and sharing with colleagues.
Other uses, including reproduction and distribution, or selling or
licensing copies, or posting to personal, institutional or third party
websites are prohibited.
In most cases authors are permitted to post their version of the
article (e.g. in Word or Tex form) to their personal website or
institutional repository. Authors requiring further information
regarding Elsevier’s archiving and manuscript policies are
encouraged to visit:
Disponible
en
ligne
sur
ScienceDirect
www.sciencedirect.com
Short
clinical
case
Spinal
infections
due
to
Eikenella
corrodens:
Case
report
and
literature
review
Infections
spinales
à
Eikenella
corrodens
:
à
propos
d’un
cas
et
résumé
de
la
littérature
C.
Yetimoglu
a,∗,
P.
Rafeiner
b,
D.
Engel
a,
J.-Y.
Fournier
aaServicedeneurochirurgie,hôpitalCantonaldeSt.Gall,RorschacherStrasse95,9007St.Gall,Switzerland bCliniquedemedicineinterne,hôpitaldeZofingen,4800Zofingen,Switzerland
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:Received21November2012
Receivedinrevisedform26February2014 Accepted29March2014
Availableonline27May2014 Keywords:
Spinalinfection Eikenellacorrodens Cervicalspondylitis Surgicalsiteinfection
a
b
s
t
r
a
c
t
SpinalinfectionswithEikenellacorrodensarerare.Wereportauniquecaseofinfectioncausedby
E.corrodensdiagnosedmorethantwoyearsaftercervicalsurgery.Allotherpublishedcasesofspinal
infections caused by E.corrodens were searched. Characteristics of this bacterium, itschallenging
diagnosisandtherapyarediscussed.
©2014ElsevierMassonSAS.Allrightsreserved.
Motsclés: Infectionspinale Eikenellacorrodens Spondylodiscitecervicale Infectiondusitechirurgical
r
é
s
u
m
é
L’infectionspinaleàEikenellacorrodensestrare.Cetarticlerapporteuncasd’infectionàE.corrodens
survenuplusdedeuxansaprèschirurgiecervicale.Parailleurs,nousanalysonslesautrescas
pub-liésd’infectionsspinalesàE.corrodens.Lescaractéristiquesprincipalesdecegermesontdécriteset,
comptetenudesdifficultésd’isolementdecettebactérieenculturestandard,nousdiscutonslesoutils
diagnostiques.
©2014ElsevierMassonSAS.Tousdroitsréservés.
1. Introduction
Eikenellacorrodensisaubiquitousbacteriumoftheoralflora.
Furthermore, it colonizes the gastrointestinal and the
genito-urinarytract.APubMedliteraturesearchrevealedonlytencasesof
spinalinfectionscausedbythisbacterium(Table1).Onlyonecase
oflumbarinfectionaftersurgeryandonecaseofspontaneous
cer-vicalspondylodiscitiswithoutpriorsurgeryhavebeenreported.A
cervicalinfectionwithE.corrodensafteraneurosurgical
interven-tionhasnotbeendescribedtodate.
∗ Correspondingauthor.
E-mailaddress:cem.yetimoglu@kssg.ch(C.Yetimoglu).
2. Observation
A47-year-oldfemaledeskclerkwasseeninouroutpatientclinic
withthechiefcomplaintofcervicobrachialgia.Themajorcervical
painexistedforhalfayearandwasoftenaccompaniedby
cephal-gias andoccasionallymigraineandparaesthesiaoftheleftarm.
Conservativetreatmentremainedunsuccessful.Besides,she
pre-sentedahistoryofacaraccidentwithcervicaldistortion3years
before,agynaecologicalroutineintervention30yearsagoanda
motorcycleaccidentwithmildtraumaticbraininjury34yearsago.
Clinicalexaminationrevealedacervicalsyndromewithout
neu-rologicaldeficits.AnMRIofthecervicalspineshowedadvanced
degenerative discdiseaseat C4/5 and C5/6 levels, aswell as a
cervicalkyphosis,osteochondrosis,ventralspondylosisdeformans
andadischerniationatC4/5withnarrowingofthespinalcanal
http://dx.doi.org/10.1016/j.neuchi.2014.03.002
198 C.Yetimogluetal./Neurochirurgie60(2014)197–200
Table1
LiteraturereviewofarticlesreportingspinalinfectionofEikinellacorrodens.
RevuedelalittératuresurdesarticlesrapportantuneinfectionspinaleàEikinellacorrodens.
Nameofstudy Typeofstudy Location Spontaneous Postoperative Antibiotics Surgicalrevision
Angetal.,2002[1] Casereportetreview L4-L5 No Yes Yes Yes
Bridgemanetal.,1990[2] Casereport Lumbar Yes No Yes No
Emmettetal.,2000[3] Casereport T10-T11 Yes No Unknown Unknown
Lehmanetal.,2000[4] Casereport C5-C6C6-C7 Yes No Yes Yes
Noordeenetal.,1992[5] Casereport Lumbar Yes No Yes No
Peereboometal.,1987[6] Casereport Cervical No Yes(transoral) Yes Yes
Raabetal.,1993[7] Casereport L3 Yes No Yes No
Sayanaetal.,2003[8] Casereport L4-L5 Yes No Yes No
Tsaietal.,2009[9] Casereport L4-L5 Yes No Yes Yes
Zeitfangetal.2002[10] Casereport L3-L4 Yes No Yes Yes
withasagittaldiameterof8mm.Similarchangeswereobserved
atC5/6withconsecutivespinalstenosiswithasagittaldiameterof
10mm.
In ordertodecompressthesymptomatic spinalcanal
steno-sis,ananteriordiscectomyC4/5and C5/6withinterbodyfusion
withatricorticalautogenousiliaccrestgraftandanteriorplating
was recommended. This procedure was conducted under
rou-tineantibioprophylaxis(cefamandole2gintravenous)withoutany
intraoperativeor postoperativecomplications.The cervical
syn-dromeregressedsatisfactorily.
One month aftertheoperation, at theroutinepostoperative
assessment,thepatientpresentedwithlowbackpainwithout
neu-rologicaldeficitsandwithoutrelevantpathologiesonlumbarMRI.
Inaddition,CT-myelographywasperformedandneural
compres-sionwasdefinitivelyruledout.Lumbarfacetjointsyndromewas
diagnosedandtreatedwithcorticosteroidinfiltrations.
Twoyearsandfivemonthsafterthecervicalintervention,the
patientwasadmittedatouremergencydepartmentforrespiratory
distress,inspiratorystridor,dysphagiaandexacerbatedright-sided
cervicobrachialpain.Thepatientcomplainedofsuffering,overthe
pasttwodays,fromaslightprogressivedysphagiasincethe
cervi-caloperation.Duringa 6-monthperiodthepatientexperienced
anocturnal cervical pain (ataround 4a.m). Laboratoryanalysis
revealedincreasedinflammatoryparameters(C-reactiveprotein
(CRP)150mg/L,leucocytes12.6G/L).Twobloodcultures
submit-tedforsamplingwerenegative.Fiberopticevaluationofthelarynx
didnotshowanytypicalstigmataoflaryngitis.ACTscanindicated
aquestionablethickeningofthesofttissueoverthespondylodesis.
Anempiricintravenoustherapywithclavulanicacidand
amox-icillin(2.2gthreetimesaday)wasstartedwiththedifferential
diagnosis of beginning bacterial laryngitis versus viral
laryngi-tisorquestionablecervicalforeignbodyassociatedinfection.An
MRI wasable to excludean abscess and revealed a moderate
enhancementofthevertebraeC3-C6withrestrictedoverall
inter-pretationofthisareaduetothemetallicplate.Clinically,thepatient
improvedquickly;theCRPdecreasedto41mg/Lwithin4 days,
andco-amoxicillinwasswitchedtooralformula(625mgt.i.d.)and
discontinued10daysafteradmission(CRP19mg/L).
The patient was re-admitted and re-assessed 3 weeks after
discontinuationoftheempiricantibiotictherapybecauseof
pro-gressivepainduringswallowing.TheMRIatthattimeshoweda
reductionofthethickenedsofttissueoverthespondylodesisand
a newintervertebralenhancementbetweenC3and C6
suggest-ingspondylodiscitis(Fig.1AandB).Bloodculturessubmittedfor
samplingwerenegative.Arevisionoperationwithintraoperative
samplingwassuggested.Intraoperatively,thesofttissue
thicken-ingturnedouttobepus.Thoroughdebridementwithremovalof
theventralplate,aC3/4discectomywithtitaniumcage-augmented
fusionandfreshventralplateosteosynthesiswasconducted.
Sam-plesformicrobiologicalanalysiswerecollected(1swabofthepus
forcultureandforeubacterialpolymerasechainreaction(PCR)and
1intervertebralbiopsyC3/4).Empiricintravenousantibiotic
ther-apywithamoxicillinandclavulanicacid(2.2gt.i.d.)wasstarted
againuntildefinitivemicrobiologicalresultswereavailableafter
Fig.1. A–D.MRIexaminationtwoyearsafterspondylodesisC4-C6.T2weightedsequencesinthesagittalplane(1A)showsignalintensitiesintheinterdiscalspaceC3/C4 with(1B)contrastenhancementinT1weightedsequenceswithgadolinium.T2weightedsequencesinthesagittalplane(1C)showsignalintensitiesprevertebralatthe hightofC4with(1D)contrastenhancementinT1weightedsequenceswithgadolinium,suggestinghighlyspondylodiscitiswithaprevertebralabscess.
ExamenparIRMdeuxansaprèsspondylodèseC4-C6.EnséquenceT2sagittale(1A)hypersignalenregarddel’espaceinterdiscalC3/C4avec(1B)prisedecontrasteenséquence T1avecgadolinium.EnséquenceT2sagittale(1C)hypersignalpré-vertébralenregarddeC4avec(1D)prisedecontrasteenséquenceT1avecgadolinium,suggérantfortementune spondylodisciteavecabcèspré-vertébral.
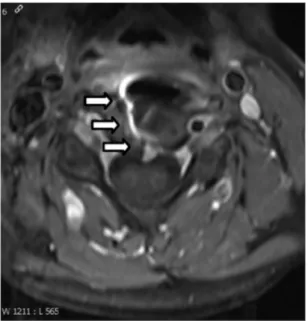
Fig.2. T1weightedMRIsequenceswithgadoliniumintheaxialplanshow prever-tebralcontrastenhancementatthelevelofinterdiscalspaceC3/4.
IRMséquenceT1axialavecgadoliniumdémontrantuneprisedecontrasteprès-vertébral auniveaudel’espaceinterdiscalC3/C4.
11days.E.corrodenswasidentifiedinbothmicrobiologicalcultures
andbyPCR.Theantibiotictherapywasswitchedtointravenous
ceftriaxonein an outpatient setting. A transthoracal
echocardi-ography(TTE)wasconductedbutdidnotrevealanyvegetation
or valvedysfunction. Accordingto theDuke’s modified criteria
(potentialarterialembolusas1positiveminorcriterion)an
endo-carditiswasunlikely[11].Duetothepatients’intolerancetodaily
injection,ceftriaxonewasreplacedafter6daysbyciprofloxacin
orally(750mgb.i.d.),afteratotalof18dayswithbetalactamine
antibiotics. Ciprofloxacin had to be discontinued 28 days later
becauseofabilateralAchillestendonitis,acommonsideeffectof
fluoroquinolones.Atthattimethenocturnalcervicalpainand
dys-phagiahaddeclinedcompletelyandinflammatoryparametershad
normalized.MRI imagesshowed marginalprevertebralcontrast
enhancement,clearregressionofprevertebralsofttissueswelling,
withoutsignsofanabscess(Fig.2).Fourweeksafter
discontinu-ationofantibiotictherapy,MRIfindingsremainedstable(Fig.3.).
Signsandsymptomsofaninfectionremainedabsentatthelast
follow-up6monthsafterdiscontinuationofantibiotictherapy.
3. Discussion
SpinalinfectionduetoE.corrodensisrare.Inthemajorityofthe
casesthisinfectionoccursinthelumbarspinewithoutprevious
surgery.E.corrodensisafastidious,slow-growing,facultative
gram-negativerod.Thepathogenprimarilyspreadhaematogenously.The
entrysiteisclassicallyapostulatedminormucosallesionlocatedin
theorobuccalregion.Intransoralsurgerythegermcanalsospread
bycontinuity.Theaetiologyoftheinfectioninourcaseremains
speculative.Insummary,latesurgicalsiteinfectionsare
statisti-callymostlycausedbyhaematogenousspreading.Haematogenous
spreadingcanbeduetotransientorpersistentbacteremia.The
lat-tersituationisseeninendovascularinfectionsi.e.inendocarditis.
Accordingtothesymptoms,theinoculationofthepathogencould
haveoccurredintraoperatively(dysphagiasincetheoperationand
nocturnalpain).Accordingtothedetectedgerm,haematogenous
aetiologyispossibleasE.corrodensisnotaskingermandtheoral
mucosawasoutsidetheoperativesite.
Ruling out endovascular affection in cases of Eikenella
bacteraemia remains essential, as Eikenella is a HACEK
organ-ism (Haemophilus parainfluenzae, Aggregatibacter aphrophilus,
Aggregatibacteractinomycetemcomitans,Cardiobacteriumhominis,
E.corrodens and Kingella kingae), a set of slow-growing
gram-negativebacteriathatformanormalpartofthehumanfloraand
canbeassociatedwithendocarditis.HACEKorganismsareknown
tocausefalseculture-negativeendocarditis,especiallyifinoculated
lessthanoneweekorifinoculatedinnon-enrichedculturemedia.
Modernculturemediaandautomatedbloodculturesystemskeep
therateoffalsenegativeresultsratherlow[12,13].
Becauseofprogressivelocalsymptoms(nocturnalpain
suggest-ingastatusofinflammation)foratleastahalfayear,lackoffever
andotherclinicalstigmataofendocarditis,andbecauseofseveral
negativebloodculturesanacuteendovascularinfectionwasnot
likely(lowpretestprobability),accordingtothemodifiedDuke’s
criteriaproposedbyLietal.[11].Inthesettingoflowprobabilitya
TTEistherecommendeddiagnostictoolofchoice[11].
TheidentificationofE.corrodenscanbedifficultduetoitsoften
minimalintricategrowthinculture.Thismaybeoneofthe
rea-sonswhyEikenella israrelyidentified orassociated withspinal
infections.TheeubacterialPCRmethodrepresentsasupplementary
diagnostictoolincasesoffastidiousgrowthbacteria,particularly
ifthediagnosticsamplingisperformedunderempiricantibiotic
therapy[14,15].
Thetherapyofchoiceisrigorousdebridementandantibiotic
treatment.Duetothelackofdata,thereisnorecommendationfor
implantassociatedinfectionsbytheHACEKgroup.Inendovascular
Fig.3. A–C.InMRIexamination4weeksafterdiscontinuationofantibiotictherapynomoresignsofdiscitisorprevertebralabscessinT2sequences(3A)orT1sequences withgadolinium(3Band3C)aredetectablein.
Quatresemainesaprèsl’arrêtdesantibiotiquesl’examenparMRTnemontreplusdesignesdedisciteoud’unabcèsprès-vertébralenséquenceT2(3A),niprisedecontrasteen séquenceT1avecgadolinium(3Bet3C).
200 C.Yetimogluetal./Neurochirurgie60(2014)197–200
infections,accordingtotheUSguidelines[16],thetherapyofchoice
isceftriaxoneoralternativelyafluoroquinolone.European
guide-linesfortreatmentofendocarditis[17]recommendceftriaxoneor
thecombinationofampicillin(ifsensitive)andgentamycin,or,after
consultinganinfectiousdiseasespecialist,alternativelya
fluoro-quinolone.Inendocarditiswithanativevalve,atreatmentduration
of4weeksisnecessary.Regardinggram-negativebacteria,most
experienceinimplantassociatedinfectionshasbeenmadewith
enterobacteriaceae and therefore (in prosthetic joint infections
[18])anintravenousbetalactamineaccordingtotheinvitro
sus-ceptibilitiesoralternativelyciprofloxacin(750mgbidbyoralroute)
isrecommended.Incasesofreimplantationofforeignmaterialat
thetimeofdebridement,aprolongedtimeofantibiotictreatment
mightbewarranted.Ouroriginalintentionwasatreatmentof8to
12weeksafterreimplantationofforeignmaterialandpostulated
chronicspondylitis.Toourknowledgetherearenosystematicdata
toconfirmthisapproach.Ourpatientwasfreeoflocalandsystemic
symptomsafterextensivedebridementandanoveralltreatment
duringsixandahalfweekswithsystemicantibiotictherapy.This
stressestheimportanceofthoroughdebridement.
Disclosureofinterest
Theauthorsdeclarethattheyhavenoconflictsofinterest
con-cerningthisarticle.
References
[1]AngBS,NganCC.EikenellacorrodensDiscitisafterspinalsurgery:casereport andliteraturereview.JInfect2002;45(4):272–4.
[2]Bridgeman SA, Espley A, McCallum ME, Harper I. Eikenella corrodens osteomyelitisofthespine.JRCollSurgEdinb1990;35(4):263–5.
[3]EmmettL,AllmanKC.Eikenellacorrodensvertebralosteomyelitis.ClinNuclMed 2000;25(12):1059–60.
[4]LehmanCR, Deckey JE, Hu SS. Eikenella corrodens vertebral osteomyeli-tissecondary todirect inoculation: acasereport. Spine (Phila Pa1976) 2000;25(9):1185–7.
[5]NoordeenMH,GodfreyLW.Casereportofanunusualcauseoflowback pain.IntervertebraldiskitiscausedbyEikenellacorrodens.ClinOrthopRelatRes 1992;(280):175–8.
[6]PeereboomD, PoretzDM.Eikenella corrodens cervical osteomyelitis:case report.VaMed1987;114(3):150–3.
[7]RaabMG,LutzRA,StaufferES.Eikenellacorrodensvertebralosteomyelitis.A casereportandliteraturereview.ClinOrthopRelatRes1993;(293):144–7.
[8]SayanaMK,ChackoAJ,McGivneyRC.Unusualcauseofinfectivediscitisinan adolescent.PostgradMedJ2003;79(930):237–8.
[9]TsaiJ,HuangTJ,HuangCC,LiYY,HsuRW.Eikenellacorrodensdiscitisina habit-ualbetelquidchewer:acasereport.Spine(PhilaPa1976)2009;34(9):E333–6.
[10]ZeifangF,Haag M,Lill CA,SaboD.Eikenella corrodens-induced spondyli-tis. Detection with 16s-RNA polymerase chain reaction. Orthopade 2002;(6):591–3.
[11]Li,etal.ProposedmodificationstotheDukecriteriaforthediagnosisofinfective endocarditis.ClinInfectDis2000;30(4):633–8.
[12]BaronEJ,ScottJD,TompkinsLS.Prolongedincubationandextensive subcul-turingdonotincreaserecoveryofclinicallysignificantmicroorganismsfrom standardautomatedbloodcultures.ClinInfectDis2005;41:1677–80.
[13]CathyA,Petti,HasanS,Bhally,MelvinP,Weinstein,etal.Utilityofextended bloodcultureincubation forisolationofHaemophilus, Actinobacillus, Car-diobacteriumEikenella,andKingellaorganisms:aretrospectivemulticenter evaluation.JClinMicrobiol2006;44(1):257.
[14]FuurstedK,ArpiM,LindbladBE,PedersenLN.Broad-rangePCRasa supple-menttoculturefordetectionofbacterialpathogensinpatientswithaclinically diagnosedspinalinfection.ScandJInfectDis2008;40(10):772–7.
[15]KupilaL,Rantakokko-JalavaK,JalavaJ,NikkariS,PeltonenR,MeurmanO,etal. Aetiologicaldiagnosisofbrainabscessesandspinalinfections:applicationof broadrangebacterialpolymerasechainreactionanalysis.JNeurolNeurosurg Psychiatry2003;74(6):728–33.
[16]BaddourLM,etal.Infectiveendocarditis:diagnosis,antimicrobialtherapy,and managementofcomplications.Circulation2005;111:e394–434.
[17]Habib G, et al. Guidelines on the prevention, diagnosis, and treat-mentof infectiveendocarditis (newversion 2009).EurHeartJ2009;30: 2369–413.
[18]DouglasR, Osmon,Elie F, Berbari,Anthony R, Berendt,et al. Diagnosis andmanagementofprostheticjointinfection:clinicalpracticeguidelines bytheInfectiousDiseasesSocietyofAmerica.ClinInfectDis2009;56(1): e1–25.