient once the IUD was in-serted.
However, our interviewees also perceived that there would be a number of barriers to implementing an initiative in Ontario. Our interviewees noted that for a program to be effective, rais-ing awareness of the initiative, among pharmacists and physi-cians, would be required and appropriate screening tools and continuing education resources would need to be developed. Pharmacists suggested that an educational letter in the month-ly Canadian Pharmacist’s Letter could be an important initial step. However, pharmacists also expressed concern that the lack of qualified personnel to perform the insertion—and to do so in a timely way—would be a barrier to implementation; this issue was especially salient for our rural participants. Interview-ees also felt that the considerable lack of awareness about the IUD, in general, and the IUD as EC, in particular, among women in the general population, as well as the high up-front costs as-Table 3. Demographic information of IDI participants (N=17)
RESEARCH
UOJM | www.uojm.ca November 2017 | Volume 7 | Issue 2
RESEARCH
5
3. Seven pharmacists in the interview component of the study reported that they currently had a Copper-T IUD in stock; seven additional pharmacists reported that they did not have any type of IUD in stock but would order one on request.
Interviewees evinced limited knowledge of the IUD as EC Consistent with the findings from the survey, our interviewees were interested in the IUD as EC but generally lacked knowl-edge about this modality of post-coital contraception. Nine pharmacists were able to provide some information about the provision of an IUD as EC but had incomplete knowledge regarding the timeframe for use or the type of IUD that could be used. These pharmacists explained that they gained this knowledge on the job. As Pharmacist #8 commented, “I think that we did not cover this at all in school. As a recent grad, I remember exactly what happened. And we did not cover using IUDs as [emergency contraception].”
Participants were generally positive about the prospect of a “same day referral” program
Only one pharmacist in the interview component of the study had heard of efforts to provide “same day referrals.” However, once we described a hypothetical initiative, participants re-sponded positively. Pharmacists indicated the need for intro-ducing and promoting more effective EC methods in the prov-ince, efforts that could be supported with the introduction of a referral system. As Pharmacist #11 asserted, “Yes, like it is definitely an option for people to consider…probably have a higher chance of preventing pregnancy…a prime over Plan B®.” Several interviewees also noted the advantages of having an automatic bridge to an ongoing contraceptive that is more
ef-fective than daily oral contraceptive pills.
All of our interviewees expressed the view that community pharmacists are accessible health service professionals and excellent resources for patients seeking information and ad-vice. Participants practicing in smaller communities and rural areas noted that sometimes pharmacists in these settings are the only accessible provider. As a consequence, interviewees felt that pharmacists, once trained and informed, were well positioned to participate in a referral program and facilitate in-creased access to timely IUD insertion by working with clinics and physicians.
Perceived facilitators and barriers to same day referrals
Interviewees believed that pharmacists have the appropriate skills, in general, to participate in a “same day referral” program. A number of participants specifically mentioned that pharma-cists already serve as trained and autonomous health service professionals and are well-positioned to initiate discussions, counsel patients, and ultimately make referrals. As explained by Pharmacist #7, “That sort of thing, [that] is a huge role for pharmacists that we already do. We have the knowledge and we have the expertise to be able to educate people about [the IUD as EC]…and we are accessible and have the resources.” In-terviewees view pharmacists as having key responsibilities in educating, counseling, and screening potential patients; some interviewees also noted that pharmacists could play an impor-tant role in following-up with the patient once the IUD was in-serted.
However, our interviewees also perceived that there would be a number of barriers to implementing an initiative in Ontario. Our interviewees noted that for a program to be effective, rais-ing awareness of the initiative, among pharmacists and physi-cians, would be required and appropriate screening tools and continuing education resources would need to be developed. Pharmacists suggested that an educational letter in the month-ly Canadian Pharmacist’s Letter could be an important initial step. However, pharmacists also expressed concern that the lack of qualified personnel to perform the insertion—and to do so in a timely way—would be a barrier to implementation; this issue was especially salient for our rural participants. Interview-ees also felt that the considerable lack of awareness about the IUD, in general, and the IUD as EC, in particular, among women in the general population, as well as the high up-front costs
as-P a g e 5 | U O J M e P u b | J u n e 2 0 1 7
system. s Pharmacist 11 asserted, “Yes, like it is de nitely an option for people to consider probably have a higher chance of preventing pregnancy a prime over Plan B®.” Several interview-ees also noted the advantages of having an automatic bridge to an ongoing contraceptive that is more effective than daily oral contraceptive pills.
ll of our interviewees e pressed the view that community phar-macists are accessible health service professionals and e cellent resources for patients seeking information and advice. Partici-pants practicing in smaller communities and rural areas noted that sometimes pharmacists in these se ngs are the only acces-sible provider. s a consequence, interviewees felt that pharma-cists, once trained and informed, were well positioned to par-ticipate in a referral program and facilitate increased access to timely IUD insertion by working with clinics and physicians.
Perceived facilitators and barriers to same day referrals
Interviewees believed that pharmacists have the appropriate skills, in general, to participate in a “same day referral” program. number of participants speci cally mentioned that pharma-cists already serve as trained and autonomous health service professionals and are well-positioned to initiate discussions, counsel patients, and ultimately make referrals. s e plained by Pharmacist 7, “That sort of thing, [that] is a huge role for phar-macists that we already do. We have the knowledge and we have the e pertise to be able to educate people about [the IUD as EC] and we are accessible and have the resources.” Interview-ees view pharmacists as having key responsibilities in educating, counseling, and screening potential patients; some interviewees also noted that pharmacists could play an important role in fol-lowing-up with the patient once the IUD was inserted.
However, our interviewees also perceived that there would be a number of barriers to implementing an initiative in Ontario.
Our interviewees noted that for a program to be effective, rais-ing awareness of the initiative, among pharmacists and physi-cians, would be required and appropriate screening tools and continuing education resources would need to be developed. Pharmacists suggested that an educational le er in the monthly Canadian Pharmacist’s Le er could be an important initial step. However, pharmacists also e pressed concern that the lack of quali ed personnel to perform the insertion and to do so in a timely way would be a barrier to implementation; this issue was especially salient for our rural participants. Interviewees also felt that the considerable lack of awareness about the IUD, in general, and the IUD as EC, in particular, among women in the general population, as well as the high up-front costs associated with IUD insertion, would constitute signi cant barriers.
C N
E panding access to emergency contraception in Canada has long been identi ed as a priority among reproductive health and rights stakeholders [8,11,20]. urther, in recent years there has been a plethora of efforts in North merica to e pand access to long-acting, reversible contraception [21 23]. Misinformation among providers, a dearth of trained providers, high up-front costs, and lack of awareness among women have limited the availability and accessibility of IUDs, both as ongoing methods of contraception and as EC [24-26]. Yet research also suggests that when women are informed about the IUD as EC, demand increases [27].
Our ndings suggest that creation of a “same day referral” initia-tive in Ontario could be a viable rst step in e panding access to more effective modalities of EC. lthough pharmacists in both components of our study had relatively limited knowledge of the IUD as EC, a nding that is consistent with other studies of health professionals in North merica [25], our participants e pressed considerable interest in participating in such an initiative. Im-portantly, pharmacists saw themselves as being well-positioned to offer these types of referrals and identi ed that this type of program would meet a demonstrable need. lthough content-speci c information would need to be developed to ensure that pharmacists provided women with accurate information, phar-macists in our study feel con dent in their ability to leverage their overarching skills in educating, counseling, and referring patients. Creating a pilot initiative modelled a er the BC initia-tive as a proof of concept appears warranted.
However, even in the absence of a dedicated “same day refer-ral” program, our ndings suggest that developing continuing education resources and training modules for pharmacists would be well received. Our survey participants indicated considerable enthusiasm for participating in such efforts and our interviewees further elaborated on potential avenues for disseminating
infor-R e s e a r c h
Characteristic n ender emale Male 12 (71) 5 (39) Number of years working in a pharmacy<2 2 5 6 10 >10 2 (12) 8 (47) 6 (35) 1 (6) Location of current pharmacy
Urban Rural
11 (65) 6 (35) Table : Demographic information of IDI participants (N=17) Table 2. Demographic information of IDI participants (N=17)
UOJM | www.uojm.ca November 2017 | Volume 7 | Issue 2
32
sociated with IUD insertion, would constitute significantbarri-ers.
DISCUSSION
Expanding access to emergency contraception in Canada has long been identified as a priority among reproductive health and rights stakeholders [8,11,20]. Further, in recent years there has been a plethora of efforts in North America to expand ac-cess to long-acting, reversible contraception [21-23]. Misinfor-mation among providers, a dearth of trained providers, high up-front costs, and lack of awareness among women have lim-ited the availability and accessibility of IUDs, both as ongoing methods of contraception and as EC [24-26]. Yet research also suggests that when women are informed about the IUD as EC, demand increases [27].
Our findings suggest that creation of a “same day referral” ini-tiative in Ontario could be a viable first step in expanding ac-cess to more effective modalities of EC. Although pharmacists in both components of our study had relatively limited knowl-edge of the IUD as EC, a finding that is consistent with other studies of health professionals in North America [25], our par-ticipants expressed considerable interest in participating in such an initiative. Importantly, pharmacists saw themselves as being well-positioned to offer these types of referrals and iden-tified that this type of program would meet a demonstrable need. Although content-specific information would need to be developed to ensure that pharmacists provided women with accurate information, pharmacists in our study feel confident in their ability to leverage their overarching skills in educating, counseling, and referring patients. Creating a pilot initiative modelled after the BC initiative as a proof of concept appears warranted.
However, even in the absence of a dedicated “same day refer-ral” program, our findings suggest that developing continu-ing education resources and traincontinu-ing modules for pharmacists would be well received. Our survey participants indicated con-siderable enthusiasm for participating in such efforts and our interviewees further elaborated on potential avenues for dis-seminating information. Our interviewees, even those who had recently completed their training, indicated that coverage of EC in pharmacy education is lacking. Further research could be conducted to assess the coverage of EC in pharmacy training programs and explore ways of strengthening this area of the curriculum, if needed.
Our study has a number of limitations. First, our survey response rate of 14.2% is low and thus our results should be viewed as exploratory. Second, although we administered the survey in both French and English and oversampled pharmacies in Franco-Ontarian communities, we had very few participants in both components who were based in language-minority areas. Future research would benefit from inclusion of these perspec-tives. Finally, reproductive health is an evolving field. We com-pleted our data collection in the fall of 2015; efforts undertaken in the last 15 months would therefore not be captured in our study.
Despite these limitations, our study offers insights into the knowledge, attitudes, and practices of Ontario pharmacists to-ward the IUD as EC and points to several avenues for improving access to a full range of contraceptive services. The enthusiasm among pharmacists for the development of a “same day referral” program is encouraging and the facilitators and barriers iden-tified by our interviewees could inform this type of effort. En-gaging with a range of stakeholders to build upon these results and explore creative educational, training, and service delivery initiatives appears warranted.
ACKNOWLEDGEMENTS
Andréanne Chaumont received a Queen Elizabeth II Graduate Scholarship in Science and Technology and several grants from the University of Ottawa to support this project. Dr. Foster’s 2011-2016 Endowed Chair in Women’s Health Research was funded by the Ontario Ministry of Health and Long-Term Care and the funding attached to her Chair covered the costs associ-ated with this study. We are also grateful to the Society of Family Planning for its support of Dr. Foster’s mentorship activities. We would like to thank Drs. Raywat Deonandan and Karen Phillips for their feedback during various phases of this project and Dr. Sheila Dunn for providing us with her survey instrument. We are also grateful to the team of volunteers for their efforts. The con-clusions and opinions expressed in this article are those of the authors and do not necessarily represent the views of the orga-nizations with which the authors are affiliated or the funders. REFERENCES
1. Fisher W, Boroditsky R, Morris B. The 2002 Canadian contraception study: part 1. J Obstet and Gynaecol Can. 2004;26(6):580-90.
2. Peipert JF, Zhao Q, Allsworth JE, et al. Continuation and satisfaction of re-versible contraception. Obstet Gynecol. 2011;117:1105-13.
3. Trussell J. Emergency contraception: hopes and realities. Chapter in Emer-gency contraception: the story of a global reproductive health technology AM Foster & LL Wynn (Eds). New York, NY: Palgrave Macmillan; 2012. 20-35.
UOJM | www.uojm.ca November 2017 | Volume 7 | Issue 2
33
4. Black A, Guilbert E. Canadian contraception consensus: part 1. J Obstet and Gynaecol Can. 2015;37(10):936-8.
5. Cleland K, Zhu H, Goldstuck N, Cheng L, Trussell J. The efficacy of intrauter-ine devices for emergency contraception: a systematic review of 35 years of experience. Hum Reprod. 2012; 27(7):1994-2000.
6. Sivin I. Utility and drawbacks of continuous use of copper T IUC for 20 years. Contraception. 2007;74(6):1102-7.
7. Dunn S, Anderson GM, Bierman AS. Temporal and regional trends in IUD insertion: a population-based study in Ontario, Canada. Contraception. 2009;80(5):469-73.
8. Wier E. Preventing pregnancy: a fresh look at the IUD. CMAJ. 2003;169(6):585. 9. Goertzen J. Learning procedural skills in family medicine: comparison of
rural and urban programs. Can Fam Physician. 2006;52:622-3.
10. Soon J, Levine M, Osmond, B Ensom M, Fielding D. Effects of making emer-gency contraception available without a physician’s prescription: a popula-tion-based study. CMAJ. 2005;172(7):878-83.
11. Dunn S, Brown TE, Alldred J. Availability of emergency contraception after its deregulation from prescription-only status: a survey of Ontario pharma-cies. CMAJ. 2008;178(4):423-4.
12. Eggertson L, Sibbald B. Privacy issues raised over Plan B: women asked for names, addresses, sexual history. CMAJ. 2005;173(12):1435-6.
13. Erdman J. Canada: competing frames of access and authority. In A Foster & L Wynn (eds.), Emergency contraception: the story of a global reproductive health technology. New York: Palgrave Macmillan; 2012. 57-78 p.
14. Wynn L, Erdman J, Foster A, Trussell J. Harm reduction or women’s rights? Debating access to emergency contraceptive pills in Canada and the Unit-ed States. Stud Fam Plann. 2007;38(4):253-67.
15. Health Canada. Emergency contraceptive pills to carry warnings for re-duced effectiveness in women over a certain body weight [Internet]. Gov-ernment of Canada; 2014 [cited 2017 March 25]. Available from: http:// healthycanadians.gc.ca/recall-alert-rappel-avis/hc-sc/2014/38701a-eng. php.
16. Health Canada. Health product info watch - product monograph and medi-cal device instructions for use updates [Internet]. November 2015 [cited: 2016 March 28]. Available from: www.hcsc.gc.ca/dhpmps/medeff/bulletin/ hpiw-ivps_2015-11-eng.php#j.
17. Wiebe E, Soon J, Trouton K. Increasing the use of copper intrauterine de-vices (IUDs) for emergency contraception. Presentation at the 2015 North American Forum on Family Planning, Chicago, IL: Nov 13-16, 2015. 18. Options for Sexual Health. EC-IUD rapid access network [Internet]. Options
for Sexual Health; 2017 [cited 2017 March 25]. Available from: http://www. emergencyiud.com/.
19. Chaumont A, Foster A. The not so over-the-counter status of emergency contraception in Ontario: a mixed-methods study with pharmacists. FAC-ETS. 2017;2:1-11.
20. Black A, Guilbert E. Canadian contraception consensus (part 1 of 4). J Ob-stet and Gynaecol Can. 2015;37(10):936-8.
21. Luchowski AT, Anderson BL, Power ML, Rglan GB, Espey E, Schulkin J. Obste-trician-gynecologists and contraception: practice and opinions about the use of IUDs in nulliparous women, adolescents and other patient popula-tions. Contraception. 2014;89(6):572-7.
22. Cristobal I, Neyro JL, Lete I. The new LNG-releasing IUS: a new opportunity to reduce the burden of unintended pregnancy. Eur J Obstet Gynecol Re-prod Biol. 2015;190:58-64.
23. Hall KS, Ela E, Zochowski MZ, et al. “I don’t know enough to feel comfort-able using them:” women’s knowledge of and perceived barriers to long-acting reversible contraceptives on a college campus. Contraception. 2016; 93(6):556-64.
24. Haper CC, Speidel JJ, Drey EA, Trussell J, Blunn M, Darney PD. Copper in-traunterine device of emergency contraception: clinical practice among contraceptive providers. Obstet Gynecol. 2012;199(2 Pt 1):200-6.
25. Batur P, Cleland K, McNamara M, Wu J, Pickle S, EC Survey Group. Emer-gency contraception: a multispecialty survey of clinician knowledge and practices. Contraception. 201693(2):145-52.
26. Broecker J, Jurich J, Fuchs R. The relationship between long-acting
revers-ible contraception and insurance coverage: a retrospective analysis. Con-traception. 2016;93(3):266-72.
27. Turok DK, Gurtcheff SE, Handley E, et al. A survey of women obtaining emergency contraception: are they interested in using the copper IUD?. Contraception. 2011;83(5):441-6.