Reflective debriefing to promote novice nurses' clinical judgment after high-fidelity clinical simulation : a pilot test
Texte intégral
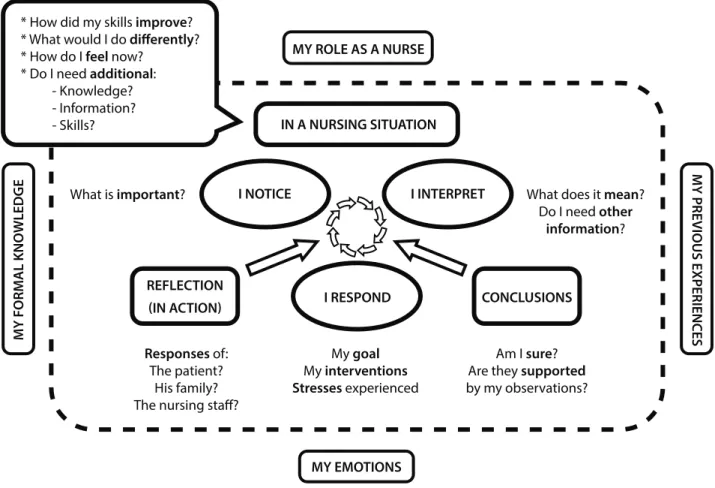
Figure
Documents relatifs
Of the 165 questionnaires distributed, 25 responses met the criteria to be included in the study. Although, the incidence of critical incidents among home care nurses is
Published in "Swiss Journal of Geosciences 111(3): 511–522, 2018" which should be cited to refer to this work... investigating planktonic foraminifera from Miocene to
The aim of this study is (a) to investigate timing and emotional valence of experienced normative and silent transitions of middle-aged persons, and (b) to discover the impact of
In the Baum-Douglas approach to the index theorem, the com- putation of the Fredholm index of an elliptic pseudodifferential operator on a compact closed manifold can be reduced to
The objectives of the literature review were to review and examine the existing literature regarding current debriefing practice guidelines for high fidelity simulation- based
It was evident from a review of the literature and consultations with nurses and key stakeholders that there is a need for novice nurses working on the surgical unit to have
The development of a teaching resource manual can be utilized for cannulation skill acquisition for novice registered nurses and assist in increasing overall knowledge while
There is limited research that supports the use of high fidelity human patient simulation (HF- SICE) as a teaching learning approach to enhance interprofessional collaboration