Urol Res (1997) 25 [Suppl 1]: S 3-S 6 © Springer-Verlag 1997
P. J i c h l i n s k i • G. W a g n i b r e s • M . F o r r e r • J. M i z e r e t L. G u i l l o u • M . O s w a l d . F. S c h m i d l i n • P. G r a b e r H . V a n d e n B e r g h • H . - J . L e i s i n g e r
Clinical assessment of fluorescence cystoscopy during
transurethral bladder resection in superficial bladder cancer
A b s t r a c t The prognosis of superficial bladder cancer in terms of recurrence and disease progression is related to bladder tumor multiplicity and the presence of concomi- tant "plane" tumors such as high-grade dysplasia and car- cinoma in situ. This study in 33 patients aimed to demon- strate the role of fluorescence cystoscopy in transurethral resection of superficial bladder cancer. The method is based on the detection of protoporphyrin-IX-induced flu- orescence in urothelial cancer cells by topical administra- tion of 5-aminolevulinic acid. The sensitivity and the spec- ificity of this procedure on apparently normal mucosa in superficial bladder cancer are estimated to be 82.9% and 81.3%, respectively. Thus, fluorescence cytoscopy is a simple and reliable method for mapping the bladder mucosa, especially in the case of multifocal bladder dis- ease, and it facilitates the screening of occult dysplasia. K e y w o r d s C a r c i n o m a • Transitional cell - C y s t o s c o p y Fluorescence - 5-Aminolevulinic acid • Protoporphyrin IX
Introduction
In superficial bladder transitional cell carcinoma, tumor multiplicity and concomitant urothelial atypia are indica- tors of a poor disease prognosis [1, 2]. High-grade dyspla-
R Jichlinski (~) - M. Oswald • H.-J. Leisinger Department of Urology, University Hospital, CHUV, CH-1011 Lausanne, Switzerland
G. Wagni~res • M. Forrer • J. Mizeret • H. Van den Bergh Laboratory of Environmental Engineering,
Swiss Federal Institute of Technology (EPFL), CH-1015 Lausanne, Switzerland
L. Guillou
Institute of Pathology, University Hospital, CHUV, CH-1011 Lausanne, Switzerland F. Schmidlin • R Graber
Department of Urology, University Hospital, HCUG, CH-1205 Geneva, Switzerland
sia or carcinoma in situ point to a higher risk of recurrence or progression [I, 3]. Occasionally, reddish and mossy spots of the bladder mucosa allow the localization by biopsy of these foci of dysplasia, but mostly no specific changes of the bladder wall can be recognized by white light cystoscopy [4].
Although its accuracy is highly variable, urinary blad- der cytology as a routine test in the early detection of blad- der cancer and in the patient monitoring after treatment is well established, but does not enable concomitant urothe- lial atypia at the time of the first bladder tumor resection to be discovered. Moreover, the usefulness of random biopsies from normal-looking mucosa has recently been seriously questioned [5]. Therefore, as for epithelial can- cers of other organs such as the oesophagus or the uterine cervix, there is a need to localize urothelial atypia during the endoscopic exploration.
Simple methods such as mucosal staining with methyl- ene blue have failed due to lack of sensitivity and speci- ficity [6]. Fluorescence studies correlated with histology on cystectomy specimens after intravenous injection o f h e - matoporphyrin derivatives have demonstrated the possible role of a photodynamic method for detecting and localiz- ing dysplasia and carcinoma in situ in bladder cancer [7]. However, the sophisticated equipment needed to obtain good images, the lack of selectivity of the photosensitizer and the risk of skin photosensitization have limited its ap- plication for clinical routine practice in urology. Recently, the high fluorescence contrast and intensity observed when treating cutaneous in situ tumors by photodynamic therapy using the endogenous photosensitizer protoporphyrin IX (PpIX), induced by the topical application of 5-amino- levulinic acid (ALA), has suggested the same approach to be suitable for detection and treatment of epithelial tu- mors of other organs, such as the oesophagus and the bladder [8]. The first clinical reports on the photodetection of early transitional cell carcinoma by light-induced fluo- rescence of PpIX following topical administration of ALA [9, 11] stimulated interest in this new method of mapping the bladder mucosa in search of dysplasia or carcinoma in situ.
$ 4
By c o m p a r i s o n to the first s y s t e m o f b l a d d e r w a l l i l l u m i n a t i o n w i t h a k r y p t o n ion laser, the n e w l i g h t source, a x e n o n arc l a m p , c o n s i d e r a b l y s i m p l i f i e s the p r o c e d u r e b y e n a b l i n g the i n v e s t i g a t o r to e x a m i n e the b l a d d e r w a l l in r e a l t i m e w i t h o u t the n e c e s s i t y for an aux- i l i a r y d e v i c e . This study p r e s e n t s our e x p e r i e n c e with this new s y s t e m and a t t e m p t s to assess the a c c u r a c y o f the m e t h o d in the d e t e c t i o n o f h i g h - g r a d e d y s p l a s i a a n d c a r c i - n o m a in situ.
Material and method
Fifty milliliters of a 3% solution of ALA, buffered with 5 ml phos- phate-buffered saline (PBS) and adjusted to a pH of 5.3 with 7 ml sodium hydroxide (1 N), were instilled into the bladder through a 16-French Foley catheter about 6 h before photodetection. Patients were asked to keep the catheter closed for 4 h to optimize the exposure of the bladder wall to the photosensitizing solution. The light source was a filtered xenon arc lamp which produced either white light for conventional cystoscopy or blue light with a wavelength range of 380-450 nm to excite the sensitized bladder mu- cosa. A foot pedal was used to switch from white to blue light and vice versa when necessary. The power of the fluorescence exci- tation light at the end of the cystoscope ranged between 150 and 480 mW, giving under normal conditions of use a power density of
2
65 mW/cm . The white light, the blue excitation light and the result- ing tissue fluorescence were transmitted through the optical fiber bundle of a Storz cystoscope or resectoscope. Two optics of 0 ° and of 30 °, suitable for either a cystoscope or resectoscope sheath, were specially configured to optimize the light transmission. As the PpIX emission peak was 635 nm, a long-pass filter (X>490 nm) was adapted to the ocular piece of the cystoscope to transmit the red and cut out most of the blue-reflected excitation light. Thus, the flu- orescent spots appeared red, whereas the non-fluorescent mucosa stayed green. The somewhat darker bladder wall vessels facilitated the positioning of the cytoscope during the operation.
Starting in January t995, 33 bladder examinations were per- formed in 31 patients, 23 male patients and 8 female patients (two patients had two successive operations). Mean age was 66.1, rang- ing from 44 to 84 years. Eleven patients were operated on for the first time, 6 for the second time and 16 for the third time or more. Topical chemotherapy or immunotherapy with bacille Cal- mette-Gu6rin (BCG) was added to the previous surgical treatment in 19 patients. Bladder urinary cytological examination was regularly performed when the catheter was introduced for the ALA instilla- tion.
The operation always started with a careful bladder inspection under white light in order to note the presence, number and location of all the visible tumors and suspicions areas. To evaluate the sensitivity and the specificity of the method in patients with bladder tumors, a four-quadrant random biopsy of the normal bladder mucosa was performed for each patient as follows: the randomly des- ignated spot of normal mucosa under white light was excited under blue light to determine the fluorescence response and then immedi- ately sampled by forceps for biopsy. A total of 132 random biopsies were obtained in this way, 51 in fluorescent areas and 81 in non- fluorescent areas. All other fluorescent areas on an apparently nor- mal or slightly irregular mucosa under white light were also biop- sled and sent for analysis. The transurethral resection of significant tumors was generally performed under fluorescence, except in the case of major bleeding. Papillary and nonpapillary urothelial carci- nomas were graded and staged according to the WHO 1973 classi- fied [12] and the IUCC/AJC-1992 system [13], respectively. Flat intraepithelial neoplastic lesions were graded according to the crite- ria of Nagy et al. [14], and classified as grade 1 (mild dysplasia), grade 2 (moderate dysplasia), grade 3 (marked dysplasia) and in si- tu carcinoma.
Results
N o s y s t e m i c or l o c a l side effects f o l l o w i n g A L A b l a d d e r i n s t i l l a t i o n e i t h e r b e f o r e or after the p h o t o d e t e c t i o n p r o c e - d u r e w e r e noted. E x c e p t for one pTaG1 tumor, all p a p i l - lary t u m o r s v i s i b l e on w h i t e light c y s t o s c o p y w e r e fluo- rescent. T h e c o r r e l a t i o n s b e t w e e n the f l u o r e s c e n c e find- ings and the p r e s e n c e or a b s e n c e o f c a n c e r cells for the 132 r a n d o m b i o p s i e s on a p p a r e n t l y n o r m a l m u c o s a are s h o w n in Table 1. T h e p r e d i c t i v e v a l u e o f a p o s i t i v e fluo- r e s c e n c e c o r r e s p o n d i n g to a t u m o r is e s t i m a t e d at 66.6% (34/51), and the p r e d i c t i v e v a l u e o f a n e g a t i v e f l u o r e s c e n c e c o r r e s p o n d i n g to b e n i g n t i s s u e at 91.3 % (74/81). T h e sen- sitivity o f this p h o t o d e t e c t i o n m e t h o d in s u p e r f i c i a l b l a d - der c a n c e r can b e e s t i m a t e d at 82.9% (34/41) and the s p e c - ificity at 81.3% (74/91).
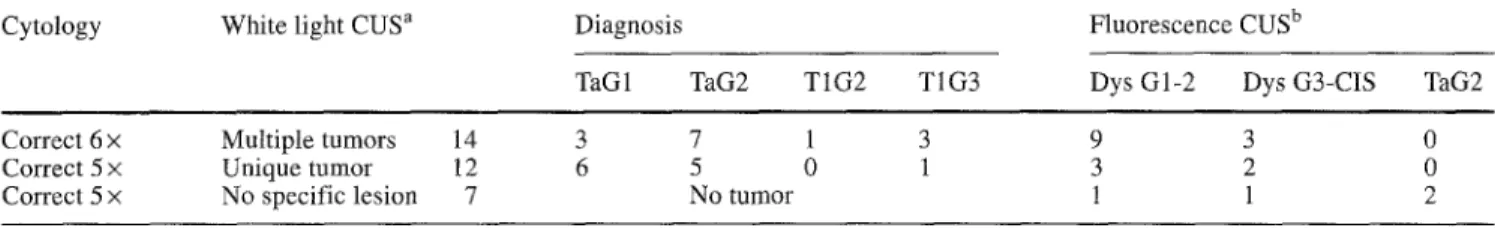
In 22/33 p a t i e n t s , 66.6% o f our c o l l e c t i v e , 47 t u m o r s w e r e d e t e c t e d b y the f l u o r e s c e n c e (Table 2). S e v e n o f these 22 patients (31.8%) h a d g r a d e 3 d y s p l a s i a or c a r c i n o m a in situ (CIS). Table 3 s h o w s the c o r r e l a t i o n s b e t w e e n c y t o l - ogy, w h i t e light c y s t o s c o p y and f l u o r e s c e n c e f i n d i n g s for e a c h patient. T h e f l u o r e s c e n c e m e t h o d d e t e c t e d a d d i - t i o n a l u r o t h e l i a l atypia, i n v i s i b l e u n d e r w h i t e light, in 12/14 p a t i e n t s (85%) w i t h m u l t i p l e t u m o r s and in 5/12 p a - tients (41%) w i t h a single tumor. In c o n t r a s t to the f l u o r e s c e n c e c y t o s c o p y , u r i n a r y c y t o l o g y was not r e a l l y h e l p f u l in p a t i e n t s w i t h m a c r o s c o p i c tumors. F o r patients p r e v i o u s l y o p e r a t e d on for a s u p e r f i c i a l b l a d d e r cancer, who p r e s e n t e d no s p e c i f i c l e s i o n on w h i t e light c y s t o s c o p y , f l u o r e s c e n c e c y s t o s c o p y c o n f i r m e d the a b s e n c e o f n e o - p l a s t i c l e s i o n s in three and d e t e c t e d u r o t h e l i a l a t y p i a or e v e n a s m a l l t u m o r in f o u r o f them. I n t h e s e cases, u r i n a r y c y t o l o g y c o u l d o n l y g i v e an i n d i c a t i o n o f the p r e s e n c e or a b s e n c e o f c a n c e r o u s cells, w h e r e a s f l u o r e s c e n c e c y t o s - c o p y p r e c i s e l y d e l i n e a t e d the n u m b e r o f c a r c i n o m a t o u s spots.
Table 1 Correlation between fluorescence findings and histopath- ological diagnosis for the 132 random biopsies on apparently nor- mal mucosa in superficial bladder cancer
Positive Negative Total histology histology
Positive fluorescence 34 17 51 Negative fluorescence 7 74 81
41 91 132
Table 2 Diagnosis distribution of the 47 tumors invisible by white light cystoscopy and detected by fluorescence in 22/33 patients
"Flat" intraepithelial tumors 41 Papillary tumors 6 Grade 1 dysplasia 12 pTaG1 2 Grade 2 dysplasia 15 pTaG2 3 Grade 3 dysplasia 3 pT1G3 1 Carcinoma in situ 11
Table 3 Correlation between cytology, white light cystoscopy
(CUS)
and fluorescence findings$5
Cytology White light CUS a Diagnosis
TaG1 TaG2 T1G2 T1G3
Fluorescence CUS b
Dys G1-2 Dys G3-CIS TaG2 Correct 6 x Multiple tumors 14 3 7 1 3
Correct 5 x Unique tumor 12 6 5 0 1 Correct 5 x No specific lesion 7 No tumor
9 3 0
3 2 0
1 1 2
a Except one pTaGl tumor, all papillary tumors, visible by white light cystoscopy, were fluorescent b Additional tumors invisible under white light and detected by fluorescence
Discussion
In the C a n t o n o f Vaud in Switzerland, the incidence of superficial bladder cancer is around 18.6/100 000 per year in male patients and 4 . 2 / 1 0 0 0 0 0 per year in female pa- tients, which represents a ratio o f 4:1 [15]. The individual risk o f cancer progression, reflecting the natural history o f the disease, varies f r o m 4 to 45% [16]. Moreover, in the year f o l l o w i n g the first treatment, superficial bladder can- cer tends to recur in a proportion up to 70%; and 1 0 - 2 0 % of recurrences on the site o f the initial t u m o r g r o w f r o m c a r c i n o m a t o u s foci left during the first operation [17]. I f the characterization o f dysplastic changes in the urothe- lium is important in the evaluation o f the disease p r o g n o - sis and the risk o f recurrence, the surgical treatment o f all e x o p h y t i c and "flat" tumors during the first operation is mandatory.
So far no reliable m e t h o d has been available to deter- mine the cancer cells in delineating the tumor basis and screening urothelial atypia. P p I X - i n d u c e d fluorescence de- tection o f urothelial cancer cells by topical administration o f A L A is a simple and harmless m e t h o d for this. No lo- cal or systemic reaction was noted after A L A bladder in- stillation or illumination with the x e n o n blue light. The cor- relation between the fluorescence tissue response and the histopathological diagnosis on normal m u c o s a in superfi- cial bladder cancer establishes that a fluorescent spot cor- responds to a c a r c i n o m a in about two out of three cases and above all that a nonfluorescent spot corresponds to be- nign tissue in nine out o f ten cases. Undoubtedly, fluores- cence c y s t o s c o p y aids in the biopsy o f the urothelium at the right place in bladder cancer. The electrocoagulation of false-positive fluorescent areas, due to i n f l a m m a t o r y or hyperplastic cells, does not harm the bladder with normal compliance.
The sensitivity and the specificity o f the procedure on apparently normal m u c o s a in patients with superficial bladder cancer is estimated at 82.9% and 81.3%, respec- tively. Calculated on a per patient basis it has been esti- mated at 94.2% b y the M u n i c h group [10]. F o l l o w i n g the same approach in our collective, bladder biopsies revealed dyspastic urothelial changes or CIS in 23 patients, a m o n g w h o m 22 had a positive fluorescence. Thus, our per pa- tient estimated sensitivity is near 95.6%, an equivalent value to the previous estimation.
Fluorescence c y s t o s c o p y constitutes a previous aid to white light cystoscopy. It is a simple and a reliable m e t h o d in m a p p i n g the m u c o s a in bladder cancer. It facilitates the delineation o f tumors and the screening o f occult dysplas- tic changes, especially in multiple papillary bladder dis- ease. In addition, it appears very useful in monitoring the patients after treatment.
Subsequent studies will be needed to assess whether the optimal transurethal bladder resection obtained with fluo- rescence c y t o s c o p y contributes to a reduction o f the risk o f recurrence in superficial bladder cancer.
Acknowledgement This study has been supported by the Vaud-Ge- neva Foundation.
References
1. Olsen PR, Wolf H, Schroeder T, Fischer A, Hojgaard K (1988) Urothelial atypia and survival rate of 500 unselected patients with primary transitional-cell tumour of the urinary bladder. Scand J Urol Nephrol 22:257
2. Witjes JA, Kiemeney LALM, Oosterhof GON, Debruyne FMJ (1992) Prognostic factors in superficial bladder cancer. Eur Urol 21:89
3. Wolf H, Hojgaard K (1983) Urothelial dysplasia concomitant with bladder turnouts as a determinant factor for future new oc- currences. Lancet 8340:134
4. Wallace DMA, Hindmarsh JR, Webb JN, Busuttil A, Hardgreave TB, Newsam JE, Chisholm GD (1979) The role of multiple mu- cosal biopsies in the management of patients with bladder can- cer. Br J Urol 51:535
5. Kiemeney LALM, Witjes JA, Heijbroek RP, Koper NR Verbeek ALM, Debruyne FMJ and the Members of the Dutch South-East Co-operative Urological Group (1994) Should random urothe- lial biopsies be taken from patients with primary superficial bladder cancer? A decision analysis. Br J Urol 73:164 6. Vicente J, Ch6chile G, Algaba F (1987) Value of in vivo muco-
sa-staining test with methylene blue in the diagnosis of pretu- moral and tumoral lesions of the bladder. Eur Urol 13:15 7. Benson RC, Farrow GM, Kinsey JH, Cortese DA, Zincke H, Utz
DC (1982) Detection and localization of in situ carcinoma of the bladder with hematoporphyrin derivative. Mayo Clin Proc 57:548
8. Kennedy JC, Pottier RH, Pross DC (1990) Photodynamic ther- apy with endogenous protoporphyrin IX: Basic principles and present clinical experience. J Photochem Photobiol B: Biol 6:143
9. Kriegmair M, Baumgartner R, Knuechel R, Steinbach P, Ehsan A, Lumper W, Hofstfidter F, Hofstetter A (1994) Fluorescence photodetection of neoplastic urothelial lesions following intra- vesical instillation of 5-aminolevulinic acid. Urology 44:836
$ 6
10. Kriegmair M, Baumgartner R, Knuechel R, Stepp H, Hofstfidter F, Hofstetter A (1996) Detection of early bladder cancer by 5-ami- nolevulinic acid induced porphyrin fluorescence. J Urol 155:105 11. Jichlinski P, Forrer M, Mizeret J, Glanzmann T, Braichotte D, Wagni~res G, Zimmer G, Guillou L, Schmidlin F, Graber P, van den Bergh H, Leisinger HJ (in press) Clinical evaluation of a method for detecting superficial transitional cell carcinoma of the bladder by light induced fluorescence of protoporphyrin IX following topical application of 5-aminolevulinic acid. Prelim- inary results. Lasers Surg Med (in press)
12. Mostofi FK, Sobin LH, Torloni H (1973) Histological typing of urinary bladder tumours. In: World Health Organisation (ed) International histological classification of tumours. WHO, Ge- neva
13. UICC (1992) TNM classification of malignant tumours, 4th edn. Springer-Verlag, Berlin Heidelberg New York
14. Nagy GK, Frable WJ, Murphy WM (1982) Classification of premalignant urothelial abnormalities. A Delphi study of the Na- tional Bladder Cancer Collaborative Group A. In: Sommers SC, Rosen PP (eds) Pathology Annual, Appleton-Century-Crofts, Norwalk, p 219
15. Levi F, La Vecchia C, Randimbison L, Franceschi S (1993) In- cidence of infiltrating cancer following superficial bladder car- cinoma. Int J Cancer 55:419
16. Abel PD (1993) Follow-up of patients with "superficial" transi- tional cell carcinoma of the bladder: the case for a change in pol- icy. Br J Urol 72:135
17. Klein R, Loy V, Huland H (1991) Residual tumor discovered in routine second transurethral resection in patients with stage T1 transitional cell carcinoma of the bladder. J Urol 146:316