Publisher’s version / Version de l'éditeur:
Magnetic Resonance in Medicine, 64, 2, pp. 377-381, 2010-08-01
READ THESE TERMS AND CONDITIONS CAREFULLY BEFORE USING THIS WEBSITE. https://nrc-publications.canada.ca/eng/copyright
Vous avez des questions? Nous pouvons vous aider. Pour communiquer directement avec un auteur, consultez la
première page de la revue dans laquelle son article a été publié afin de trouver ses coordonnées. Si vous n’arrivez pas à les repérer, communiquez avec nous à PublicationsArchive-ArchivesPublications@nrc-cnrc.gc.ca.
Questions? Contact the NRC Publications Archive team at
PublicationsArchive-ArchivesPublications@nrc-cnrc.gc.ca. If you wish to email the authors directly, please see the first page of the publication for their contact information.
NRC Publications Archive
Archives des publications du CNRC
This publication could be one of several versions: author’s original, accepted manuscript or the publisher’s version. / La version de cette publication peut être l’une des suivantes : la version prépublication de l’auteur, la version acceptée du manuscrit ou la version de l’éditeur.
For the publisher’s version, please access the DOI link below./ Pour consulter la version de l’éditeur, utilisez le lien DOI ci-dessous.
https://doi.org/10.1002/mrm.22438
Access and use of this website and the material on it are subject to the Terms and Conditions set forth at
Reactions of young children to the MRI scanner environment
Malisza, Krisztina L.; Martin, Toby; Shiloff, Deborah; Yu, Dickie C. T.
https://publications-cnrc.canada.ca/fra/droits
L’accès à ce site Web et l’utilisation de son contenu sont assujettis aux conditions présentées dans le site LISEZ CES CONDITIONS ATTENTIVEMENT AVANT D’UTILISER CE SITE WEB.
NRC Publications Record / Notice d'Archives des publications de CNRC: https://nrc-publications.canada.ca/eng/view/object/?id=3c2e82da-f057-4986-9a6e-4f947f8a0f7a https://publications-cnrc.canada.ca/fra/voir/objet/?id=3c2e82da-f057-4986-9a6e-4f947f8a0f7a
Reactions of young children to the MRI scanner environment
K. L. Malisza1,2, 3, T. Martin4, D. Shiloff1, C.T. Yu3, 4
1Institute for Biodiagnostics, National Research Council of Canada, Winnipeg, Manitoba,
Canada
2Dept. of Physiology, University of Manitoba, Winnipeg, Manitoba, Canada 3Dept. of Psychology, University of Manitoba, Winnipeg, Manitoba, Canada
4St. Amant Research Centre, Winnipeg, Manitoba, Canada
Running Title: Reactions to the MRI environment in children
Word count: 3284
Correspondance:
Dr. K. L. Malisza
Institute for Biodiagnostics
National Research Council of Canada 435 Ellice Avenue Winnipeg, Manitoba Canada, R3B 1Y6 Tel: 204-984-6616 Fax: 204-984-7036 e-mail: Kris.malisza@nrc-cnrc.gc.ca
ABSTRACT
Seventy children aged 2 to 7 years were exposed to the MR imaging environment through a series of steps typical of a research study. Their willingness to proceed through the process was used to estimate the prevalence of fear. Thirty-seven children (53%, 95% CI [41%, 65%]) completed the approach sequence. Although the correlation of child age in months (M = 60.1, SD = 16.5, N = 70) and highest successful step (M = 5.8, SD = 2.6, 95% CI [5.2, 6.4]) completed was not statistically significant at the 0.05 level, r(68) = 0.21, p = 0.08, 95% CI [-0.03, 0.42], the proportion of children aged 6-7 yrs who successfully completed all steps (14 of 21, 67%, 95% CI [50%, 84%]) was significantly different from the proportion of children aged 2-3 yrs who completed all steps (6 of 23, 26%, 95% CI [11%, 41%]), (Fisher's Exact Test, two-tailed P = 0.0148). A failure rate of at least 50% should be included into group size calculations when performing studies with young children (2-7 years), in addition to motion and other experimental factors.
KEY WORDS:
INTRODUCTION
Magnetic Resonance Imaging (MRI) environments present psychological risks to those being imaged (1). Risks include transitory fear and panic (2) that sometimes result in prematurely-terminated scans (3). Long-term effects have also been reported, including both increases and decreases in claustrophobic feelings in MRI settings (4) and in other enclosed spaces (5). A number of studies have reported proportions of people who show strong fear and refuse to receive an MRI scan unless sedated (1). These data are
inadequate for estimating the prevalence of fear in children or their willingness to participate in MRI research studies.
The available data on psychological risks of MRI come mainly from adult patients in clinical settings, where the MRI is often being used to diagnose a potentially serious medical condition. These situations present additional stresses to patients and may exacerbate fearful reactions to the MRI environment. The difference, if any, between fear prevalence under these conditions versus prevalence in MRI research contexts is
unknown. Furthermore, the risks for children are less well-studied (with the exception of Dewey et al.) (6), but may differ from those for adults due to limited understanding of the environment, and reduced ability to communicate with those administering the scan.
Researchers and ethics boards require data regarding the probability and severity of all of these effects in order to make accurate judgments of the risk/benefit ratio for prospective participants, and to help estimate the numbers of participants who must be recruited in order to have a final sample of desired size. The lack of data on the reactions of children to MRI in research settings increases the likelihood that children will be excluded from research and the benefits it may provide. The present study addressed this
need. We estimated the population proportion of children aged 2 through 7 (n = 70) who demonstrated willingness to enter an MRI scanner in a non-clinical research situation.
METHOD
Participants
Seventy children (41 male, 29 female) between the ages of 2 and 7 participated. Parents were recruited through advertisements in the local papers and information sheets and posters. Standard MRI exclusion criteria were in place; children were excluded if parents indicated that the child may have any metal in the body (with the exception of amalgam fillings; however, none of the children had these fillings) and diagnosis of claustrophobia or fear of tight or enclosed spaces. A parent provided informed consent and was present with the child throughout the procedure. Assent of the children who participate in the study was also obtained. A Siemens 3.0 T Tim Trio clinical MRI scanner with 60 cm bore size, was used to gauge the reactions of the children to the MRI environment. The informed consent procedure and Visual Analogue Scale (VAS; see Measures, below) competency assessment took place in a reception room near the scanning room. The protocol was reviewed and approved by the local Research Ethics Boards at each affiliated institution.
Measures
Willingness and comfort level were the dependent variables. Willingness was measured in terms of progress through an 8-step series of approximations (see Procedure, below) to normal patient behaviour during MRI scans. Comfort level was measured on a
5-point self-report scale, where 1 meant no fear/anxiety at all, 3 meant "this is ok, neither good nor bad" and 5 meant something disliked or frightening that the child preferred to avoid. Ratings were collected using a VAS on a printed card (see Figure 1). The
participant was asked to point to the face that indicated how he or she was feeling at each step.
We contacted each child's parent prior to their visit and asked the parent to identify five items that the child liked and five items that the child disliked or feared. We retrieved pictures (if possible, photographs) of these items from the internet and printed them in colour on 8.5" by 11" sheets of paper. Before the child encountered the scanner we showed him or her a printed VAS card (Figure 1) and stated the meaning of each face. We then showed the child each of the 10 pictures in random order and asked, "Do you like this?" and then, "Show me how much." Following the second question the child was prompted to point to one of the five faces on the VAS scale. If the child's first rating disagreed with his or her response to the "Do you like this?" question, the experimenter prompted a second response (e.g., "That face means that you don't like it. You said that you do like it; which face means that you do like it and how much, a lot or only a little?"). The child was not prompted further following this second prompted rating if it continued to disagree with his or her initial statement of like/dislike.
Initial VAS ratings from children agreed with their assessments of like/dislike for 91.3% (639/700) of items. Final VAS ratings agreed with like/dislike assessments for 93.0% (651/700) of items. Six children gave final VAS ratings that agreed with their like/dislike assessments on 7 or fewer items (i.e., agreement was 70% or less).
Procedure
The following steps were followed for the MRI scanner encounter; each child was asked to:
1. stand outside the scanner room,
2. enter the room and look at the scanner,
3. put in ear plugs and listen to the scanner noises (generated using a standard fast spin echo sequence),
4. stand beside the scanning bed while the noises continued, The scanner noise was then stopped.
5. lie on the scanning bed, outside the main bore,
6. lie on the bed while the head coil and mirror (through which the child could see his or her parent standing at the foot of the bed) were put in place,
7. lie still while the bed was moved slightly into the bore to position the subject using laser light positioning alignment, as is performed in routine MRI to ensure the region to be imaged (i.e., the brain) will be centred in the magnet for imaging. The child was asked to close his/her eyes while the laser was activated.
Following step 7, the child was asked if he or she was willing to enter into bore. If the child responded affirmatively, then he or she was asked to:
8. lie on the bed while it moved into the scanner bore.
After each completed step the experimenter asked, "how are you doing here?" and showed the child the VAS card to prompt a comfort rating. Therefore, no imaging was conducted with the child in the magnet bore and those children who completed all step
spent approximately 30 seconds in the bore while their comfort level was assessed. The six children with 70% or less agreement between final VAS ratings and like/dislike assessments during the VAS competency assessment were instead asked, "Are you feeling okay here?" and their yes/no response was recorded. A VAS rating was requested immediately following the yes/no response, but a "no" response terminated participation regardless of the VAS rating. Participation concluded when the child indicated an unwillingness to proceed, rated the current step as a 4 or 5 on the VAS, indicated feeling not okay at the current step, or completed all of the approach steps.
Inter-observer Agreement
Samples of child responses during the like/dislike assessments, VAS familiarization ratings, and VAS ratings during approach to the MRI scanner were recorded by a second observer in order to enhance believability of the primary observations. Of 678 like/dislike responses made, 447 (65.9%) were recorded by the second observer. The experimenter and second observer agreed about the response made in 399 of 447 cases (89.3% agreement). Of 689 VAS familiarization ratings, 462 (67.1%) were recorded by the second observer, who agreed with the experimenter about the response made in 423 of 462 cases (91.6% agreement). Of 431 MRI scanner approach VAS ratings, 302 (70.1%) were recorded by the second observer, who agreed with the experimenter about the response made in 281 of 302 cases (93.0% agreement). The observer and experimenter agreed when to terminate the study, based on the criteria outlined above, for all children (100%). The second observer recorded data during less than 100% of sessions because of the costs of secondary observation, and because the
agreement scores obtained were high.
Follow-up
Parents of all subjects who did not complete all of the steps involved in the study were contacted one week following the study date and asked follow-up questions
regarding their child to determine if there were any behavioural changes noticed following the visit.
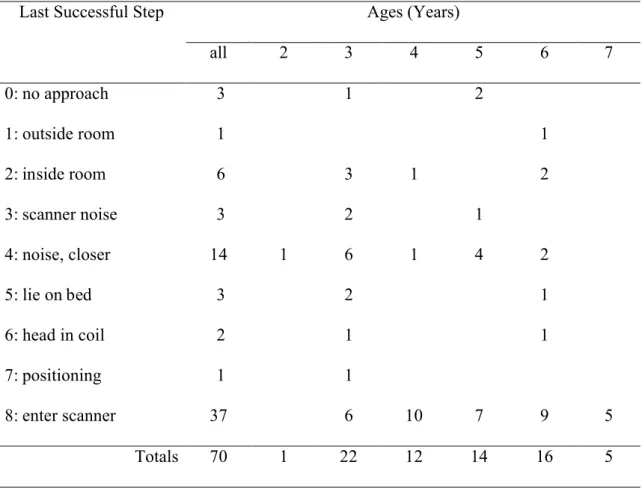
RESULTS
Table 1 presents counts of participants, by age, who ended participation at each of nine possible highest successful steps (approach sequence steps 1 through 8, or 0 if step 1 was unsuccessful). Thirty-seven children (53%, 95% CI [41%, 65%]) completed the approach sequence and entered the bore of the MRI scanner. Of 41 male subjects, 20 (49%, 95% CI [33%, 64%) completed the full approach sequence successfully. Of 29 female subjects, 17 (59%, 95% CI [41%, 77%]) completed the sequence successfully. The mean highest successful step reached was 5.8 for males (SD = 2.5, 95% CI [5.1, 6.6]) and 5.9 (SD = 2.8, 95% CI [4.8, 6.9]) for females.
The correlation of child age in months (M = 60.1, SD = 16.5, N = 70) and highest successful step (M = 5.8, SD = 2.6, 95% CI [5.2, 6.4]) completed was not statistically significant at the 0.05 level, r(68) = 0.21, p = 0.08, 95% CI [-0.03, 0.42]. However, the proportion of children aged 6-7 yrs who successfully completed all steps (14 of 21, 67%, 95% CI [50%, 84%]) was significantly different from the proportion of children aged 2-3 yrs who completed all steps (6 of 23, 26%, 95% CI [11%, 41%]) (Fisher's Exact Test,
two-tailed P = 0.0148). The breakdown of children who successfully completed all steps (steps 1 through 8) as a factor of age were as follows: 0% (0 of 1) of children at age 2, 27% (6 of 22, 95% CI [9%, 46%]) at age 3, 83% (10 of 12, 95% CI [62%, 100%]) at age 4, 50% (7 of 14, 95% CI [24%, 76%]) at age 5, 53% (9 of 16, 95% CI [32%, 81%]) at age 6, and 100% (5 of 5) of children at age 7.
The greatest stumbling block for cooperation was the step involved in lying down on the patient table (step 5). Of the 33 children who did not complete the protocol, this position of vulnerability was the stopping point for 14 (42%, 95% CI [26%, 59%]; see Table 1). The second most significant factor contributing to not completing the approach was the introduction of the scanner noise (step 3). Of the 33 children who terminated prematurely, 6 (18%, 95% CI [5%, 31%]) stopped prior to this point (successfully completing only steps 1 and 2) with an additional 3 subjects completing step 3 but not wanting to continue hearing the scanner noises (n=9, 27%, 95% CI [12%, 42%]).
Among the 33 children who did not complete all steps, 17 (52%, 95% CI [34%, 69%]) ended their participation by stating an unwillingness to continue, rather than by rating a performed step at 4 or 5 on the VAS. The remaining 16 children (48%, 95% CI [31%, 66%]) terminated participation by rating a performed step at 4 or 5 on the VAS. The experimenter therefore immediately ended the session and removed the child from the scanning environment. Several of the children whose participation ended this way indicated a desire to continue, but the experimenter refused and reiterated for the child that a rating of 4 or 5 meant that the session must end.
No adverse events occurred in any of the 70 sessions. No child at any time cried, panicked, bolted, or indicated fear in any manner other than stating an unwillingness to
continue, or providing a 4 or 5 rating on the anxiety scale. No parent requested to terminate participation. No parent stated concern about his or her child's well-being.
Follow-up telephone interviews were conducted with the parents of children who did not complete all approach steps (n = 33). We were able to contact all parents of the 33 children, none of whom indicated that their child showed any long-lasting effects of participation. Families with children who did not complete all of the steps in the protocol were asked if they were interested in participating in a separate, but related, follow-up study in a mock scanner environment. All parents but one indicated they were willing to return for the follow-up study. Data collection is currently ongoing for this study. The sole parent unwilling to return stated that they were simply too busy to participate.
DISCUSSION
The results suggest that approximately 53% of children between the ages of 2 and 7 years would be willing to enter a MRI scanner as part of participating in an imaging study. Neither age nor sex strongly predicted a child's willingness to receive the scan, however, it must be noted that certain age groups contained few subjects. We do not anticipate that the overall results would vary much from those presented given a more even distribution of child ages, however, we are limited in the conclusions we can draw given the disparity in child numbers within the age groups.
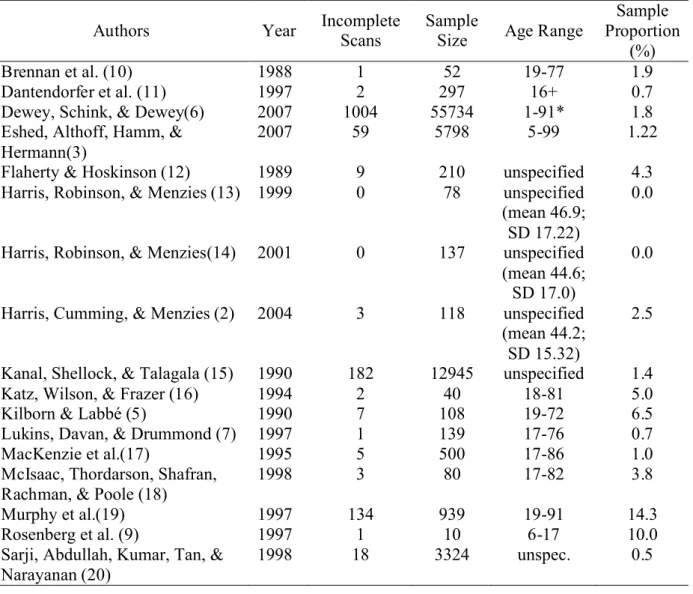
The observed proportion of premature termination (47%) is the highest among proportions we found in the literature (see Table 2; articles were identified by searching the PubMed and Google Scholar database services for terms including MRI, imaging, fear, anxiety, claustrophobia, premature termination, and children, and by scanning the
reference sections of the articles that described premature termination). We suggest that several factors may be responsible for this discrepancy. First, our participants were younger than those from previous studies. Second, we did not pressure or even encourage the child to continue if he or she indicated unwillingness to perform a particular step. We also requested that parents not coax the children to continue, as they might for a clinical scan, and we received full compliance from parents in this regard. In several cases children expected and wanted the protocol to continue even after providing a VAS rating greater than three. Ethically, this is an interesting dilemma, as frequently in research studies we wish to obtain assent from the child to participate in a study as well as informed consent by the parent or legal guardian. We wish to ensure that children are willingly participating in the research and at any point if they would like to stop
participation, their desires would be respected. More frequently than not, some attempt is made to request the child to “at least try it”, with respect to some aspect of the study, for example, lie down on the bed. Perhaps this additional request is not undue pressure for the child, but clearly there is a line at which the researcher and parent should no longer push the child to participate if he or she does not want to or feels uncomfortable. The point at which this line should be drawn would be an interesting debate for future ethical studies.
We distinguished willingness to complete the scan from comfort level, and measured both. The VAS proved to be useful, allowing us to repeatedly measure comfort level in situ. In previous studies, State-Trait Anxiety Inventory questionnaire items were presented post-scan, and were reworded to require retrospective evaluation of anxiety experienced during the scans (2, 7). A secondary purpose of the VAS was to identify
elevating discomfort levels before adverse events occurred. This too appears to have been successful, in that 16 children ended their participation by providing a rating higher than 3 despite being willing to complete the step, and no adverse events of any kind were observed.
The study was limited by the fact that we did not scan children who willingly entered the bore. The proportion of these children who may have prematurely terminated over the course of a 30 to 40-min scan is unknown. Of the 37 children who completed the approach, only five (14%, 95% CI [3%, 25%]) showed any increase in VAS ratings while moving from step 7 to 8 and one child indicated a decreased VAS rating.
The response of a patient during an MRI scan may affect his or her future responses to the same or similar situations. It would therefore have been useful to learn how the children would have reacted had we brought them back for a second exposure. Some evidence that patients habituate to the MRI experience, even if initially stressful, comes from the success of exposure-based treatments for MRI scan anxiety (8, 9). These procedures involve repeatedly presenting the fear-eliciting stimuli and situations under controlled conditions with the result (in both studies cited) that the situations come to elicit little or no fear. This demonstrates the importance of familiarizing the children with the scanning environment. Slow introduction did not lead to any lasting negative effects in the current study, since the child was immediately removed from the situation prior to it becoming a problem. The follow-up telephone interviews we conducted with the parents of children who did not complete all approach steps clearly showed that the situation to which the children were exposed did not cause any significant discomfort or long-lasting negative effects. This fact was supported by the comments of several parents
that their children had asked them when they could return to the scanner again.
In our experience, children are often excluded from MRI research and its potential benefits because of concerns about physical or psychological risks. In this study we gathered data that may help to prevent exclusion or inclusion based on inaccurate estimates of the risk of fear reactions to the MRI environment. Therefore, researchers who work with children should factor into their calculations for correct group size a failure rate of approximately 50% for children entering the imaging environment between the ages of 2 and 5 years and 35% for children aged 6 to 7 years, not including experimental failure due to motion and other factors. These numbers can likely be improved if researchers commit the extra time, care and effort required to acclimatize the children to the MR environment by successive approximations to the requirements for the actual imaging study.
ACKNOWLEDGMENT
We would like to thank the parents and children who participated in this research, and Dr. P. Gervais and Ms Q. Senkow for technical assistance. This work was supported by a New Emerging Team grant in Neuroethics from the Canadian Institutes of Health Research (NNF 69458, awarded to J. Downie; www.neuroethics.ca).
REFERENCES
1. Marshall J, Martin T, Downie J, Malisza K. A comprehensive analysis of MRI research risks: in support of full disclosure. Can J Neurol Sci 2007;34(1):11-17. 2. Harris LM, Cumming SR, Menzies RG. Predicting anxiety in magnetic resonance
3. Eshed I, Althoff CE, Hamm B, Hermann KG. Claustrophobia and premature termination of magnetic resonance imaging examinations. J Magn Reson Imaging 2007;26(2):401-404.
4. Wood BS, McGlynn FD. Research on posttreatment return of claustrophobic fear, arousal, and avoidance using mock diagnostic imaging. Behav Modif
2000;24(3):379-394.
5. Kilborn LC, Labbe EE. Magnetic resonance imaging scanning procedures:
development of phobic response during scan and at one-month follow-up. J Behav Med 1990;13(4):391-401.
6. Dewey M, Schink T, Dewey CF. Claustrophobia during magnetic resonance imaging: cohort study in over 55,000 patients. J Magn Reson Imaging 2007;26(5):1322-1327.
7. Lukins R, Davan IG, Drummond PD. A cognitive behavioural approach to preventing anxiety during magnetic resonance imaging. J Behav Ther Exp Psychiatry 1997;28(2):97-104.
8. Klonoff EA, Janata JW, Kaufman B. The use of systematic desensitization to overcome resistance to magnetic resonance imaging (MRI) scanning. J Behav Ther Exp Psychiatry 1986;17(3):189-192.
9. Rosenberg DR, Sweeney JA, Gillen JS, Kim J, Varanelli MJ, O'Hearn KM, Erb PA, Davis D, Thulborn KR. Magnetic resonance imaging of children without sedation: preparation with simulation. J Am Acad Child Adolesc Psychiatry 1997;36(6):853-859.
10. Brennan SC, Redd WH, Jacobsen PB, Schorr O, Heelan RT, Sze GK, Krol G, Peters BE, Morrissey JK. Anxiety and panic during magnetic resonance scans. Lancet 1988;2(8609):512.
11. Dantendorfer K, Amering M, Bankier A, Helbich T, Prayer D, Youssefzadeh S, Alexandrowicz R, Imhof H, Katschnig H. A study of the effects of patient anxiety, perceptions and equipment on motion artifacts in magnetic resonance imaging. Magn Reson Imaging 1997;15(3):301-306.
12. Flaherty JA, Hoskinson K. Emotional distress during magnetic resonance imaging. N Engl J Med 1989;320(7):467-468.
13. Harris LM, Robinson J, Menzies RG. Evidence for fear of restriction and fear of suffocation as components of claustrophobia. Behav Res Ther 1999;37(2):155-159. 14. Harris LM, Robinson J, Menzies RG. Predictors of Panic Symptoms During
Magnetic Resonance Imaging Scans. International Journal of Behavioral Medicine 2001;8(1):80-87.
15. Kanal E, Shellock FG, Talagala L. Safety considerations in MR imaging. Radiology 1990;176(3):593-606.
16. Katz RC, Wilson L, Frazer N. Anxiety and its determinants in patients undergoing magnetic resonance imaging. J Behav Ther Exp Psychiatry 1994;25(2):131-134. 17. Mackenzie R, Sims C, Owens RG, Dixon AK. Patients' perceptions of magnetic
resonance imaging. Clin Radiol 1995;50(3):137-143.
18. McIsaac HK, Thordarson DS, Shafran R, Rachman S, Poole G. Claustrophobia and the magnetic resonance imaging procedure. J Behav Med 1998;21(3):255-268. 19. Murphy KJ, Brunberg JA. Adult claustrophobia, anxiety and sedation in MRI.
Magn Reson Imaging 1997;15(1):51-54.
20. Sarji SA, Abdullah BJ, Kumar G, Tan AH, Narayanan P. Failed magnetic resonance imaging examinations due to claustrophobia. Australas Radiol 1998;42(4):293-295.
Table 1. Number of children in each age group and the last step which they successfully completed.
Last Successful Step Ages (Years)
all 2 3 4 5 6 7 0: no approach 3 1 2 1: outside room 1 1 2: inside room 6 3 1 2 3: scanner noise 3 2 1 4: noise, closer 14 1 6 1 4 2 5: lie on bed 3 2 1 6: head in coil 2 1 1 7: positioning 1 1 8: enter scanner 37 6 10 7 9 5 Totals 70 1 22 12 14 16 5
Table 2: Proportions of Patients Unable to Complete MRI Scans
Authors Year IncompleteScans Sample Size Age Range
Sample Proportion
(%) Brennan et al. (10) 1988 1 52 19-77 1.9 Dantendorfer et al. (11) 1997 2 297 16+ 0.7 Dewey, Schink, & Dewey(6) 2007 1004 55734 1-91* 1.8 Eshed, Althoff, Hamm, &
Hermann(3)
2007 59 5798 5-99 1.22 Flaherty & Hoskinson (12) 1989 9 210 unspecified 4.3 Harris, Robinson, & Menzies (13) 1999 0 78 unspecified
(mean 46.9; SD 17.22)
0.0 Harris, Robinson, & Menzies(14) 2001 0 137 unspecified
(mean 44.6; SD 17.0)
0.0 Harris, Cumming, & Menzies (2) 2004 3 118 unspecified
(mean 44.2; SD 15.32)
2.5 Kanal, Shellock, & Talagala (15) 1990 182 12945 unspecified 1.4 Katz, Wilson, & Frazer (16) 1994 2 40 18-81 5.0 Kilborn & Labbé (5) 1990 7 108 19-72 6.5 Lukins, Davan, & Drummond (7) 1997 1 139 17-76 0.7 MacKenzie et al.(17) 1995 5 500 17-86 1.0 McIsaac, Thordarson, Shafran,
Rachman, & Poole (18)
1998 3 80 17-82 3.8
Murphy et al.(19) 1997 134 939 19-91 14.3 Rosenberg et al. (9) 1997 1 10 6-17 10.0 Sarji, Abdullah, Kumar, Tan, &
Narayanan (20)
1998 18 3324 unspec. 0.5 * Not given, but can be inferred from figure in article.
FIGURE CAPTIONS
Figure 1. Visual Analogue Scale (VAS) used during the current study to determine likes, dislikes and comfort level of the children.