Graefe's Arch Clin Exp Ophthalmol (1997) 235:10-13 © Springer-Verlag 1997
Edoardo Baglivo
Andr6 Dosso
Constantin Pournaras
Thrombus and branch retinal vein occlusion
Received: 21 March 1996
Revised version received: 23 July 1996 Accepted: 20 August 1996
E. Baglivo ( ~ ) • A. Dosso • C. Pournaras Clinique d'Ophtalmologie,
H6pital Cantonal Universitaire, Rue Alcide-Jentzer, 22, CH- 1205 Geneva, Switzerland Tel. +41-22-38.26.429; fax +41-22-382.83.82; e-mail baglivo-edoardo @ diogenes.hcuge.ch
Abstract
B r a n c h retinal vein oc- clusion ( B R V O ) is often a s s o c i a t e d with arteriosclerosis. T y p i c a l l y the o c c l u s i o n o c c u r s at an arterio- venous crossing. We r e p o r t a case o f a p r e v i o u s l y h e a l t h y patient w h o d e v e l o p e d a B R V O . F u n d u s c o p y and f l u o r e s c e i n a n g i o g r a p h y sug- gested an intravascular t h r o m b u s as the cause o f the occlusion. T h e investigations p e r f o r m e d were posi- tive for systemic h y p e r t e n s i o n andh y p e r l i p i d a e m i a . A f t e r 2 months, f u n d u s e x a m i n a t i o n revealed dis- a p p e a r a n c e o f the intravascular t h r o m b u s , resolution o f the m a c u l a r e d e m a and i m p r o v e m e n t o f the - visual acuity. C e r t a i n physiological characteristics o f the retinal circu- lation a s s o c i a t e d with h y p e r l i p i - d a e m i a and systemic h y p e r t e n s i o n a p p e a r to favour t h r o m b u s f o r m a - tion.
Introduction
Case report
A c u t e b r a n c h retinal vein o c c l u s i o n ( B R V O ) presents a characteristic clinical picture with f l a m e - s h a p e d and dot and blot h a e m o r r h a g e s , soft and hard exudates, retinal o e d e m a and a dilated vein in a s e g m e n t a l distribution. T h e o c c l u s i o n invariably appears to o c c u r at an arteri- ovenous (AV) c r o s s i n g point [9, 10]; t h i c k e n i n g o f the arterial wall and the p r e s e n c e o f a c o m m o n adventitia o f the a r t e r y and the vein at AV c r o s s i n g s s e e m to play a role in the p a t h o g e n e s i s o f the B R V O [10, 16],
T h e m a j o r risk f a c t o r is arteriosclerosis (age, systemic h y p e r t e n s i o n , diabetes mellitus, s m o k i n g , h y p e r l i p i - daemia). O t h e r p r e d i s p o s i n g factors, such as blood dyscrasias, l y m p h o - p r o l i f e r a t i v e disorders, periphlebitis (sarcoidosis, B e h c e t ' s disease, retinal infections), h y p e r - opia and o p e n - a n g l e g l a u c o m a have b e e n d e s c r i b e d [ 1 - 3 , 12, 15, 17].
We r e p o r t here the case o f a 5 3 - y e a r - o l d m a n w h o developed an o c c l u s i o n o f the superior t e m p o r a l vein. F u n d u s c o p y and f l u o r e s c e i n a n g i o g r a p h y o f the o c c l u - sion s u g g e s t e d the p r e s e n c e o f an intravascular t h r o m - bus.
A 53-year-old previously healthy man presented in December 1992 with a 2-day history of sudden decrease of visual acuity in his left eye.
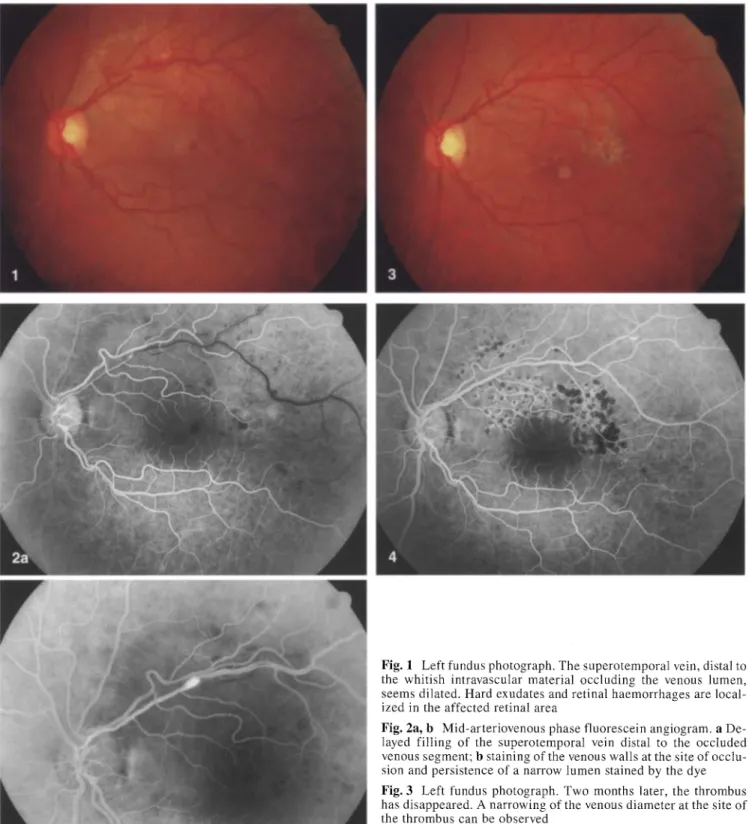
On examination, the patient's visual acuity for distance was 10/10 with -0.75 in the right eye, and the best corrected visual acuity in the left eye was 5/10. Intraocular pressure was 10 mmHg in both eyes. Results of slit-lamp examination were normal in each eye. Fundus examination of the right eye showed minimal arteriosclerosis. In the left eye, a superotemporal BRVO was noted. Whitish intravascular material was observed in a segment of the occluded vein at two disc diameters from the optic disc (Fig. 1). The fluorescein angiography showed staining of the venous wall at distance of the proximal end of the intravascular material. The hyperfluorescence was visible in the early arteri- ovenous phase and increased in the mid-phase of the angiogram. Distal to the intravascular material, the retinal venous circulation time was increased (Fig. 2a). At the site of the venous occlusion, the biomicroscopic and angiographic findings suggested that this material was an intravascular thrombus. Moreover, in this area, a breakdown of the blood-retinal barrier was observed (Fig. 2b).
We performed investigations for systemic hypertension, dia- betes mellitus, hyperlipidaemia, connective tissue disorder, Be- hcet's disease, sarcoidosis and blood dyscrasia. Results were posi- tive for systemic hypertension and hyperlidaemia [HDL choles- terol 0.52 retool/1 (n = 0.75-1.73); total cholesterol 8.03 retool/1 (n = 3.3-6.5); LDL cholesterol 4.81 mmol/1 (n = less than 3.9);
II
Fig. 1 Left fundus photograph. The superotemporal vein, distal to the whitish intravascular material occluding the venous lumen, seems dilated. Hard exudates and retinal h a e m o r r h a g e s are local- ized in the affected retinal area
Fig. 2a, b Mid-arteriovenous phase fluorescein angiogram, a De- layed filling of the superotemporal vein distal to the occluded venous segment; b staining of the venous walls at the site of occlu- sion and persistence of a narrow lumen stained by the dye Fig. 3 Left fundus photograph. Two months later, the thrombus has disappeared. A narrowing of the venous diameter at the site of the thrombus can be observed
Fig. 4 M i d - p h a s e fluorescein angiogram. The thrombus and the delayed filling of the superotemporal vein are no longer apparent
triglycerides 5.94 mmol/1 (n = 0.4-1.83)]. We excluded sec- ondary dyslipidaemia (hypothyroidism, diabetes, liver disease, re- nal disease). The patient did not drink alcohol, did not smoke and was neither obese nor a drug abuser.The systemic h y p e r t e n s i o n was treated with a calcium channel blocker and the dyslipidaemia
with hypolipaemic medication (benzylfibrate), and we introduced salicylates (100 rag/day). Dietary advice was given.
Two days later, the visual acuity of the left eye had worsened ( 3 / 1 0 ) and retinal examination showed macular oedema. Due to the persistence of the macular o e d e m a and the presence of is-
12
chaemic areas, argon laser photocoagulation was performed 6 weeks after the diagnosis.
Two months later, the visual acuity of the left eye had improved (10/10 without correction). Fundus examination showed the dis- appearance of the whitish intravascular material and a resolution of the macular oedema (Fig. 3). Fluorescein angiography revealed reperfusion of the superior temporal vein (Fig. 4). Finally, the lipidogram and the patient's blood pressure were normal.
Discussion
Leber [14] was the first to suggest the importance of arteriosclerosis and the vulnerability of AV crossing sites in BRVO. Jensen observed that the artery lay anteri- or to the vein at the majority of BRVO crossing sites and postulated that the predilection of BRVO for the super- otemporal quadrant was due to the greater number of crossings in this quadrant [ 11 ]. Others have recently con- firmed Jensen's observation of a greater percentage of artery-anterior-to-vein crossings at the BRVO sites [7, 19] and of a greater number of crossings in the super- otemporal quadrant [8]. A histopathologic study con- firmed the importance of the AV crossing at the site of the BRVO [10]. In our case, we observed, at the site of the occlusion, an intravascular white material occluding the vessel's lumen without any sign of ocular inflamma- tion. This material disappeared two months later.
These observations suggest that the cause of the oc- clusion was the presence of a thrombus. The follow-up was characterized by the disappearance of the thrombus
and the recanalisation of the superotemporal vein. As risk factors, our patient had high blood pressure and hy- perlidaemia. This seems to be the first clinical report of a BRVO caused by a thrombus.
Since the F r a m i n g h a m study [13], hyperlidaemia as an isolated predisposing factor furthering atherosclero- sis in large vessels or an ischaemic arterial stroke has been well documented [18]. Nevertheless, few studies describe venous thrombosis occurring in association with dyslipidaemia [4].
Dodson and colleagues [5, 6] found a greater preva- lence of hyperlipidaemia and hypercholesterolaemia in patients suffering from BRVO than in an age-matched group. They proposed that the increase of serum lipids may contribute to the aetiology of vein occlusion by al- tering plasma viscosity or affecting platelet function.
There is general agreement that the origin of BRVO includes both systemic factors such as hypertension and local anatomical factors such as AV crossings. However, the initial p h e n o m e n o n causing such condition is still uncertain.
In our case, the mechanical factor was absent. Whether the thrombus formation was due to abnormal blood viscosity or alteration of platelet function, induced by hyperlipidaemia, could not be ascertained. However, it appears that hyperlipidaemia and hypertension may favour intravenous thrombus formation, and the treat- ment of risk factors seems to improve the natural course of the disease.
References
1. Appiah AR Greenidge KC (1987) Factors associated with retinal vein occlusions in Hispanics. Ann Ophthal- mol 19:307-309
2. Appiah AR Trempe CL (1989) Differ- ences in contributory factors among hemicentral, central, and branch reti- nal vein occlusions. Ophthalmology 96:364-366
3. Coscas G, Dhermy P (1978) Occlu- sions veineuses r6tiniennes. (Soci6t6 fran~aise d'ophtalmologie) Masson, Paris
4. De Gennes JL, Ozanne R Turpin G (1982) Les accidents thrombo-em- boliques veineux au cours des hyper- lipid6mies idiopathiques. Nouv Presse Med 23:1777-1780
5. Dodson PM, Galton D J, Winder AF ( 1981) Retinal vascular abnormalities in the hyperlipidaemias. Trans Oph- thalmol Soc UK 101:17-21
6. Dodson PM, Galton D J, Hamilton AM, Blach RK (1982) Retinal vein occlusion and the prevalence of lipo- protein abnormalities. Br J Ophthal- tool 66:161-164
7. Duker JS, Brown GC (1989) Anterior location of the crossing artery in branch retinal vein obstruction. Arch Ophthalmol 107:998-1000
8. Feist RM, Ticho BH, Shapiro MJ, Farber M (1992) Branch retinal vein occlusion and quadratic variation in arteriovenous crossings. Am J Oph- thalmol 113:664-668
9. Finkelstein D (t989) Retinal branch vein occlusion. In: Ryan S J, Schachat AR Murphy RP, Patz A (eds) Medical retina, vol 2. Mosby, St Louis, pp 427-432
10. Frangieh GT, Green R, Barraquer- Somers E, Finkelstein D (1982) Histo- pathologic study of nine branch retinal vein occlusions. Arch Ophthalmol
1 0 0 : 1 1 3 2 - 1 1 4 0
11. Jensen VA (1936) Clinical studies of tributary thrombosis in the central retinal vein. Acta Ophthalmol Suppl
10:1-193
12. Johnston RL, Bruckner AJ, Steinmann W, Hoffmann ME, Holmes JH (I985) Risk factors of branch retinal vein oc- clusion. Arch Ophthalmol 103:1831-
1832
13. Kannel WB, Castelli WP, Gordon T, et al (1971) Serum cholesterol, lipo- proteins, and the risk of coronary heart disease. The Framingham study. Ann Intern Med 74:1-11
14. Leber T (1877) Die Krankheite der Netzhaut und des Sehnerven. In: Graefe A, Saemisch T (eds) Handbuch der Gesammten Augenheilkunde: Pathologie und Therapie. Engelmann, Leipzig, pp 521-535
13
15. McGrath MA, Wechsler F, Hunyor AB, Penny R (1978) Systemic factors contributory to retinal vein occlusion. Arch Intern Med 138:216-220 16. Orth DH, Patz A (1978) Retinal
branch vein occlusion. Surv Ophthal- tool 22:357-376
17. Rath EZ, Frank RN, Shin DH, Kim C (1992) Risk factors for retinal vein occlusions. Ophthalmology 99: 509- 514
18. The Lipid Research Clinics Coronary Primary Prevention Trial (1984) The lipid research clinics coronary prima- ry prevention trial results. 1. Reduc- tion in incidence of coronary heart disease. 2. The relationship of reduc- tion in incidence of coronary heart disease to cholesterol lowering. JAMA 251 : 351-364
19. Weinberg D, Dodwell DG, Fern SA (1990) Anatomy of arteriovenous crossings in branch retinal vein occlu- sion. Am J OphthalmoI 109:298-302