591
I
NCREASING life expectancy entails increased risks ofacquiring functional deficits and disabilities at advanced ages (1). Disabilities and functional deficits have consider-able consequences both for the affected individual and for society, as they are associated with dependency and elevated use of health and social care services (2). Therefore, promo-tion of health and prevenpromo-tion of funcpromo-tional impairment in later life are major health policy priorities.
Use of multidimensional geriatric assessment (3) and of standardized tools (4) has shown favorable effects on func-tional status in frail older persons. However, there is an
on-going debate on how prevention of functional status decline in non-frail older persons can be achieved. Health risk ap-praisal (HRA) is a potentially promising approach for a pre-ventive purpose in older persons, covering the multiple domains of multidimensional geriatric assessment in a stan-dardized tool, with a self-administered questionnaire and a computer-based feedback system (5). A systematic review of HRA showed benefits on behavior, physiological vari-ables, and general health status in older persons among studies including personalized reinforcement (6). However, experience with HRA is limited, and the few previous studies
A Randomized Trial of Effects of Health Risk Appraisal
Combined With Group Sessions or Home Visits on
Preventive Behaviors in Older Adults
Ulrike Dapp,
1Jennifer A. M. Anders,
1Wolfgang von Renteln-Kruse,
1Christoph E. Minder,
2Hans Peter Meier-Baumgartner,
1Cameron G. Swift,
3Gerhard Gillmann,
4Matthias Egger,
5John C. Beck,
6and Andreas E. Stuck,
7for the PRO-AGE Study Group
1Albertinen-Haus Geriatrics Center, Scientific Department at the University of Hamburg, Germany. 2Horten Zentrum, University of Zürich, Switzerland.
3Department of Health Care of the Elderly, Kings College London, Clinical Age Research Unit, King’s College Hospital, UK. 4Swiss Federal Statistical Office, Neuchâtel, Switzerland.
5Department of Social and Preventive Medicine, University of Bern, Switzerland. 6Langley Research Center, Los Angeles, California.
7Division of Geriatrics, Department of General Internal Medicine, Inselspital and University of Bern, Switzerland. Address correspondence to Wolfgang von Renteln-Kruse, Albertinen-Haus Geriatrics Center, Scientific Department at the University of Hamburg,
Sellhopsweg 18-22, D-22459 Hamburg, Germany. Email: w.renteln-kruse@albertinen.de
Background. To explore effects of a health risk appraisal for older people (HRA-O) program with reinforcement, we
conducted a randomized controlled trial in 21 general practices in Hamburg, Germany.
Methods. Overall, 2,580 older patients of 14 general practitioners trained in reinforcing recommendations related
to HRA-O-identified risk factors were randomized into intervention (n = 878) and control (n = 1,702) groups. Patients (n = 746) of seven additional matched general practitioners who did not receive this training served as a comparison group. Patients allocated to the intervention group, and their general practitioners, received computer-tailored written recommendations, and patients were offered the choice between interdisciplinary group sessions (geriatrician, physio-therapist, social worker, and nutritionist) and home visits (nurse).
Results. Among the intervention group, 580 (66%) persons made use of personal reinforcement (group sessions:
503 [87%], home visits: 77 [13%]). At 1-year follow-up, persons in the intervention group had higher use of preventive services (eg, influenza vaccinations, adjusted odds ratio 1.7; 95% confidence interval 1.4–2.1) and more favorable health behavior (eg, high fruit/fiber intake, odds ratio 2.0; 95% confidence interval 1.6–2.6), as compared with controls. Com-parisons between intervention and comparison group data revealed similar effects, suggesting that physician training alone had no effect. Subgroup analyses indicated favorable effects for HRA-O with personal reinforcement, but not for HRA-O without reinforcement.
Conclusions. HRA-O combined with physician training and personal reinforcement had favorable effects on
preven-tive care use and health behavior.
Key Words: Health promotion—Prevention—Elderly—Preventive home visits—Group session.
Received October 4, 2010; Accepted January 15, 2011 Decision Editor: Luigi Ferrucci, PhD, MPH
of HRA-based interventions were mostly conducted in the United States and usually included personal counseling by a health educator, personal mailing, or monetary incentives. The use of HRA is practically nonexistent as part of preven-tive health care outside the United States, probably related to limited applicability of previous U.S. studies to settings in other countries.
Based on the original HRA for the elderly (5), we gener-ated a multilingual, updgener-ated, and regionally adapted version for use in European settings, labeled HRA-O (HRA for older persons) (7). In addition, methods of personal HRA reinforcement with group sessions or preventive home vis-its adapted to the German setting were developed and im-plemented (8,9). Group sessions have been successfully tested for chronic disease management purposes (10–12), but there is little experience on the effectiveness of this ap-proach for a preventive purpose.
The objectives of this trial were to evaluate the feasibility and acceptance of the HRA-O instrument combined with physician training and with group sessions or preventive home visits, and to determine the short-term effects of this multifaceted intervention on preventive care use and health behavior in older persons.
Methods
The present study is one of three trials that took place in the context of the PRO-AGE (PRevention in Older people— Assessment in GEneralists’ practices) project in three loca-tions (7,13). The present study was conducted in Hamburg, Germany, and was intended to test whether HRA-O, com-bined with personal reinforcement and supplemented by a quality circle (special educational program) for the involved physicians, improves use of preventative care and health behavior. Ethical approval was obtained from the Hamburg General Medical Council Ethics Committee and the Alber-tinen-Hospital Ethics Committee.
Recruitment of General Practitioners
In Hamburg, general practitioners (GPs) registered in the entire metropolitan area (~500 GPs) were informed via the newsletter of their regional GP association (BDA-Landes-verband Hamburg). Overall, 21 GPs (organized in solo practices) agreed to participate. We formed seven clusters of three GPs each, matched for physician’s age, gender, and qualification (family practice, internal medicine). Two GPs from each cluster were allocated to the training group (14 GPs), and one to the comparison group (7 GPs).
Recruitment of Older Persons
Each participating practice provided a complete list of the patients 60 years and older, excluding those with need for human help (eg, professional care) in basic activities of daily living and/or receiving nursing care, cognitive impairment,
terminal disease, and/or inability to understand German. Eligible patients were sent a letter of invitation by their phy-sician, including an information sheet describing the project, a brief questionnaire including the Pra-questionnaire (Prob-ability of Repeated Admission) with six items measuring baseline risk status (14), a self-reported question on need for human help in basic activities of daily living (persons with self-reported need for help were excluded from the study), and an informed consent form. Patient’s age and sex were obtained from the GP’s register. All patients were in-formed that they could withdraw from the project without negative impact on their care. Recruitment took place over a 9-month period.
Group Assignment of Older Persons
Eligible persons from the 14 practices of the trained GPs who returned both the brief questionnaire and the consent form were allocated to the intervention and the control group relying on computer-based randomization at an inde-pendent center. We selected a randomization ratio of 1:2 (intervention:control) to minimize the number of persons in the intervention group (resources for offering the interven-tion reinforcement services were limited). Persons living in the same household were allocated to the same group. Eli-gible persons from the seven remaining practices were not randomized and formed the comparison group. The detailed flow diagram describing patient numbers in the recruitment and allocation phase has been described in a separate Meth-ods article (13). An abbreviated flow diagram with addi-tional detailed information on the follow-up period is depicted in Supplementary Figure 1.
Intervention
HRA-O intervention.—Intervention group members re-ceived the self-administered HRA-O questionnaire immedi-ately after randomization. Briefly, the HRA-O questionnaire contains the following sections (7): administrative informa-tion, chronic conditions, preventative care use, medication use, signs and symptoms, self-perceived health, physical activity, nutrition, injury prevention, tobacco use, alcohol use, vision, hearing, depressive symptoms, memory, social network, social support, basic and instrumental activities of daily living, socioeconomic information education, occupa-tion, living arrangement, and health measurements (weight, height, blood pressure, and cholesterol).
Completed questionnaires were double entered at the study center, and individualized computer-generated feedback re-ports were produced for participants and their GPs. Participant’s reports included individually tailored information and recom-mendations based on the older persons’ responses, general health information in the domains of the HRA-O question-naire, and local sources of further information (7).
All 14 GPs allocated to training participated in bimonthly 2-hour training sessions (Thursday evenings 8–10 pm) led by an experienced geriatrician during the whole interven-tion period. The main purpose was to train them in reinforc-ing recommendations related to HRA-O-identified risk factors and to make them aware of the reinforcement pro-gram offered by the geriatric center. As a basis for these training sessions, we used cases from GPs practices, and a newly developed evidence-based manual with guidance notes for GPs participating in the intervention (published as part of reference 13). Key topics of the training included cardiovascular risk prevention, immunizations, cancer screening, health maintenance, specific health issues (pain, medication use, injury, incontinence), and psychosocial health and behavior. As an incentive, physicians participat-ing in the trainparticipat-ing sessions received credits required for their documentation of continuing education.
For their patients allocated to the intervention, but not for those allocated to control (Supplementary Figure 1), the GPs received a personal summary report with personal in-formation on recommendations based on HRA-O-identified risk factors. Patients were encouraged to discuss HRA-O-based recommendations with their GPs, but it was up to the GPs and the participants to decide how the issues raised in the reports were addressed: directly, opportunistically, or not at all.
Additional personal reinforcement.—Patients of the in-tervention group having returned the HRA-O questionnaire had the choice between two offers of reinforcement: par-ticipation in group sessions or home visits. The present study made use of the health care structures and professions established in Germany, and of the interdisciplinary geriat-ric team located at a geriatgeriat-ric center, trained in health pro-motion and motivational methods.
Group session.—Groups of 12 seniors took part in one half-day group session at the geriatric center. Information on healthy eating, physical activity, active social participa-tion, and successful aging was provided in group sessions by the geriatric team: nutritionist, physiotherapist, social worker, and geriatrician (team leader) (8,9). First, geriatric team members gave structured information about the se-lected health topics, and the complex interactions between health topics. Second, each person was asked to complete an individual dietary and physical activity record. Such self-reflection of participants proved helpful to the four advisors of the geriatric team for developing individual recommen-dations and setting individual goals (preventive assess-ment). Two weeks later, all participants received a personal report with recommendations confirming the agreements reached during the group session, including individually se-lected addresses of, for example, sports clubs and senior citizens’ organizations close to the participant’s home to promote lasting lifestyle changes (motivation, self-efficacy,
empowerment). Group session participants were offered a second follow-up appointment at the geriatric center in 6 months’ time to check adherence to the recommendations.
Home visits.—A specially trained nurse conducted a first home visit including a multidimensional assessment of mo-bility, functional decline, falls, pain, medication use, nutri-tion, cogninutri-tion, vision, hearing, social contacts, housing, and living location. Based on this assessment and the HRA-O feedback report, the nurse discussed each case with the geriatric team at the center. Recommendations were formu-lated, prioritized, reinforced, or modified for each partici-pant. Nurse and geriatrician provided the participant’s GP with a short written report containing the assessment results and recommendations given. Intensive cooperation between nurse, social worker, and GP resulted in finding solutions for special needs uncovered during home visits (eg, meals on wheels, application for nursing care). The nurse conduct-ed a second follow-up home visit after 6 months to check adherence to the recommendations (15,16).
Control Group
Participants randomized to control received usual care over the study period, but GPs of control patients had re-ceived special training and were involved in care of inter-vention group patients, and might therefore have changed their preventive care practice. Such a treatment contamina-tion of control group patients might reduce the point esti-mate of the intervention’s effectiveness, and this might lead to underestimation of treatment effects.
Comparison Group
Due to the concern regarding a diffusion of treatment effects among control group patients, we recruited seven additional practices not involved in the intervention, did not offer special training to these GPs, and allocated all participants from these untrained GPs to usual care. This patient group was therefore not exposed to a possible con-tamination effect and was called “comparison group” in this study. From this perspective, comparisons between in-tervention and comparison group patients are expected to give more appropriate estimates of intervention effects. However, these comparisons have a limited validity be-cause they are based on initial matched physician alloca-tion with subsequent invitaalloca-tion of patients for study participation.
Outcome Data Collection
Survival, nursing home admission, and need for ambula-tory nursing care as well as change of residence data were obtained from the GP records and completed with partici-pant and proxy information. At year 1, the HRA-O ques-tionnaire was used for collecting outcome information from
all study participants. It was sent to surviving persons in combination with a short questionnaire on self-efficacy in the patient–physician interaction (17). All data were double entered by staff blinded for subject allocation.
Primary outcomes were self-reported use of preventive care measures and self-reported health behavior at year 1 follow-up (13,18–20). Two summary scores, one each for preventive care (preventive care use index) and for health behavior (health behavior index), were created. The preven-tive care use index was calculated for each person as the proportion of preventive care services that were used by this person. For example, if a person reported use of six of the nine preventive care services listed in this study, the index was 66.7%. Similarly, the health behavior index was calcu-lated as the proportion of favorable health behavior items among the six items addressed in this study. For physical activity, the five-or-more-times-per-week cutoff was used for calculating the index.
All other measures, including HRA-O items covering health and functional status measures (7), measures of pa-tient–physician interaction (17), mortality, and nursing home use at 1-year follow-up, were used for secondary out-come analyses.
Sample Size
We calculated the sample size required to detect a 30% difference in preventive care use or health behavior between the intervention and the control groups at year 1, using a = .05 and a power of 80%. Prevalence of positive preventive care use or health behavior was assumed at 20% among controls. Assuming a 20% dropout rate during year 1, the required sample size was 763 and 1,525 persons, respec-tively, in the intervention and control groups.
Statistical Methods
Main analyses were comparisons of primary outcomes between intervention and control groups, adjusted for base line factors (age, gender, and the individual items of the Pra-questionnaire) and household membership (a variable identifying persons living in the same household), based on generalized estimating equations assuming an independent correlation structure (21). To explore whether treatment ef-fects were underestimated due to diffusion, we repeated all analyses of primary outcome data by comparing interven-tion versus comparison groups. Secondary outcomes were compared between intervention and control groups based on the same method. For the analysis of health care use in-formation (physician visits, hospital use), an ordinal regres-sion model was used. All analyses were done according to an a priori plan (13) using SAS version 9.1 and STATA version 11.1.
To investigate potential bias introduced by missing data, we repeated all primary outcome analyses comparing inter-vention, control, and comparison groups, and the secondary
outcomes of health and functional status comparing inter-vention and control groups, based on multiple imputation of missing values by chained equations (22). The chosen pre-dictor variables for the imputation model included gender, age, individual and summary items of baseline Pra-instru-ment, 1-year follow-up preventive care items and summary score, 1-year follow-up health behavior measures and sum-mary score, 1-year follow-up health and functional status measures, an indicator of the completion of the 1-year fol-low-up questionnaire (yes/no), and group affiliation (inter-vention, control, or comparison). Ten completed data sets were generated.
We also conducted planned subgroup analyses. Based on previous research, we hypothesized favorable effects for the combination of HRA-O and personal reinforcement, but no favorable effects for HRA-O without personal reinforce-ment. For this purpose, we used generalized estimation equations, controlling for household clusters, and did these analyses based on intervention versus control group com-parisons, using the two main summary outcome measures (preventive care index and health behavior index). The model included categorical variables with levels denoting (a) participation in the full intervention consisting of HRA-O with personal reinforcement (group session or home visit), (b) partial participation in the intervention with com-pletion of HRA-O but without personal reinforcement (HRA-O intervention alone), and (c) usual care and no in-tervention (corresponds to control group). The fourth cate-gory of persons (intervention group who refused to participate in the intervention, n = 74) could not be included in this analysis because persons refusing the intervention also refused providing self-reported outcome data.
Results
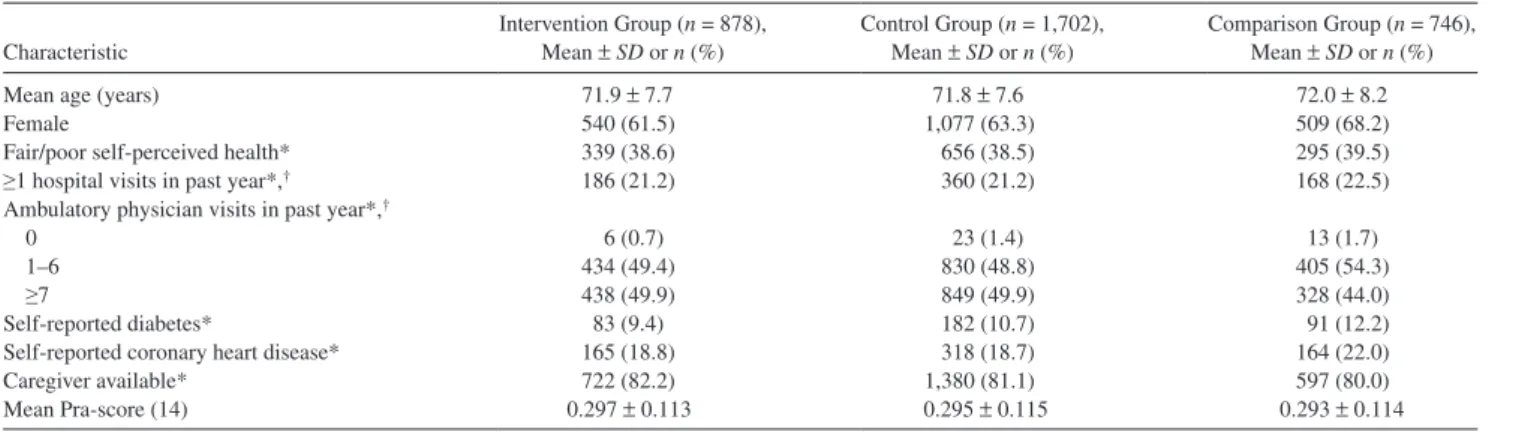
The number of participants agreeing to participate was 2,580 among those included in the randomized study and 746 in the concurrent comparison group (Supplementary Figure 1). At 1-year follow-up, the numbers (percent of eligible) returning the HRA-O questionnaire were 587 (70.6%) in the intervention group, 1,376 (83.8%) in the randomized control group, and 582 (81.4%) in the com-parison group. Information regarding survival and place of living was available for nearly all persons (missing: n = 17) (see Supplementary Figure 1 for detailed flow diagram). Table 1 demonstrates that all three groups had similar base-line characteristics.
Of 878 individuals in the intervention group, 74 did not return the HRA-O instrument at baseline, and did therefore not participate in the intervention. The remaining 804 per-sons received computer-generated individualized reports, and they were invited to make use of group sessions or pre-ventive home visits. Overall, 503 chose group sessions, 77 opted for home visits, and the remaining 224 did not par-ticipate in any reinforcement intervention.
Preventive Care Use at Year 1
For preventive care measures, differences were statisti-cally significant for the three actions with the lowest uptake among control patients (influenza vaccination, p < .001; pneumococcal vaccination, p < .001; and hearing checks,
p = .001) (Table 2). The fraction of preventive care measures taken up at the 1-year follow-up was 74.9% among persons
in the intervention group, versus 68.4% in the control group (p < .001).
Differences between intervention and comparison groups were similar compared with differences between interven-tion and control groups, suggesting little treatment diffu-sion. The only possible exception was hypertension control (Table 2), but these data should not be overinterpreted given Table 1. Baseline Characteristics of Study Participants
Characteristic
Intervention Group (n = 878),
Mean ± SD or n (%) Control Group (n = 1,702), Mean ± SD or n (%) Comparison Group (n = 746), Mean ± SD or n (%)
Mean age (years) 71.9 ± 7.7 71.8 ± 7.6 72.0 ± 8.2
Female 540 (61.5) 1,077 (63.3) 509 (68.2)
Fair/poor self-perceived health* 339 (38.6) 656 (38.5) 295 (39.5)
≥1 hospital visits in past year*,† 186 (21.2) 360 (21.2) 168 (22.5)
Ambulatory physician visits in past year*,†
0 6 (0.7) 23 (1.4) 13 (1.7)
1–6 434 (49.4) 830 (48.8) 405 (54.3)
≥7 438 (49.9) 849 (49.9) 328 (44.0)
Self-reported diabetes* 83 (9.4) 182 (10.7) 91 (12.2)
Self-reported coronary heart disease* 165 (18.8) 318 (18.7) 164 (22.0)
Caregiver available* 722 (82.2) 1,380 (81.1) 597 (80.0)
Mean Pra-score (14) 0.297 ± 0.113 0.295 ± 0.115 0.293 ± 0.114
Notes: *Item contributing to the Pra-score.
† Hospital and physician visits in the year prior to baseline, based on self-reported information.
Table 2. Primary Outcomes at 1-Year Follow-Up*
Intervention Group, Cases/n (%) Control Group, Cases/n (%) Intervention vs Control, OR (95% CI) Comparison Group, Cases/n (%) Intervention vs Comparison, OR (95% CI) Preventive action
Blood pressure check in previous year 565/573 (98.6) 1,320/1,355 (97.4) 1.5 (0.7–3.3) 547/576 (95.0) 3.3 (1.5–7.3) Blood glucose measurement in
previous 3 years
514/567 (90.7) 1,194/1,329 (89.8) 1.0 (0.7–1.5) 486/562 (86.5) 1.4 (1.0–2.2) Cholesterol measurement in
previous 5 years† 382/401 (95.3) 884/943 (93.7) 1.3 (0.7–2.2) 381/413 (92.3) 1.5 (0.8–2.8) Dental checkup in past year 504/575 (87.7) 1,137/1,346 (84.5) 1.3 (0.9–1.7) 485/573 (84.6) 1.2 (0.8–1.8) Vision checkup in past year 451/574 (78.6) 1,017/1,353 (75.2) 1.2 (0.9–1.5) 446/574 (77.7) 1.0 (0.8–1.4) Colon cancer screening
(fecal occult blood in past year)‡ 343/486 (70.6) 782/1,158 (67.5) 1.1 (0.9–1.4) 341/495 (68.9) 1.0 (0.8–1.4) Influenza vaccination in past year 395/574 (68.8) 768/1,353 (56.8) 1.7 (1.4–2.1) 321/573 (56.0) 1.7 (1.3–2.2) Hearing checkup in past year 248/575 (43.1) 471/1,353 (34.8) 1.4 (1.2–1.8) 176/574 (30.7) 1.7 (1.3–2.2) Pneumococcal vaccination (ever) 267/568 (47.0) 319/1,342 (23.8) 2.8 (2.3–3.5) 167/566 (29.5) 2.0 (1.5–2.7) Preventive care use index (mean ± SD)§ 74.9 ± 18.4 (n = 570) 68.4 ± 17.8 (n = 1,334) D = 6.1 (4.3–7.9) 68.0 ± 19.4 (n = 569) D = 6.0 (3.8–8.3) Health behavior
Use of car safety belt 534/558 (95.7) 1,237/1,287 (96.1) 0.9 (0.5–1.5) 526/549 (95.8) 0.9 (0.5–1.7) No tobacco use 479/536 (89.4) 1,069/1,246 (85.8) 1.4 (1.0–1.9) 445/522 (85.2) 1.6 (1.1–2.3) No hazardous alcohol use (18) 453/525 (86.3) 1,038/1,235 (84.0) 1.2 (0.9–1.7) 435/508 (85.6) 1.1 (0.7–1.6) Low fat intake (19) 354/530 (66.8) 812/1,268 (64.0) 1.1 (0.9–1.4) 331/510 (64.9) 1.2 (0.9–1.6) Moderate or strenuous
physical activity (20)
≥3 times per week 204/541 (37.7) 395/1,265 (31.2) 1.4 (1.1–1.7) 189/523 (36.1) 1.1 (0.9–1.5) ≥5 times per week 112/537 (20.9) 235/1,255 (18.7) 1.2 (0.9–1.5) 113/518 (21.8) 1.0 (0.7–1.4) Consumption of ≥5 fruit or fiber items
per day (19)
146/558 (26.2) 194/1,292 (15.0) 2.0 (1.6–2.6) 95/542 (17.5) 1.8 (1.3–2.4) Health behavior index (mean ± SD)§ 64.1 ± 17.1 (n = 525) 60.3 ± 16.7 (n = 1,240) D = 3.7 (2.0–5.4) 61.5 ± 17.8 (n = 499) D = 3.3 (1.2–5.5)
Notes: CI = confidence interval; OR = odds ratio. D = difference with 95% CI. Items are listed in rank order of control group prevalence. OR >1 and D >0 denote favorable intervention effect. Results are based on general estimation equation adjusted for household clusters and baseline factors.
* Numbers are number of persons reporting action or behavior or number of persons with available response (percentage). Example: 565 persons of 573 (98.6% of 573) persons in the intervention group reported that they had a blood pressure check in previous year.
† Reference group: persons aged <75 years. ‡ Reference group: persons aged <80 years.
large confidence intervals (CIs) and high control group ad-herence rates.
Repetition of all analyses for preventive care outcomes with imputed data sets revealed similar differences. For ex-ample, based on multiple imputation analyses, the preven-tive care index (mean ± standard deviation) was 74.7% ± 18.4% (intervention group) and 68.3% ± 17.7% (control group), with a resulting difference of 6.0% (95% CI 4.2%– 7.7%, p < .001).
Health Behavior at Year 1
Both the intervention group and control group showed low percentages of tobacco (10.6% vs 14.2%) and hazard-ous alcohol use (13.7% vs 16.0%) as well as high percent-ages of safety belt use (95.7% vs 96.1%) at year 1, and there were no significant differences in these. For all health be-haviors except safety belt use, the directional trend was to-ward improved activity in interventions versus controls. There were significantly higher percentages in the interven-tion group of recommended levels of three or more times of moderate to strenuous physical activity per week (p = .006) and consumption of five or more fruit or vegetable items per day (p < .001). In the intervention group, the mean health behavior index was 64.1%, versus 60.3% in the control group (p < .001) (Table 2).
Differences between intervention and comparison groups were similar compared with differences between interven-tion and control groups (Table 2), suggesting that no treat-ment diffusion occurred.
Results with imputed data sets for health behavior re-vealed similar differences. For example, based on imputa-tion analyses, the health behavior index (mean ± standard deviation) was 63.6% ± 16.8% (intervention group) and 60.3% ± 16.4% (control group), with a resulting difference of 3.3% (95% CI 1.7%–5.0%, p ≤ .001).
Subgroup Analyses
Subgroup analysis revealed a difference of the preventive care index between persons receiving the full intervention (completion of HRA-O combined with participation in group sessions or home visits) and those receiving usual care of 7.1% (95% CI 5.2%–9.0%, p < .001), and a differ-ence of the health behavior index of 4.9% (95% CI 3.1%– 6.7%, p < .001). In contrast, the comparisons between persons who only partially participated in the intervention (HRA-O intervention alone without personal reinforcement) and control groups (reference group) were statistically non-significant (difference in preventive care index: 2.0%, 95% CI −2.2 to 6.3, p = .350; difference in health behavior index: −1.8%, 95% CI −5.8 to 2.1, p = .362). These results suggest that only the combination of HRA-O with personal rein-forcement had favorable effects, with no evidence of favor-able effects of interventions consisting of HRA-O alone.
Secondary Outcomes
There were no significant differences between interven-tion and control groups in mortality, nursing home admis-sion, need for ambulatory nursing care, hospital admissions, frequencies of physician visits, or patient–physician inter-action scores during the first year after the intervention (for number of deaths and nursing home admissions, see Sup-plementary Figure 1). Full case and imputed analyses re-vealed favorable effects of the intervention for several health and functional measures at 1-year follow-up, such as self-reported health, mobility, vision, and falls (see Supple-mentary Table 3 for detailed results).
Discussion
This study demonstrates consistent, moderately favorable effects of this newly developed regionally adapted approach of HRA-O with personal reinforcement on preventive care uptake and health behaviors in nondisabled older persons. This adds evidence to previous research demonstrating that HRA-O combined with reinforcement has favorable effects and to previous studies demonstrating that preventive pro-grams in non-frail older persons (6,24), but not those in frail older persons (25,26), have favorable effects.
The intervention tested in this trial was complex, con-sisting of three main components with tailored feedback to older persons, involvement of GPs (training sessions for GPs and individualized checklists for GPs with preventive recommendations for each patient), and additional per-sonal reinforcement (group sessions or home visits). Sub-group results of the randomized study reveal that persons who did not receive the full intervention package (tailored feedback and GP involvement alone, without personal re-inforcement) did not benefit from the intervention. The ad-ditional observation that treatment effects did not diffuse to control group patients suggests that the isolated training offered to GPs does not affect preventive care use. These findings add to the literature and are in contrast to other studies demonstrating that intense physician training might modify physician behavior (27), or tailored written recom-mendations might successfully improve patient behavior (28). However, the majority of this previous research was based on single and not on multiple risk factor intervention studies.
The group session approach presented in this study is a novel and promising method of personal reinforcement in health promotion and preventive care in old age. The major-ity of older persons selected group sessions, and not preven-tive home visits, as a method of reinforcement. It is likely that the favorable effects of the intervention package ob-served in this study were related to the additional effects of group sessions, but due to the small number of home visits, analyses of the distinct effects of group sessions and home visits were not done. Further research exploring effects of this novel approach of group sessions are likely promising.
The results of this study differ from the findings of a par-allel randomized controlled study of HRA-O conducted in London, UK (29,30). In the London study, HRA-O was largely ineffective for improving health behavior and pre-ventative care uptake in older people. The findings of the present Hamburg study suggest this difference may reflect the effects of the additional reinforcement programs offered to intervention group persons. In the London study, HRA-O was integrated into the electronic health care record in the primary care system, but any reinforcement was discretion-ary, rather than programmed as described here.
The present study also found favorable effects of the in-tervention for several health and functional measures as-sessed. These results are promising, possibly indicating the potential of this intervention to prevent or postpone the on-set of disability over longer time periods. However, these results should be interpreted with caution because these were secondary outcomes, and subject to the problem of multiple testing. As expected, no significant differences be-tween intervention and control group in mortality, nursing home admission, and need for ambulatory nursing care or hospital admissions in the first year of follow-up were found. In fact, the present study was not powered to detect differences in these outcomes, and we hypothesized on the basis of previous studies of multidimensional geriatric assessment (23,24,31) that more extended follow-up be required for impact on these outcomes.
Missing data are a potential limitation of this study. Non response for primary outcome data was relatively high and differed between treatment groups. We can only hypothe-size about the reason for this difference between groups be-cause outcome data were collected with mailed questionnaires. It is likely that this difference is related to the study design: intervention group patients, but not pa-tients in control or comparison groups, had to complete the full HRA-O questionnaire at baseline as the basis for the intervention. At the time of 1-year follow-up, it was there-fore the second time intervention group patients were asked to complete the HRA-O questionnaire, resulting in an in-creased fraction of nonresponding persons. Despite these missing data aspects, several aspects support the validity of our findings. First, baseline factors were available for all study participants (no missing data) and did not reveal dif-ferences between groups. Second, not only were favorable treatment effects found in the comparison between inter-vention and control groups, but consistently in comparisons between intervention and comparison groups as well. Third, the results of the complete case analyses were confirmed in state-of-the-art imputation analyses based on an extensive database. Overall, these factors strongly suggest that ob-served effects are not due to missing data bias but are true intervention effects.
This study has both research and practice implications. Further research is needed to identify modifiable health risk factors (32), and to test various HRA-O and group session
approaches to attain favorable longer-term effects on health. This research is highly relevant for practice implementa-tion. It is consistent with research on comprehensive care for older adults, demonstrating that multifaceted care man-agement approaches, involving physicians and other health professionals, and addressing patient empowerment, con-tribute to improved quality of preventative and medical care (33,34). Practice implementation of the type of intervention tested in this study might have relevant impact on the pre-vention of disability in older persons.
Funding
This work was supported by the European Union (Brussels, QLK6-CT-1999-02205); the Federal Education and Science Ministry (Bern, Swit-zerland, BBW 990311.1); the Bundesministerium für Familie, Senioren, Frauen und Jugend, Berlin; the Max und Ingeburg Herz Stiftung, Ham-burg; and the Robert Bosch Stiftung, Stuttgart.
Supplementary Material
Supplementary material can be found at: http://biomedgerontology. oxfordjournals.org/
Acknowledgments
Additional members of the PRO-AGE study group—Germany: Norbert Lübke, Susann Laub, Kim Gihsa, and Stefan Golgert; UK: Steve Iliffe, Kalpa Kharicha, and Danielle Harari; Switzerland: Stephan Born, André Moser, Thomas Münzer, Jan Wagner, and Stefan M. Goetz. Our special thanks go to the persons in charge of the funding of Gesa Hansen, Petra Weritz-Hanf, Ingeburg Herz, Wolfgang Herz, and Almut Satrapa-Schill. We are grateful to all members of staff in the participating GP practices, the president and vice president of the Hamburg Association of General Practitioners, and the General Medical Council of Hamburg for their support. International Standard Randomized Controlled Trial Number: ISRCTN 28458424.
References
1. Keeler E, Guralnik JM, Tian H, Wallace RB, Reuben DB. The impact of functional status on life expectancy in older persons. J Gerontol A
Biol Sci Med Sci. 2010;65:727–733.
2. Vita AJ, Terry RB, Hubert HB, et al. Aging, health risks, and cumula-tive disability. N Engl J Med. 1998;338:1035–1041.
3. Wieland D, Ferrucci L. Multidimensional geriatric assessment: back to the future. J Gerontol A Biol Sci Med Sci. 2010;63:272–274. 4. Bernabei R, Landi F, Onder G, Liperoti R, Gambassi G. Second and
third generation assessment instruments: the birth of standardization in geriatric care. J Gerontol A Biol Sci Med Sci. 2008;63:308–313. 5. Breslow L, Beck JC, Morgenstern H, et al. Development of a health
risk appraisal for the elderly (HRA-E). Am J Health Promot. 1997;11: 337–343.
6. RAND 2000. Rand Corporation: Health Risk Appraisals and
Medi-care. Evidence Report and Evidence-Based Recommendations; Balti-more, MD:: U.S. Department of Health and Human Services; 2000. 7. Stuck AE, Kharicha K, Dapp U, et al. Development, feasibility and
performance of a health risk appraisal questionnaire for older persons.
BMC Med Res Methodol. 2007;7:1.
8. Dapp U, Anders J, Renteln-Kruse von W, et al. Active health promo-tion in old age: methodology of a preventive intervenpromo-tion programme provided by an interdisciplinary health advisory team for independent older people. J Public Health. 2005;13:122–127.
9. Meier-Baumgartner HP, Dapp U, Anders J. Aktive
Gesundheitsförder-ung im Alter. Ein neuartiges Präventionsprogramm für Senioren, 2nd ed. Stuttgart, Germany: Kohlhammer; 2006.
10. Lorig KR, Ritter PL, Laurent DD, et al. Long-term randomized controlled trials of tailored-print and small-group arthritis self- management interventions. Med Care. 2004;42:346–354.
11. Pitkälä KH, Routasalo P, Kautiainen H, Tilvis RS. Effects of psycho-social group rehabilitation on health, use of health care services, and mortality of older persons suffering from loneliness. J Gerontol A Biol
Sci Med Sci. 2010;65:792–800.
12. Rejeski WJ, Marsh AP, Chmelo E, et al. The Lifestyle Interventions and independence for Elders Pilot (LIFE-P). J Gerontol A Biol Sci
Med Sci. 2010;64:462–467.
13. Stuck AE, Kharicha K, Dapp U, et al. The PRO-AGE study: an inter-national randomised controlled study of health risk appraisal for older persons based in general practice [ISRCTN28458424]. BMC Med Res
Methodol. 2007;7:2.
14. Wagner JT, Bachmann LM, Boult C, et al. Predicting the risk of hos-pital admission in older persons—validation of a brief self-adminis-tered questionnaire in three European countries. J Am Geriatr Soc. 2006;54:1271–1276.
15. Renteln-Kruse von W, Anders J, Dapp U, et al. Präventive Hausbe-suche durch eine speziell fortgebildete Pflegefachkraft bei 60jährigen und älteren Personen in Hamburg. Z Gerontol Geriat. 2003;36: 378–391.
16. Meier-Baumgartner HP, Anders J, Dapp U. Präventive Hausbesuche.
Gesundheitsberatung für ein erfolgreiches Altern; Hannover, Ger-many: Vincentz; 2005.
17. Maly RC, Frank JC, Marshall GN, et al. Perceived efficacy in patient physician interactions (PEPPI): validation of an instrument in older persons. J Am Geriatr Soc. 1998;46:889–894.
18. Babor TF, de la Fuente JR, Saunders J, Grant M. AUDIT—The Alcohol
Use Disorders Identification Test: Guidelines for Use in Primary Health Care. Geneva, Switzerland: World Health Organization; 1992. 19. Stoy DB, Curtis RC, Dameworth KS, et al. The successful recruitment of elderly black subjects in a clinical trial: the CRISP experience. Cho-lesterol Reduction in Seniors Program. J Natl Med Assoc. 1995;87: 280–287.
20. Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activ-ity Scale for the Elderly (PASE): development and evaluation. J Clin
Epidemiol. 1993;46:153–162.
21. Liang KY, Zeger SL. Longitudinal data analysis using generalized lin-ear models. Biometrika. 1986;73:13–22.
22. Royston P. Multiple imputation of missing values: update. Stata J. 2005;5:188–201.
23. Meinck M, Lübke N, Lauterberg J, et al. Preventive home visits to the elderly: systematic review of available evidence. Gesundheitswesen. 2004;66:732–738.
24. Huss A, Stuck AE, Rubenstein LZ, et al. Multidimensional geriatric assessment: back to the future. Multidimensional preventive home visit programs for community-dwelling older adults: a systematic re-view and meta-analysis of randomized controlled trials. J Gerontol A
Biol Med Sci. 2008;63:298–307.
25. van Hout HPJ, Jansen APD, van Marwij HWJ, Pronk M, Frijters DF, Nijpels G. Prevention of adverse health trajectories in a vulnerable elderly population through nurse home visits. J Gerontol A Biol Sci
Med Sci. 2010;65:734–742.
26. Bouman A, van Rossum E, Evers S, Ambergen T, Kempen G, Knip-schild P. Effects on health care use and associated cost of a home visit-ing program for older people with poor health status. J Gerontol A
Biol Sci Med Sci. 2010;63:291–297.
27. Grimshaw JM, Shirran L, Thomas R, et al. Changing provider behav-ior: an overview of systematic reviews of interventions. Med Care. 2001;39(suppl 2):112–145.
28. Oenema A, Brug J, Dijkstra A, de Weerdt I, de Vries H. Efficacy and use of an internet-delivered computer-tailored lifestyle intervention, targeting saturated fat intake, physical activity and smoking cessation: a randomized controlled trial. Med Care. 2008;35:125–135. 29. Stuck AE, Elkuch P, Dapp U, et al. Feasibility and yield of a
self-ad-ministered questionnaire for health risk appraisal in older people in three European countries. Age Ageing. 2002;31:463–467.
30. Harari D, Iliffe S, Kharicha K, et al. Promotion of health in older peo-ple: a randomised controlled trial of health risk appraisal in British general practice. Age and Ageing. 2008;37:565–571.
31. Diehr P, Hirsch C. Health benefits of increased walking for sedentary, generally healthy older adults. J Gerontol A Biol Sci Med Sci. 2010;65: 982–989.
32. Shah RC, Buchman AS, Boyle PA, et al. Musculoskeletal pain is associated with incident mobility disability in community-dwelling elders. J Gerontol A Biol Sci Med Sci. 2011;66:82–88.
33. Marsteller JA, Hsu YJ, Reider L, et al. Physician satisfaction with chronic care processes: a cluster-randomized trial of guided care. Ann
Fam Med. 2010;8:308–315.
34. Boult C, Green AF, Boult LB, Pacala JT, Snyder C, Leff B. Successful models of comprehensive care for older adults with chronic condi-tions: evidence for the Institute of Medicine’s “retooling for an aging America” report. J Am Geriatr Soc. 2009;57:2328–2337.