Duplex sonographic registration of age and diabetes‐related loss of renal vasodilatory response to nitroglycerine
Texte intégral
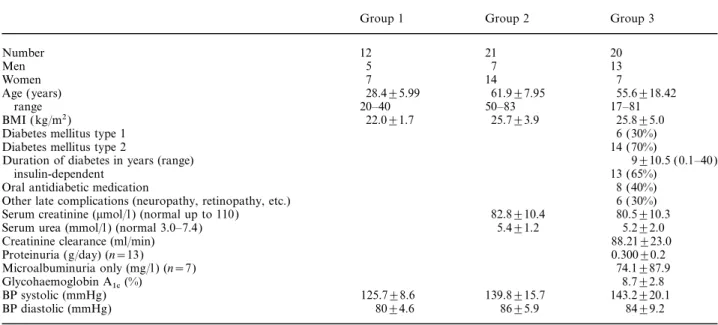
(2) 828. been shown as a function of creatinine clearance, age, and duration of diabetes in cases of diabetic nephropathy [10]. The aim of this study was threefold: firstly to find out whether duplex ultrasonography could be used to detect the changes in renal haemodynamics after administration of nitroglycerine, secondly to ascertain the parameters on which any change in these resistive indices is dependent, and thirdly to determine whether the change in resistance is less evident in patients with diabetic nephropathy because of the existing arteriolar dilatation caused by NO, mentioned above.. Patients and methods Patients The study, which was approved by the Ethics Commission, included 53 healthy volunteers and patients between October 1996 and December 1999. The volunteers and patients were divided into three different groups. The following inclusion and exclusion criteria were used. For all groups, written declaration of consent and current good health was required. Group 1, young, healthy volunteers: aged between 16 and 40 years, no history of or clinical indications of kidney disease. Exclusion criteria were arterial hypertension (values detected before, during and 24 h after duplex ultrasonography of over 150 mmHg systolic and 95 mmHg diastolic), smoking, diabetes mellitus, taking any medication except for hormonal contraceptives, and a kidney size of less than 9 cm. Twelve volunteers were finally included, the relevant characteristics of whom are listed in Table 1. Group 2, older, healthy volunteers: aged between 50 and 85 years, no history or clinical indications of kidney disease. Exclusion criteria were arterial hypertension, smoking, diabetes mellitus, any current medication, with the exception of hormone replacement therapy, serum creatinine. B. Frauchiger et al.. >120 mmol/l, urea >8.5 mmol/l, pathological urinanalysis (Combur 10A, Boehringer Mannheim, Germany), and kidney size of less than 9 cm, or morphological abnormalities detectable with duplex ultrasonography. Three volunteers were excluded from this group. Twenty-one volunteers were included and the patient characteristics are again shown in Table 1. Group 3, patients with diabetic nephropathy: diabetes mellitus type 1 or 2 [11], age 17–81 years, mild to moderate proven nephropathy (serum creatinine <120 mmol/l, serum urea <8.5 mmol/l ), combined with proteinuria, either detected as macroalbuminuria >0.04–1.0 g/24 h (PrecisetA U/CSF Protein, photometric determination of protein after precipitation with trichloroacetic acid, Boehringer Mannheim, Germany), or, if the Preciset test was negative, as microalbuminuria, inclusion value >20 mg/l ( TurbiquantB, photometric determination of the albumins on immunochemical reaction with specific antibody, detection limit 6 mg/l, Behring Diagnostik GmbH, Germany). Exclusion criteria were unstable diabetic metabolic status with blood glucose values of <4 or more than 15 mmol/l in the 48 h immediately prior to duplex ultrasonography, arterial hypertension, treatment with antihypertensives (exception, diuretics for mild heart failure), treatment with ACE inhibitors, prostaglandin synthesis inhibitors (exception: acetylsalicylic acid, 100 mg/day), smoking, creatinine clearance below 50 ml/min/1.73 m2 (determined by the Cockcroft formula [12]), kidney size less than 9 cm, or morphological abnormalities detected with duplex ultrasonography. An orientational preliminary selection yielded primarily 36 possible patients, 20 of these were included in the study. The chronic medication prescribed for seven patients (platelet aggregation inhibitors, diuretics, beta blockers) was stopped at least 24 h prior to the duplex ultrasonographic investigation and were not given again until after the ultrasonography. The patients’ characteristics are shown in Table 1.. Duplex ultrasonographic measurements before and after administration of nitroglycerine The measurements were commenced after 10 min rest in a horizontal position. All the examinations were performed by. Table 1. Patient data. Number Men Women Age (years) range BMI (kg/m2) Diabetes mellitus type 1 Diabetes mellitus type 2 Duration of diabetes in years (range) insulin-dependent Oral antidiabetic medication Other late complications (neuropathy, retinopathy, etc.) Serum creatinine (mmol/l ) (normal up to 110) Serum urea (mmol/l ) (normal 3.0–7.4) Creatinine clearance (ml/min) Proteinuria (g/day) (n=13) Microalbuminuria only (mg/l ) (n=7) Glycohaemoglobin A (%) 1c BP systolic (mmHg) BP diastolic (mmHg) Data are expressed as the mean±SD.. Group 1. Group 2. Group 3. 12 5 7 28.4±5.99 20–40 22.0±1.7. 21 7 14 61.9±7.95 50–83 25.7±3.9. 20 13 7 55.6±18.42 17–81 25.8±5.0 6 (30%) 14 (70%) 9±10.5 (0.1–40) 13 (65%) 8 (40%) 6 (30%) 80.5±10.3 5.2±2.0 88.21±23.0 0.300±0.2 74.1±87.9 8.7±2.8 143.2±20.1 84±9.2. 82.8±10.4 5.4±1.2. 125.7±8.6 80±4.6. 139.8±15.7 86±5.9.
(3) Age and diabetes-related loss of renal vasodilatory response to nitroglycerine. two experienced investigators (BF, PN ) with an Acuson 128 XP 10 ultrasound unit (Acuson Corporation, Mountainview, CA, USA) using a 3.5 MHz or 4 MHz vector array transducer with wall-filter setting of 50 Hz. After recording pulse and blood pressure, the first measurement was the size of the left and right kidney. For orientation purposes, perfusion in the whole of the left and right kidneys was then checked using colour duplex ultrasonography and the main trunk of the renal artery was displayed. If the orientational duplex ultrasonography did not reveal any abnormalities in size or perfusion, three measurements each were taken within 5 min in the vicinity of the interlobar artery at the boundary of the centre of the kidney and the upper pole on the right side, using pulsed Doppler. To this end, the pulsed Doppler measured volume was located in the interlobar artery and the Doppler angle corrected in accordance with the course of the artery (a maximum of 60°). The maximum systolic and minimum diastolic flow rate was recorded in centimetres per second. Subsequent to these first three measurements, the volunteers or patients were given two puffs of sublingual nitroglycerine (2×0.4 mg glyceryl trinitrate, NitrolingualA Spray, Pohl-Boskamp, Germany). A first Doppler measurement was taken 1 min after administration and repeated after 3 and 5 min at the same place. Pulse and blood pressure were measured again 3 min after administering the drug. Any adverse reactions were noted.. Calculation of the resistance parameters The resistive index (RI ) according to Pourcelot [13] was calculated on the basis of the following formula: 1−. minimal diastolic velocity peak systolic velocity. Since all the pulse measurements were between 52 and 90 beats per minute, the correction recommended by Mostbeck et al. for bradycardic or tachycardic values was not implemented [14].. Accuracy To determine the accuracy of the RI measurements in our laboratory, we performed on 10 healthy volunteers an intraand interobserver variability test with two blinded investigators. The two measurements were taken within 1 week and revealed an intraobserver variability of 3.5 and 5.1% respectively, and an interobserver variability of 4.7%.. 829. Results RI before and after administration of nitroglycerine Table 2 shows an overview of all values of all groups. Differences between groups 1, 2 and 3 The starting RI and DRI values differed significantly between groups 1 and 3 (P<0.01 and. P<0.001 respectively). RI and RI reduction differed significantly also between groups 1 and 2 (P<0.01 and P<0.02 respectively) but not between groups 2 and 3 (P= 0.071 and P=0.077 respectively). If all healthy volunteers were compared to all DN patients (n=33 vs 20, age 50±18 vs 56±18 years, n.s.) again significant differences for RI and DRI were found (0.616±0.042 vs 0.669±0.086 before, DRI 7.7 vs 3.4% after nitroglycerine, P<0.005 for initial RI and P<0.003 for DRI ). Figure 1 illustrates the different response to nitroglycerine in diabetic nephropathy patients compared to the healthy volunteers. The starting RI and DRI as a function of various parameters Table 3 shows the different factors influencing starting RI and DRI. Significant correlations exist between age and RI and DRI in healthy subjects, between age and RI and creatinine clearance and RI in diabetic nephropathy, and between duration of diabetes and DRI. Pulse and blood pressure behaviour As was expected, the systolic blood pressure in group 1 fell slightly but significantly by 3.4% after administration of nitroglycerine (P<0.01). Among the healthy older subjects, the decrease in blood pressure was slightly more marked with respect to systolic pressure, at 4.3% (P<0.01); the diastolic decrease was not significant. In the patients with nephropathy, nitroglycerine caused a decrease in blood pressure of 3.0%, n.s.; the decrease in diastolic pressure of 0.3% was also not significant. In none of the groups was pulse statistically affected.. Discussion Statistical analysis Data input, basic evaluations, and graphic representations were carried out using Excel 97 table calculation program (MicrosoftA Corporation, Bellevue, WA, USA). The Statistical Package for the Social Sciences (SPSSA Inc. Chicago, IL, USA) was used for more detailed statistical calculations. The data were checked for normal distribution (Q-Q plot) and combined as mean±SD. One-way ANOVA was used to calculate the differences between groups 1, 2 and 3. The paired t-test was used for analysis of the values before and after administration of nitroglycerine within the same group. Correlation calculations were performed using Pearson’s test and multiple linear regression. The null hypothesis was tested at the significance level P<0.05.. Our study shows that haemodynamic changes in renal perfusion occur after sublingual administration of nitroglycerine, which can be detected using duplex ultrasonography. The differences in this reaction to medication found between young and older volunteers and patients with diabetic nephropathy are remarkable. The parameter used in this paper to grade the intrarenal resistance, resistive index, or RI, represents the intrarenal resistance downstream of the measuring site and is the easiest of all the known resistance parameters to record [8]. The reproducibility of the RI measurements is demonstrated by our own intraand interobserver variability results and data in the.
(4) 0.022 (±0.020) <0.01. 0.038 (±0.033) <0.01. <0.01. <0.01. <0.01. 0.528±0.036 (−10.8±2.8) 0.593±0.046 (−5.9±5.1) 0.647±0.091 (−3.4±3.0) <0.01. NS. NS 0.631 (±0.040). 0.669 (±0.086). 2 (n=21). 3 (n=20). 0.536±0.055 (−9.5±7.4) 0.615±0.052 (−2.4±6.6) 0.662±0.092 (−0.9±5.8) 0.592 (±0.033) 1 (n=12). *Compared with value prior to nitroglycerine administration.. <0.01. <0.01. 0.515±0.041 (−13.0±4.1) 0.579±0.047 (−8.1±6.2) 0.634±0.091 (−5.3±5.1) 0.529±0.039 (−10.5±4.3) 0.577±0.058 (−8.6±7.3) 0.642±0.102 (−4.3±4.8) <0.01. <0.01. P* RI 1 min, 3 min, 5 min mean value (% reduction) P* RI 5 min after (% reduction) P* RI 3 min after (% reduction) P* RI 1 min after (% reduction) RI before Group. Table 2. RI (mean±SD) before and 1, 3 and 5 min after nitroglycerine administration. 0.064 (±0.016). B. Frauchiger et al.. DRI mean value. 830. literature [6,15]. Despite the small absolute values of DRI, the relative reduction of 50% and more between our different groups yields clear statistical results. The starting values we recorded in our healthy volunteers compare well with figures from the literature. A statistically significant correlation between age and RI was found in this population. This relationship is known [16,17]. Blood pressure also correlates with age in these subjects. This fact was recently confirmed by Jacquet et al. in a larger population [18]. It is possible that the increased resistance parameter already represents arteriolar dysfunction or minimal arteriolar damage, even in older subjects who are still normotensive by definition. The phenomena observed after administration of sublingual nitroglycerine are particularly interesting. We know of no study to date which has used duplex ultrasonography to investigate the influence on renal haemodynamics of this drug, which is frequently administered for cardiac indications. The rapid change in RI corresponds to the known rapid cardiac effect, which can be expected within 1–3 min [1]. The action measured by the fall in RI can probably be explained by a reduction in the tension of the resistive vessels, i.e. the afferent arterioles. The direct effects of this dilatation on the vas afferens are only partially known. In the rat kidney, nitroglycerine leads to increased renal plasma flow with a non-significant increase in glomerular filtration rate [19]. Inhibition of sodium transport by nitric oxide also results in increased elimination of sodium in the urine [20]. Bank and Aynedjian, in 1993, showed that inhibition of nitric oxide synthesis in healthy rat kidneys results in both a decrease in renal blood flow and in a reduction in the glomerular filtration rate [21]. Although it remains hypothetical in the final analysis, it could well be assumed that by lowering resistance at the vas afferens, nitroglycerine probably contributes to increased renal blood flow, increased glomerular filtration, and increased natriuresis. The clinical significance of this mechanism remains unknown at present. In comparison with the healthy subjects, patients with mild diabetic nephropathy exhibit a limited reactivity to nitroglycerine, which depends on the duration of the diabetes. However, in addition the starting RI values are to be higher, thus confirming the results obtained by Ishimura et al. [10]. We presume that the higher starting RI as well as the decreased DRI in patients at an early stage of nephropathy are influenced more by ultrastructurally probable glomerular damage and perhaps arteriolosclerosis than by pre-existing submaximal vasodilatation by nitric oxide [10,22]. It is worth noting that the RI decrease in the diabetic subjects does not depend on chronological age but on the duration of the diabetes. This is a further indication of a disease-specific restriction of responsiveness to nitroglycerine. The existing figures in the literature for resistive indices in healthy volunteers and also in cases of diabetic nephropathy were confirmed. Although the clinical significance is actually unknown, the study.
(5) Age and diabetes-related loss of renal vasodilatory response to nitroglycerine. 831. Fig. 1. Comparison of initial RI ( left) and DRI (right) in all healthy volunteers (1, n=33) and in patients with nephropathy (2, n=20). Table 3. Dependency of RI and DRI on different factors Factor. DRI. RI k*. Healthy volunteers (n=33) Age Systolic blood pressure Difference of syst. blood pressure before and after nitroglycerine Patients with nephropathy (n=20) Age Systolic blood pressure Difference of syst. blood pressure before and after nitroglycerine Creatinine clearance Duration of diabetes. P*. k*. P*. 0.418 0.179. 0.024 0.316. −0.548 0.007 0.042. 0.004 0.97 0.797. 0.553 0.002. 0.017 0.991. −0.568 −0.014 0.316. 0.102 0.963 0.178. −0.401 −0.028. 0.047 0.848. −0.366 −0.542. 0.204 0.024. *Multiple linear regression.. reveals additional interesting phenomena of renal haemodynamics induced by nitroglycerine. Furthermore, it proves that duplex ultrasonography is also suitable for recording changes during therapy or in physiological studies.. 2. 3. 4.. Acknowledgements. We would like to offer our sincere thanks for the secretarial work of Esther Brandner. 5.. References 6. 1. Robertson RM, Robertson D. Drugs used for the treatment of myocardial ischemia. In: Hardman JG, Limbird LE, Molinoff PB, Ruddon RW, Gilman AG eds Goodman and Gilman’s The. 7.. Pharmacological Basis of Therapeutics. McGraw-Hill, Inc., New York, 1996; 759–779 Harrison DG, Bates JN. The nitrovasodilators. New ideas about old drugs. Circulation 1993; 87: 1461–1467 Lowenstein CJ, Dinerman JL, Snyder SH. Nitric oxide: a physiologic messenger. Ann Intern Med 1994; 120: 227–237 Yamada K, Nakano H, Nakayama M et al. Endotheliumdependent relaxation in peripheral vasculature and kidney of non-insulin-dependent diabetes mellitus. J Diabetes Complications 1995; 9: 203–207 Komers R, Allen TJ, Cooper ME. Role of endothelium-derived nitric oxide in the pathogenesis of the renal hemodynamic changes of experimental diabetes. Diabetes 1994; 43: 1190–1197 Krumme B, Blum U, Schwertfeger E et al. Diagnosis of renovascular disease by intra- and extrarenal Doppler scanning. Kidney Int 1996; 50: 1288–1292 Mastorakou I, Robbins ME, Bywaters T. Resistance and pulsat-.
(6) 832. 8.. 9.. 10. 11. 12. 13. 14.. B. Frauchiger et al. ility Doppler indices: how accurately do they reflect changes in renal vascular resistance. Br J Radiol 1993; 66: 577–580 Frauchiger B, Bock A, Eichlisberger R et al. The value of different resistance parameters in distinguishing biopsy-proved dysfunction of renal allografts. Nephrol Dial Transplant 1995; 10: 527–532 Frauchiger B, Zierler R, Bergelin RO, Isaacson JA, Strandness DE Jr. Prognostic significance of intrarenal resistance indices in patients with renal artery interventions: a preliminary duplex sonographic study. Cardiovasc Surg 1996; 4: 324–330 Ishimura E, Nishizawa Y, Kawagishi T et al. Intrarenal hemodynamic abnormalities in diabetic nephropathy measured by duplex Doppler sonography. Kidney Int 1997; 51: 1920–1927 WHO Study Group on Diabetes Mellitus. Diabetes Mellitus, Report of a WHO Study Group. ( Technical Report Series 727), World Health Organization, Geneva, 1985 Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron 1976; 16: 31–41 Pourcelot L. Applications cliniques de l’examen Doppler transcutane. In: Peronneau P ed. Velocimetrie Ultrasonore Doppler. INSERM, Paris, 1975; 213–240 Mostbeck GH, Goessinger HD, Mallek R, Siostrzonek P, Schneider B, Tscholakoff D. Effect of heart rate on Doppler measurements of resistive index in renal arteries. Radiology 1990; 175: 511–513. 15. Rasmussen K. Non-invasive quantitative measurements of blood flow and estimation of vascular resistance by Doppler ultrasound method. Dan Med Bull 1992; 39: 1–14 16. Brkljacic B, Mrzljak V, Drinkovic I, Soldo D, SabljarMatovinovic M, Hebrang A. Renal vascular resistance in diabetic nephropathy: duplex Doppler US evaluation. Radiology 1994; 192: 549–554 17. Terry JD, Rysavy JA, Frick MP. Intrarenal Doppler: characteristics of aging kidneys. J Ultrasound Med 1992; 11: 647–651 18. Jacquet F, Goldstein IB, Shapiro D. Effects of age and gender on ambulatory blood pressure and heart rate. J Hum Hypertens 1998; 12: 253–257 19. Komers R, Allen TJ, Cooper ME. Role of endothelium-derived nitric oxide in the pathogenesis of the renal hemodynamic changes of experimental diabetes. Diabetes 1994; 43: 1190–1197 20. Stoss BA, Garvin JL. Actions of nitric oxide on renal epithelial transport. Clin Exp Pharmacol Physiol 1997; 24: 591–594 21. Bank N, Aynedjian HS. Role of EDRF (nitric oxide) in diabetic renal hyperfiltration. Kidney Int 1993; 43: 1306–1312 22. Taniwaki H, Nishizawa Y, Kawagishi T et al. Decrease in glomerular filtration rate in Japanese patients with type 2 diabetes is linked to atherosclerosis. Diabetes Care 1998; 21: 1848–1855 Received for publication: 26.7.99 Accepted in revised form: 1.2.00.
(7)
Figure

Documents relatifs
The Herschel Mass-loss of Evolved StarS guaranteed time key program MESS (Ref. 14) investigates the dust and gas chemistry and the properties of CSEs for a large, representative
Figure 1 Diagnostic algorithm for asymptomatic carotid stenosis. A proposed diagnostic algorithm for the use of non- invasive imaging in evaluation of the carotid arteries
parameters (24-hour urinary albumin excretion rate, creatinine clearance, glomerular filtration rate, serum creatinine, 24-hour sodium excretion in urine); clinical
The pectin properties of apricots may play an important role in this loss of texture, even more than the initial firmness, but this is not yet well understood [1]. This
The PV-deficient mice are characterized by a decreased expression of NCC in the early DCT, leading to a discrete NaCl- losing phenotype with impaired response to diuretics, and
planners’ background, the computer-based tools they used in work, their knowledge and experience of smart cities, and their opinions on how smart cities might
For example, many recent works deal with F I -modules (functors from the category of finite sets with injec- tions to abelian groups, see [1]); finitely generated F I -modules
WHEREAS age-grouping must be adapted to the size of the populations in the administrative areas covered by the statistics, to ensure signi- ficance of the figures relating to