Digitized
by
the
Internet
Archive
in
2011
with
funding
from
Boston
Library
Consortium
IVIember
Libraries
HB31
.M415
Massachusetts
Institute
of
Technology
Department
of
Economics
Working
Paper
Series
Civil
Rights,
the
War
on
Poverty,
and
Blaci<-White
Convergence
in
Infant
Mortality
in
the
Rural
South
and
Mississippi
Douglas
Almond
Kenneth
Y.
Chay
Michael
Greenstone
Working
Paper
07-04
December
31,
2006
Room
E52-251
50
Memorial
Drive
Cambridge,
MA
021
42
This
paper
can be
downloaded
without
charge
from
the
Social
Science
Research
Network Paper
Collection
athttp://ssrn.conn/abstract=961 021
MASSACHUSETTS
;Ni^ .OFTECriNOa)C
'-FEB
t 52007
jLIBRARIES
Civil
Rights,
the
War
on
Poverty,
and
Black-White
Convergence
inInfant
Mortality
inthe
Rural South
and
Mississippi*
Douglas
Almond,
Kenneth
Y.
Chay, and Michael
Greenstone
December
2006
*
We
thankGary
Becker,David
Card, JohnDiNardo, Michael
Grossman,
Jon Gruber, LarsHanen,
James
Heckman,
Ted
Joyce, Allen Lapey, Ellen Meara,Kevin
Murphy,
Derek
Neal,Doug
Staiger, JillQuadagno, and
seminar participants at Berkeley, Chicago, Harvard,MIT,
and
theNBER
Summer
InstituteChildStudies
Workshop
forhelpfulcomments.
We
areespecially indebtedtoDick Johnson and
Harold
Armstrong
of the Mississippi StateDepartment
of Health, JoanExhne
of the University of Southern Mississippi, SarahHaldeman
of theLyndon
B.Johnson
Library,and
Gary
Kennedy
oftheBureau
ofEconomic
Analysis for their invaluable assistance withsome
ofthe data used in this study.Chuan
Goh,
ElizabethGreenwood,
Heather Royer, Stacy Sneeringer,and
PaulTorelliprovided excellentCivil Rights, the
War
on
Poverty,and
Black-White
Convergence
inInfantMortalityinthe
Rural South
and
MississippiAbstract
For
the last sixty years, African-Americanshave
been
75%
more
likely todie during infancy as whites.From
themid-1960s
to the early 1970s, however, thisracialgap narrowed
substantially.We
argue thatthe ehmination of widespreadracialsegregation in Southern hospitals duringthisperiodplayed a causal
role in this
improvement.
Our
analysis indicates that TitleVI
of the 1964 Civil Rights Act,which
mandated
desegregation in institutions receiving federal funds, enabled 5,000 to 7,000 additional blackinfants to survive infancy
from 1965-1975 and
atleast25,000 infantsfrom
1965-2002.We
estimatethatby
themselves theseinfantmortahtybenefitsgenerateda welfare gain ofmore
than$7 billion(2005$) for1965-1975 and
more
than$27
billion for 1965-2002.These
findings indicate that the benefits ofthe1960s Civil Rights legislation extended
beyond
the labormarker and were
substantially larger thanrecognizedpreviously.
Douglas
Almond
Department
ofEconomics and
SIPA
Columbia
UniversityInternationalAffairsBuilding,
MC
3308
420
West
118thStreetNew
York,NY
10027
and
NBER
da2
152@columbia.edu
Michael
GreenstoneMIT
Department
ofEconomics
50Memorial
Drive,E52-391B
Cambridge,
MA
02142
and
NBER
mgreenst@mit. edu
Kenneth
Y.Chay
Department
ofEconomics
UniversityofCalifornia,Berkeley
549
Evans
HallBerkeley,
CA
94720
and
NBER
I.Introduction
In 1965,
40
AfricanAmerican
infants diedforevery 1,000bom
inthe U.S.-
aratecomparable
tocurrentlevels inIndia orIran.
Over
thenextten years, theinfant mortalityrateamong
U.S. blacks fellto24
perthousand.Among
black infantsbom
in1975, roughly 7,000more
babiessurvivedtoage 1 thanifthe pre-1
965
trendhad
continued. Further, the gapbetween
blackand
white infantmortalityrates(IMR)
narrowed
substantially duringthelate 1960sand
early 1970s (Figure la). Indeed, these years comprisethe soleperiodoflargereductionsintheblack-whiteinfantmortalitygapsince
World
War
II.'In this paper
we
establish thatmuch
of the 1965-75improvement
in black infant healthwas
driven
by
a sharp decline in post-neonatal mortality rates(PNMR)
in the rural South.^ Figure lb, forexample,
shows
thenumber
ofpost-neonatal deathsamong
blackand
white infants due to diarrhea andpneumonia
inthe stateofMississippi. In the early 1960s, post-neonatal death ratesfor thesetwo
causeswere
6-7 times higheramong
blacks than whitesand
showed
no
trend toward relative improvement.Starting in 1966, however, the
number
ofdeathsdue
to these causesplummeted
among
black infants,while the
number
for whitesremained
nearly constant. This dramatic trend breakin fatalities forthesetwo
causes is important because they contributed to a high fraction ofoverall black infant mortahtyand
effectivetreatmentsforbothconditions
were
wellknown
and
widelyused.We
arguethatthetrendbreakinblackIMRs
in themral
Southwas
drivenby
federallymandated
desegregationefforts thatincreasedaccess tohospital care forblackinfants.
Of
theevents thatledtothemandated
desegregation,two
stand out as central.The
passage ofTitleVI
ofthe CivilRightsAct
inJuly1964
prohibited discriminationand
segregation in any institution receiving federal funds. Second,hospital eligibilityfor
payments
underthenew
Medicare
program
-
begun
July 1,1966
-
was
conditionedon
eliminationofthe racially discriminatory practicesthatwere
common
atthe time. Together,the CivilRights
Act and
the financial leverage exercisedby
theJohnson
administration led to the opening ofpreviously "white-only"hospitalstoblacks
and
theend ofexplicit racial segregationinhealthcare.'
The
National CenterforHealth Statisticsswitchedfromcoding racebased onthe infant's race to therace ofthe
motherin 1990. Consequently, itisimpossibletoextendtheseseriesbeyond 1990inaconsistentmanner.
"Conventionally, infant mortalityis definedas the deathrateofinfantswithintheirfirstyear oflife. Post-neonatal
mortalityisthedeathrate intheperiodfrom 28daysto 1 yearafter birth. Neonataldeaths are thosethatoccurinthe first28daysafter birth.
We
implement
a battery oftests to evaluate thehypothesis thathospital desegregationcausedthelarge reductions intheblack-white
IMR
gap.The
results ofthese tests are strongly supportive. First,thereduction in the black-white
IMR
gapbegan
immediately after integrationand
was
largest in the ruralSouth
where
blacks' access to hospitalswas
themost
constrained. Second, within the rural South, thedecline
was
concentratedamong
post-neonatal deaths,which were
more
preventable than neonatalfatalities at the time.
Roughly
two-thirds ofthe decline in relativePNMRs
was due
to a reduction inpneumonia
andgastroenteritisdeaths,two
causespreventableby
hospitaltreatment.The
most
demanding
testcomes from
a case study of Mississippi. Despite strong financialincentivesprovided
by
Medicare,many
hospitalsin Mississippiwere slow
to integrate.We
evaluate theimpact ofthose delaysusingan event-study approachthat is based
on
detailed,hospital-leveldataon
thetiming ofhospital compliance with Title VI.
We
findimmediate
and
large reductions in post-neonatalmortality, especially
among
conditionsmost
treatable in hospitals,when
a hospital in the county ofresidence
was
certified as desegregated.These
gainswere
not sharedby
white infants,and
they arerobusttoadjustmentforvarious alternativehealth determinants,such asmaternalcharacteristics(e.g.,age
and
marital status), transferpayments
(includingFood
Stamps),Medicaid
participation,and
per-capitaincome. Further, the
same
approach findsanimmediate
and
sharp increase inthe fraction of blackbirthsinhospitals,
which
corroborates thevalidity ofthe federal governments' claims ofsuccessful integration.Thus,the evidence appears inconsistent withalternative explanations, including an innovationinmedical technologyor a
change
blackinfants'home
environments.Overall, our analysis indicates that this federally
mandated
desegregation of hospitals enabledover 5,000 black infants to survive until age 1
between
1965and
1975 in the rural Southand
25,000 through 2002.We
estimate thatthe infant mortality benefits alonewere
equivalent to a welfare gainof$7.2 to $11.1 billion (2005$) for blacks
bom
in the rural Southfrom
1965-1975.For
the1965-2002
period,
we
estimate gainsbetween
$27.5and
$41.9 billion.These
findings indicate that the benefits ofthe 1960s Civil Rights legislation extended
beyond
the labormarket outcomes
considered previously(Chay
1995;Chay
1998;Donohue
andHeckman
1991;Heckman
and Payner
1989). Consequently,we
The
paper proceeds as follows. Section II provides a brief history ofthe federallymandated
desegregation of hospitals. Section III uses state
by
urban/rural data to test the hypothesis that themandated
desegregation accounts fora substantial fractionoftheimprovement
intheblack-whiteIMR
inthe decade after 1965. Section
IV
reportson
the Mississippi event studyand
its results. SectionV
interpretstheresults,
and
SectionVI
concludes.II.
The
FederallyMandated
Desegregation
ofHospitalsA. Segregation
and
Scarcity:Blacks'AccesstoHospitalsPriorto1965
Hospitals
and
other health facilities,which
shouldbethe institutionsofhealing,oftenbecause ofdiscrimination
become
themeans
ofshorteninglife.(RobertNash,DirectorofOfficeof Equal Health Opportunity, 1966)
The
Southwas
a deeply segregated society throughout the 1950s and early 1960s. Thisseparation ofracesextended to all areas oflife, including the provision ofhealth services.
A
Journalof
theNational
Medical
Association survey of 523 hospitals administeredin1955-1956
foundthatwhile 87 percent ofhospitals intheNorth
had
a "policy ofintegration", only 1 percent ofhospitals in the Southhad
one. Further,a 1956 survey of2400
Southernhospitaladministrators foundthatonly 17 percentwere
wiUing
to accept desegregation, with 62 percent adamantly opposed, 10 percent favoring separatehospitals,
and
11 percent unwilling to respond(Seham
1964).These
policies continued into the early1960s.
A
1963 survey found that 85 percent of southern hospitals reported"some
type of racialsegregation or exclusion,"
compared
to less than 2 percent in northernand
western states (U.S.Commission
on
Civil Rights 1963:141).The
pattern ofdiscrimination usually "consisted ofa separatewing
or floor forNegro
patients"insingle-building hospitals (U.S.Commission
on
CivilRights 1966:10).A
relatively unrecognized^ aspect of hospital segregationand
exclusion in the Southwas
thefederal government's role in supporting itboth legally and financially through the Hospital Survey
and
Construction
Act
of1946, alsoknown
as theHill-BurtonAct.Two
decades afteritsenactment, 350,000hospitalbeds (orapproximately halfofthe existing beds inthe
US)
had
been
constructed undertheHill-Burton
program.''As
Hill-Burton fundingwas more
generousinpoorerareas(DHEW
1966), the federalgovernment
was
thedominant
force in the postwar hospital construction in the South.The
1946^Reynolds
(1997) and Smith(1999,2005) are notable exceptions.
"
Almond
legislation that enactedHill-Burtonexplicitlyinvokedthe principleof"separatebut equal" with regardto race. Thisclause
remained
despite thefact that otherparts ofthe legislationwere
amended
and
extendedseveral times both before
and
after the 1954Brown
vs.Board
of Education
decision that "separate butequal"
was
unconstitutional.^'^Moreover,
the Hill-Burtonprogram
funded health care facilities thatspecifically excluded individuals
on
the basis of race.'The
Hill-BurtonAct
was
the only federallegislation to codify racial segregation
and
exclusion since the 19th century (Smith 1999).As
Seham
noted in the
New
England
Journalof Medicine
in 1964,"To
20,000,000 citizens, discriminationand
segregationfollowed"
from
theseparate -but-equal clauseoftheHill-BurtonAct.Table 1 presents evidence that black hospital patients in the rural South
were
tremendouslyunderservedrelative towhites throughthe early 1960s. Panel
A
ofTable 1 reports the fraction of blackinfants
bom
in hospitals with doctors present for1955-1965 by
region.*''While
black hospitalizationrates forlabor
and
delivery approachedthose of whites inthe urban areas oftheNorthand "Elsewhere"
(largelythe
Midwest
and
West),largegapsexisted intheSouth.For
residentsoftheRuralSouth,40%
ofblack babies
bom
were
not bora in a hospital with a doctor present, while thecomparable
figure forwhites
was
only4%.
The
racial disparitywas
still larger in Mississippi;more
than halfof black infants'
After the
Brown
decision, Hill-Burton program administrators repeatedly requested that the program ceasefollowingthe"separate but equal"doctrine. For example, aFebruary 1963
memo
fromtheGeneral Counsel attheDepartmentofHealth, Education, and Welfareto theAssistant Surgeon General states, "Theacceptanceofinternal
segregation atinstitutionswhichadmit bothraces isalso,Ibelieve,inaccordwiththeintent of Congressatthetime
when
thelegislationwas enacted,and in this respect alsoCongresshasmade
nochangetothelaw"(DHEW
memo
February 12, 1963:1). This
memo
goesonto arguethatHill-Burton"administrative officers"have nochoicebuttocontinue to award grants to segregated health care facilities "despite any doubts they individually
may
entertainregardingthe constitutionalvalidityofthestatutes" (ibid).
^
As
lateas August, 1963, theU.S Senaterejected aproposalthatwould haverequired grantsunderthe Hill-BurtonActtohospitalsthatdidnot discriminateonthebasisofrace (U.S.Court ofAppeals FourthCircuit1963:23)
'a hospital constructed withHill-Burton
money
could exclude a race outright ifithad indicatedin its applicadonthat "certain persons in this areawill be denied admission to the proposed facilides as padents because ofrace,
creed, orcolor" and reportedto theSurgeon General thatotherfacilities fortheexcluded racewereavailable (U.S.
Court ofAppeals Fourth Circuit 1963:7).
A
total of89 hospital construction projects in 14 stateswere approvedwiththestipulation thatonlyoneracewouldbe admittedtothefacility(U.S.Commission onCivilRights
1963:130-131). Ninetypercentofthefundsforthese discriminatingfacilitieswentto all-whitefacilities.
*Thisistheonlymeasureofhospitalaccess availablefromthevitalstatisticsdata.
'
We
define the "Rust Belt" states as Illinois, Michigan,New
York, Ohio, and Pennsylvania. The South iscomprised of 17 states (including Washington DC), as assigned by the
US
Census Bureau.We
refer tonon-metropolitan and metropolitan counties as the "rural" and "urban" areas ofa state. With the exception of
New
England, counties are classified as "metropolitan" if they are included in a Census Bureau-defined Standard
Metropolitan Statistical Area (SMSA). Race was coded aswhite and non-white inthe Vital Statistics data in this
period. In 1968, the non-white categorywas subdivided and
we
found thatblacksaccountedfor99%
ofnonwhiteinfant deaths intheUrban Rustbelt,Urban South,Rural South, and Mississippi. Thecomparable figure forUrban
Elsewhere is 93%.
We
exclude Rural Elsewhere from the analysis because blacks only accounted for 52%i ofwere
bom
outsidehospitals,versus2%
ofwhites.Panel
B
uses dataon
thenumber
of hospital beds available for whiteand
"colored" patientscollected
by
the MississippiCommission
on
Hospital Care.'°The number
of hospital beds per 1,000births allocated to blacks versus whites in the early 1960s is reported." This
measure
of access tohospital careis relevantbecause certainlife-savingtreatments for infants
were
onlyavailable athospitals.More
than twice asmany
hospital bedswere
available to whites as blacks in the predominantly whitecounties.
More
than five times asmany
hospital bedswere
available to whites as blacks in thepredominantly blackcountiesofMississippi.'^
Low
hospitalization ratesand
bed
ratios reflected the inferiormedical
care available toblacks
tmder
segregation.Senator
Javitsof
New
York
stated to the U.S. Senate:"Segregated
hospitalsand
segregated
wards have
resulted inover-crowded
conditionsand
substandard
facilities for
many
Negro
patients,"who
are often "relegated tobasement and
atticwards."
Javits further
noted
that:"Often
when
Negro
wards
are filled,no
additionalNegro
patients areadmitted
even
though
theremay
be
empty
beds elsewhere
inthehospital." (Javits 1962).B.
The
End
of Legalized SegregationinHealthCare
FacilitiesJim
Crow
was
a persistent feature of southern hospitals well into the 1960s.'''Below,
we
highlight three
landmark
events ofthemid-1960s
thatwere
instrumental in ending racial segregation inthe
American
healthcare system.These
events involvedallthreebranches ofgovernment
in turn: judicial,legislative, andexecutive.
'"
That such data were collected annually reflects the degree to whichracial segregation was institutionalized in
Mississippi. Through 1964, MississippiStatelawrequiredthat inhospitals"maintainedbythe Statefortreatmentof
white and coloredpatients,"hospital administrators mustprovideseparate entrances forwhitesandblacksandthat
the entrances"shall be usedbythe races onlyfor whichthey areprepared." Further, theGovernorofMississippi
was
empowered
to remove any administrator failing to comply with this law (Dept. of Health Education andWelfare
memo,
June 26, 1964:6). Mississippiwastheonlystateinthe nationthatrequired segregationinstate-runhospitals
(DHEW
memo,
January31, 1956). ''
We
have bedsdatabyrace for 1960, 1962, 1963 and 1964 andcomputetheratio to birthsoccurringinthese years.'"
The
findingofgreaterdisparities inaccess inthepredominantly blackcounties issimilartoBond's (1939) studythatdemonstratesthatblack schoolswere ofa higherqualityincountieswhere blacksformeda smaller fractionof
thepopulation.
We
thankananonymous
refereeforpointingthisout.'^ There was even evidence that Southerners' commitment to this system was growing as a reaction to the
burgeoning Civil Rights movement. Caro (2002) argues thatthe early stages ofthe Civil Rights
movement
in the1950s led to increased violence by whites against blacks and a renewed focus on preserving the system of
First, in 1963, Dr.
George
Simkins, a black dentist in Greensboro,North
Carolina, joined with black patients and other physicians in suingtwo
hospitalswhich
denied blacks admissionand
staffprivileges.
These
hospitals, although private,had
received federal Hill-Burton construction funds. InNovember
1963, the Fourth Circuit Court of Appeals decided Simkins v.Moses
H.Cone Memorial
Hospital in favor ofthe plaintiffs.
The
court declared that the section of the Hill-Burton legislationpermitting "separate-but-equal" health facilities
was
unconstitutional.''' Furthermore, the majorityopinionstated: "Racial discriminationin medicalfacilities is atleastpartlyresponsible forthe fact that in
North
Carolinathe rate ofNegro
infantmortality is twicetherate forwhites...." (U.S. Courtof Appeals
FourthCircuit 1963:14)'^In
March
1964, theSupreme
Court declinedto review theAppeals
Court decision, leaving it inplace.
The
immediate
resultofthisdecisionwas
thatnew
applications forHill-Burton fundsand
pendingprojects
were
allrequiredto be nondiscriminatory withrespectto admissions, staffprivileges,and
accessto all portions ofthe facilities (Smith 1999). Since halfofall Hill-Burton grantees
were
private,non-profits
(DHEW
February 12, 1963),thisruling's impactwas
notsimplylimitedtopublic healthfacilities.However,
this ruling did not affect segregated hospitals thathad
previously received Hill-Burtonfunding.'^ In fact,
lawmakers
cited the Simkins case as demonstrating theneed
for definitive federallegislation.
Passage ofTitle
VI
ofthe Civil RightsAct
in July 1964,which
prohibited discriminationand
segregationinanyinstitutionreceiving federal funds,
was
the secondlandmark
event.'''According
to thebipartisanU.S.
Commission
on
Civil Rights,"Seldom
has anypieceoflegislationbeen
sobroadinscope,sweeping
across departmental, geographicaland
political lines, as TitleVI
ofthe Civil Rights Act of1964"
(U.S.Commission
on
Civil Rights 1966;1).The
passage of the legislationby
itself led to asubstantial integration ofhospitals inthe South duringthe remainderof 1964 and 1965.
However,
there'*
Reynolds, 1997refers toSimkinsas "the
Brown
caseforhospitals."' This viewwas alsoexpressedbythe medical community. Forexample, see
Seham
(1964) intheNew
EnglandJournalofMedicine andNash(1968)intheAmericanJournalofPublicHealth.
'^Accordingto the 1963 survey by the
U.S. Commission onCivil Rights,
60%
of segregated healthfacilities hadreceivedHill-Burton funds: Reynolds(1997).
'^
In particular, Title VI stipulated that"Patients must be admittedto facilities without regardto their race, creed,
color, ornational origin.
Once
admitted, patientsmusthave access to allportions ofthefacility andto allserviceswithout discrimination. They
may
notbe segregated withinanyportionofthefacility,provided a different service,restricted in their enjoyment ofanyprivilege, or treated differentlybecause oftheirrace,creed, color, ornational
remained
pocketsofnoncompliance
insome
hospitals andinsome
practices (e.g.,integrationof
patientswithinwards),
even
within hospitalsthatclaimedtocomply
withTitleVI
(ibid).The
final eventwas
the inception oftheMedicare
program
in July 1966. Following directionsfrom
President Johnson, eligibility forMedicare
reimbursement required that hospitalsend
racialdiscrimination.'^
One
observerhas noted: "...Medicarepayments
to hospitalspromised
to be generous,and
thereby essential. In essence, hospitalshad
to choosebetween
affluence throughcompliance and
bankruptcy" (Smith, 2005:320).'' Further, in themonths
leadingup
to July, a "Children'sCrusade"
of750
federalemployees
under the Office of Equal Health Opportunityworked
to ensure hospitalcompliance
withTitleVI
throughon-siteinspections(Smith 1999:1 13)."°By
June30, 1966, 92percentofallhospitalbedswere
in compliance withTitleVI
(Ibid: 141). InJuly
and
throughthefallof1966, the Officeof Equal Health Opportunityworked
tosecurecomplianceinthe remaining hospitals.^' This "quiet revolution"
meant
that insouthern hospitals:"Negroes
are being admittedand
treated asanyone
else for the first time"(Nash
1968:246) Notably, Mississippi hospitalswere
among
themost
intransigenttothesechanges,which
we
exploitinthebelow
analysis.C. Gastroenteritis,
Pneumonia,
and
theBlack-WhiteMortalityGap
Prior to the
development and
diffusion of technologies benefiting prematureand
low-weightinfants duringthe 1970s
and
1980s,^^ medical carewas
most
successflil inpreventing deaths during thepost-neonatal period (1-12
months
after birth). Post-neonatal deaths tended to be caused by negative'*
In a speech to the American public the night before Medicare went into effect, Johnson said, "Medicare will
succeed-ifhospitals accepttheirresponsibilityunderthelawnottodiscriminate againstanypatientbecause ofrace"
(quotedinReynolds 1997). Alsosee
Quadagno
(1999)."
The
formerdirectorofthe Mississippi State Hospital Association,Thomas
Logue,referredtotheearlyMedicare programasa"goldmine"forMississippihospitals.^^
Robert
Nash
(Director of Office of Equal Health Opportunity,PHS)
wrote about the process of enforcingintegration ofhealth carefacilities,
"Some
people havecomparedouradministration ofTitle VIto the practicesofsome
oftheworld'soutstandingdictatorships"(Nash 1968; 251).^'
Reynolds (1997) quotes WilburCohen,
who
as the Secretary ofHEW
was aprincipal architectofthe Medicarelegislation:"There isone otherimportantcontributionofMedicareandMedicaidwhichhas not yet received public
notice-thevirtualdismantlingofsegregationofhospitals,physiciansoffices,nursinghomes, andclinicsasofJuly 1,
1966....If Medicare and Medicaid had not
made
another single contribution, this result would be sufficient toenshrineitasone ofthemostsignificantsocialreformsofthedecade[ifnot the century]."
^^
Two
key changesin the treatment of neonates during thepast40 years were the advent ofrespiratory therapy
techniquesand improvements in mechanical ventilation in the 1970s and the introduction ofsurfactant therapy in
1989. Further, most ofthe diffusion oflocal specialized neonatal intensive care units (NICUs) occurred in the 1980s.
events after birth, usually infectious diseases
and
accidents(Grossman and
Jacobowitz 1981). Forpneumonia
and
gastroenteritis infections in particular, death could be prevented with timely medicaltreatment,^^ in part a resuh ofgreater availabiUty ofantibiotics following
World
War
II (Shapiro et al,1968). Antibiotics
were
administeredintravenously, togetherwithfluids,inhospitals.Prior to
World
War
II,pneumonia and
gastroenteritis accounted for halfofpost-neonatal deathsfor blacks
and
whites alike.^''By
1965, thesetwo
causes accounted for under a third of whitepost-neonatal deathswhilestill comprising
45%
of black post-neonatal deaths.The
postwar surge in hospitalcapacity financed
by
the Hill-BurtonProgram
succeeded in reducing infant mortality, but these benefitswere
concentratedamong
whites(Almond
etal.2006b).By
1965, blackswere
fourtimesas likely to diefrom
gastroenteritisand pneumonia
in the post-neonatal period as whites. Thus, the primary factorunderlyingthe
widening
black-whiteinfantmortalitygap
after 1947
(seeFigure 1a)was
thedivergenceinblack
and
white experiences withthesetwo
eminentlytreatable afflictions.D.Implications
Thispaper's goal is to assess
whether
the federallymandated
integration ofhealth care facilitiescaused at leastpart ofthe
improvement
in black infant mortality ratesdocumented
inFigure 1a. In theabsence ofa
randomized
experiment,we
proceedby
presenting aseries ofincreasinglydemanding
tests.Specifically ifthere is a causal relationship, then the
above
historical context suggests that the datawillfailto rejectthe following hypotheses aboutthedeclineintheblack
IMR
after1965:1
.
Itshouldexceed the declineinthewhite
IMR.
2. It should disproportionately occur in the areas of the country
where
segregation and inadequate supplywere
more
pervasive.3 .
Itshould disproportionately occur
among
causes of death that aremore
responsive to accesstohospitals.
4.
Among
the causes of death that are preventable with hospital access, it should respondquicklytointegration.
The
remainder ofthepaperimplements
tests ofthesefourhypothesesand
failsto rejectthem.III.
Regional
Evidence on
theConsequences
oftheMandated
Desegregation
of Hospitals"^ With
regard to gastroenteritis,
Emery
(1976:204) writes that the mortality rate relates to "the eariiness [or]latenessofdiagnosis and admissionto hospital." Similarly forpneumonia, a 1964pediatrics textbookstates: "The outcomeisdependentuponearlydiagnosisandtheappropriatenessof[medical]treatment"(Nelson 1964:847-848).
"
Shapiroetal. (1968):Appendixtables1.2dandI.2e.There is
no
question that if thesame
carewere
available toNegroes
inMississippi
and
otherSouthernstatesasinMinnesota
andotherNorthernstates,Negro
morbidityand
mortalityratescouldbe sharplyreduced.(Max
Seham,New
EnglandJournalofMedicine: 1964)A.
Data
Surprisingly
few
studies exist of long-run trends in therelative health of black infants overtime.In addition, the existing research is based
on
highly aggregated data, both across regionsand
overtime,which
provide little informationon
theprecise locationand
timing ofinfant mortality changesby
race.Consequently, evidence on the specificfactorsunderlyingsignificantchangesinblack-whiteinfant health
outcomes
issparseand
often anecdotal.To
document
the locationand
timing of improvements,we
entered datafrom
the1955-1975
publicationsoftheVitalStatisticsoftheUnited States.
Drawn
from
standardcertificates oflive birthand
death, theycoverthe universeofbirths
and
deathsintheUnited States in eachyear.We
entered annual,race-specific (white
and
non-white) seriesfor ruraland urban areas of eachstate.Our
focus ison
infantmortality rates, the ratio ofinfant deaths within a year ofbirth to thetotal
number
oflive births in thatyear (expressed as deaths per 1,000 live births),
and
we
also distinguishbetween
deaths in the neonataland
post-neonatal periods.As
discussed in the previous section,we
focuson
the Rural South,Urban
South,
Urban
Rustbelt,Urban
Elsewhere,and
Mississippi.'^We
also obtained individual-level electronic mortality data for the years 1960-1975."^Unfortunately, analogousnatality micro-dataare available only beginningin 1968. Nevertheless,
we
canuse the 1960-75 mortalitymicrodatatogetherwith natalitydataaggregated
by
urbanand
ruralregions ofeach state. This enables us to analyze trends in mortality rates
due
topneumonia and
gastroenteritis.These
causes accountedfor39%
ofallpostneonatalfatalitiesinthe 1960-65period.B. Trends inBlack-WhiteInfantMortalityRatesby Region,
1955-1975
Figure 2 plots the difference in black and white infant mortahty rates
by
region for the years1955-1975. Clearly, large gaps ininfant mortality rates existed throughoutthecountry. In thefirsthalf
^^Almost 80 percent of
allnonwhite birthsfrom 1955-75 werein eitherthe Southor theurbancountiesoftheRust
Beltstates. The UrbanElsewherecounties accountedforanother 16 percent. Duringtheperiod, 28and26percent
ofallbirths intheruraland urbanSouth, respectively,werenonwhite;comparedto 17percentintheurbanRustBelt
and 11 percentinallotherurbancounties.
of
the period, the differencebetween
blackand
whiteinfantmortahty ratesdisplaysno
obviouspattern-remaining roughly constant in
some
regionsand
actually expandingin others.Between
1965and
1975,however, the racial gap
narrowed
in all regions.The
timing ofthis convergence is consistent with our hypothesis that federallymandated
integration ofhealth care facilitiesbegun
in themid-1960s
caused animprovement
inblackinfant mortalityrates.Examination
of the regional pattems in mortality gaps provides amore
demanding
test.Specifically,
we
expect that the decline should be greater in regionswhere
segregationand
restrictedaccess
were
pervasive. Again,these mortalityseries supportthisprediction. Forexample
among
thefourregions, the largest decline
from
1965-1975 occurred in the Rural South,where
the pre-existingdisparities in access
were
the greatest (recall Table 1). In this region, the racial gap declinedby
11.4deathsper 1,000births, closing fullyhalfoftheinitial disparity.
To
putthisnumber
in context, itmeans
that4,700
more
blackinfantsbom
in 1975 survived toage 1 than ifthe 1965 black-white differencestillheldin 1975.^^ InMississippi,
where
pre-1965 access differenceswere
especially glaring,the declinewas
16.4deaths per 1,000births."*
Finally, trends in the racial
gap
outside the South track each other well throughout the entireperiod.
These
regions also experienced anarrowing oftheracialgap
inthe 1965-75 period,albeit35%-40%
smaller than the decline in the Rural South.The
nexttwo
subsections furtherprobethe validity ofour hypothesis
by
estimating trend breakmodels
by
regionand
decomposing
the mortalityimprovement
intocategories
beheved
more
and
lessresponsive tohospital access.C. Trends inBlack- WhiteInfant MortalityRates by
Age and
Region,1955-1975
Ifthe equalization ofhospital access
between
blacksand
whites indeed caused the black-whiteinfantmortality gaptofall,
we
would
expectthisreductiontobe concentratedinthe post-neonatal period.To
evaluatethispossibility,we
fitsimpletrendbreakregressionmodels
ofthefollowing form:(1) ysn
=
af+P(/-1965)*
l(?>1965)
+
53r+
8srt,where
s,r,and
tindex state, urban/rural,and
year, respectively.The
dependentvariableis theneonatal or'
Calculatedas: #ofBlackBirths"" *(Black
IMR""-(White
IMR""-White
IMR'"')),for rural Southbirths. 'In theruralSouthandMississippi, theblack-whitegapwasincreasingfrom 1955-1965.
postneonatal mortalityrate.
The
equationis estimated separatelyforblacks, whites,and
theblack- whitedifference.
The
explanatoryvariables are atimetrend, t,and anindicatorvariableequaltooneiftheyearis after 1965 interacted witha post-1965 timetrendequal to {t
-
1965).a
measuresthe average 1955-65trend in the infant mortality rate across states. [3 is the parameter ofinterest
and
measures the averageslope
change
in theIMR
trend that occurred after 1965. All specifications include rural/urbanby
statefixed effects, 5sr,
which
account forpermanent
differences across rural/urban areas of states.The
numbers
of births in each race-rural/urban-state-year cell are used as weights in the race-specificregressions,
and
the weight is thenumber
of black births in the black-white regressions.The
standarderrors arecorrectedforheteroskedasticityandresidualtime-series correlationatthe state-level.
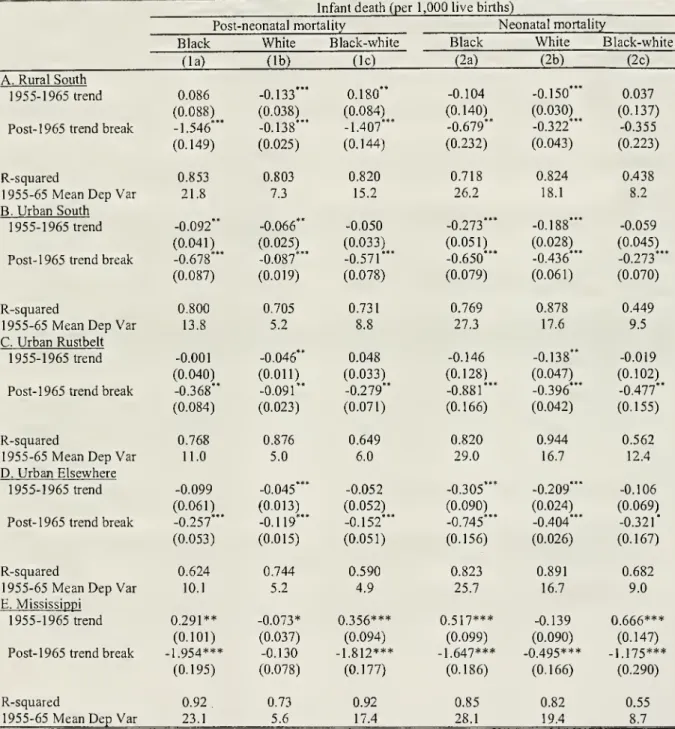
Table 2 presents the trend breakregression results forpost-neonataland neonatal mortalityrates
inthe
two
setsof columns. Within eachsetof columns, resultsforblackand
whitemortalityratesand
theblack-whitedifference are
shown,
althoughwe
focusour descriptionhere onthe difference regressionsincolumns
(Ic)and
(2c) dueto space constraints.The
panels ofthe tablecorrespond tothe fourregions inFigure2andMississippi.
The
rural Southstands outfor several reasons. First, the pre-1965
black post-neonatal mortalityrate
exceeded
the white rateby
15.2 deaths per 1,000 live births. This racial differenceexceeded
theaverage blackpost-neonatal mortality rate in each regionoutside the South. Second,the estimates
show
thatthe
gap between
black and whitepost-neonatal mortality rateswas
increasingfrom
1955 to 1965 atthe rate of0.18 deaths (per 1,000 live births) per year. Thus, conditions for blacks
were
apparentlydeterioratingrelative towhites.
Third, there
was
a largetrendbreakof about 1.4deathsper yearafter 1965. Thisimpliesthattheblack-whitemortality
gap
intherural South decreased 14deathsper 1,000 birthsmore
through 1975 thanifthe pre-1965 trend
had
prevailed. Thisimprovement
iscomparable
to the pre-existing racial gap.Moreover,
itimplies that 5,900 additional infants survivedtoyear 1 through 1975 thanwould
havebeen
expected
from
pre-1965 trends.The
racialgapinpost-neonatal mortalityratesalsonarrowed
intheother three regions.However,
theblack-white trendbreak in therural South is 2.5 times largerthan in the
Urban
South, 5 times largerthan in the
Urban
Rustbelt,and
9 times larger than in theUrban
Elsewhere.Among
these regions, themagnitude
ofthe trend break corresponds to the deficiencies in hospital access inTable 1: largest in theurban South followed
by
the urbanrustbeltand
urban elsewhere. Finally,we
notethat the largestblack-whitetrendbreakafter 1965
was
forMississippi,where
accessgapswere
greatest.After 1965,both whites
and
blacks enjoyedimprovements
inneonatal mortality, althoughblacks'gains
were
larger. Interestingly, the closing of the racial gapwas
roughly equivalent across the fourregions. Further, for blacks in
Urban
areas outside the South, the post-1965 reductions in neonatalmortalityexceededthe post-neonatal ones.^^ Forpresent purposes,
we
note thatthelargest reductions inboth mortality
and
black-white gapswere
achieved during the post-neonatal period,and
that themagnitude
ofpost-neonatalimprovements
corresponds toavailablemeasures
ofhospitalaccess.'"D. TrendsinBlack-WhiteInfant MortalityRates by
Cause ofDeath
and
Region,1960-1975
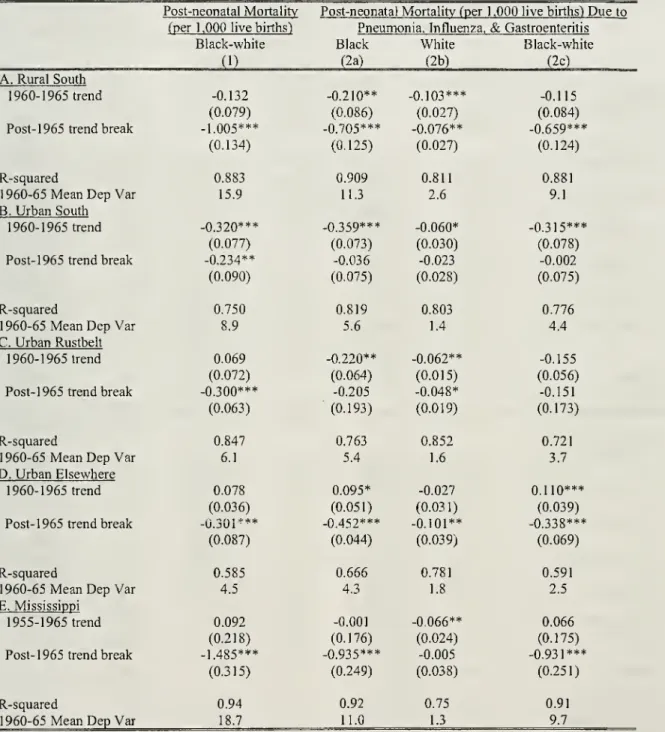
Table 3 present analogous trendbreak results for the subset ofpost-neonatal deaths caused
by
pneumonia
and gastroenteritis.As
noted,we
isolate these deaths because theywere
readilyand
necessarily treated in hospitals at the time.
Because
the data reporting cause of death are availablebeginningin I960,''
column
(1) reports trend-break estimates for allpost-neonatal deathswhen
thepre-periodis restricted to 1960-1965. This permits assessment oftheextentto
which
treatablecausesaccountforthepost-neonatal trendbreaksinTable2.
Estimates in
columns
(2a)-
(2c) indicate that largereductions inpreventable deaths occurred inthe South that
dwarfed
improvements
for whites. Moreover, the decline in deaths due to these causes accounted for roughly two-thirds ofthe entire relative decline in the post-neonatal mortahty gap.The
pattern forMississippiis similar. Thus, althoughgastroenteritis
and
pneumonia
accountedforunderhalf^'
A
comprehensiveaccounting ofneonatal mortality trends (especially inMississippi) is beyondthe scopeofthis
paper,howevertheyarelikely tobeatleastpartiallyduetotheinitiationoftheFood Stamps program
(Almond
etal.2006a) and theextension ofthe Maternal and Infant Care
Component
ofthe Maternal and Child Health ServicesProgram (Chay andGreenstone 2000; Gold,etal. 1969;Sokoletal. 1980;PeoplesandSiegel 1983;Chabot1971).
'°
Chay
and Greenstone (2000)show
that this measureofaccesswas increasingintheyears priorto 1965 for ruralsouthernblacks, but this trend acceleratedafter 1965. In regression specifications analogous to those underlying
Tables 2 and 3 for the fi-action ofbirths in hospitals, the estimated post-1965 trend break for blacks in therural
South is large and significant.
To
the extent that this measure reflects the availability ofhospital care to blackinfants after 1965, this availability improved at the time
when
post-neonatal mortality rates for Southern blacksbegan tofall. See
Chay
and Greenstone (2000)forevidenceonthe significantandpositive associationbetweenthe mortalityimprovementandtheshareofbirths in hospital."
SeeData Appendix.of post-neonatal deaths
by
the mid-1960s,^^ they accounted for nnost of the post-neonatal mortalityimprovement
for blacks. In contrast, there is little evidence ofa decline in these deaths in theUrban
South
and
Urban
Rustbelt."IV.
Event
Study Evidence
oftheImpact
of Integrationon
InfantHealth
and
HospitalAccess
A.Event Study Evidence
We
now
turn tothemost
directand
demanding
test ofthe integration hypothesis, conducted with anew
data filecompiled
for this purpose.Medicare
certification dates for the roughly 100 Mississippihospitals
were
obtainedfrom
theJournalof
theAmerican
Hospital Association annual guidesissues.We
combined
these datawithannual, race-specific county-levelvitalstatistics data forMississippi, includingthe
number
of neonataland
post-neonatal fatalitiesby
broad cause of death categories, thenumber
ofbirths ina hospital with adoctorpresent,totalbirths, the distributionofbirths
by
maternal age (under 15,15-19, 20-29, 30-34,
and
35 orolder), and the fraction of"illegitimate" births.^'' Finally,we
compiled
county-level data on federaltransferpayments, broken out by categories (e.g.
Food
Stamps) andcounty-level
income
per-capita. SeetheData
Appendix
forfurtherdetails.We
implemented
an event-study analysisofthe impacts ofthepresenceofatleastoneMedicare-certifiedhospital in acounty on infanthealth
and
hospital access usingthesedata. Specificallywe
fitthefollowingequation:
6
(2)
yc
=
ttc ?+
X
Tii 1(xc,=
i)+ Xc'P
+
ric+
U
where
c references countyand
t indexes year, x denotes the event year, and itis normalized so that foreach county x
=
1 inthe firstfull yearthatthe firsthospital within its boundaries is certified asMedicare
eligible.
Among
the 80 Mississippi counties with complete data," x=
I for 47 counties in 1967, 11 in'^For
1964-1966,gastroenteritis and pneumonia accountedfor
43%
ofallpost-neonatal deaths intherural South,and
37%
ofpost-neonatal deaths nationally.Among
blacks,thesecausesaccountedfor49%
ofpost-neonataldeathsintheruralSouth and 45%)nationally.
^^
The
entire declineinpost-neonatalfatalitiesamong
urban Elsewhereresidents,whilesubstantiallysmallerthanintheruralSouthandMississippi,isaccountedforbyfewerpreventable deaths. This findingisan interestingsubject
forfuture research.
^''
For 1959-1970,
we
obtained these vital statistics data by filing atreedom of information act request with theMississippi State Department ofHealth.
We
then extended these data through 1975 with the publicly-available NatalityandMortahty Vital Statisticsdatafiles.''
Vitalstatistics dataforBlacksinItawambaandTishomingocountieswereunavailable.
1968, 5 in 1969, and 17 in 1970.^^ Data
from
each county are restricted tothe 13 yearsrunningfrom
theseven yearsbefore acounty'sfirsthospital
was
certifiedforMedicare
throughsixyears afterward(i.e., -6<
T<
6).The
dependent variables are the post-neonatal mortality rate for all causesand
for preventable(i.e.,
pneumonia
andgastroenteritis) causesamong
countyresidents.We
also use the percentof
births inhospitals witha doctor present as a dependent variable totestfor differential changes in hospital access
by
raceasan implicit "first-stage"testofthe integration hypothesis.A
failuretofindincreasedaccessforblacks
would
undermine
the claim that greater access caused theimprovement
in infant healthdocumented
in thissubsection.Equation(2) includes atimetrendthat isallowedtovaryatthe county level(i.e., a^).
The
vectorXct includes the fraction ofmothers in the five age categories listed above, the fraction of mothers that
were
unmarried, county-level per-capita income,and
county-level per-capita transferpayments
(net ofmedical insurance payments)."
The
specification also includes fixed effects for each county (i.e., tjc).The
equation is estimated separatelyforblacks,whites,and
theblack-white differenceand
it isweighted
by
thenumber
ofblack,white,and
blackbirths,respectively, ^ctisthe stochastic errorterms. Finally, thestandarderrorsarecorrectedforheteroskedasticity
and
clusteringatthe county-level.The
parameters ofinterest are the six TCi's.They
separately test formean
shifts in county-levelpost-neonatal mortality rates(and hospital access), after adjustment forpre-existing trends andthebroad
setofcovariates, ineach ofthesixyears subsequenttothe first certificationofa hospital for
Medicare
inthe county. This event study approach provides arigorous test ofthe integration hypothesis
—
thatblackpost-neonatal fatalities
were
causedby
racial discrimination in hospitalsand
that blacks' access tohospitals
was
restricted.An
immediate
and persistent intercept shiftwould
provide strong evidence infavor ofthe integration hypothesis. If instead the infant mortality and hospitalization rates
were
notassociated with certification, took a
number
of years tobecome
evident, evaporated soon aftercertification, or
began
prior to certification, the validity of the integration hypothesiswould
be undermined.''^
See DataAppendixfor adescriptionof
how
countieswereassignedMedicarecertification dates."
Both incomeandtransferpaymentsare interpolatedin missingyears. However,datacoverageisbestduringthe
periodofcertificationfortheMedicareprogram.
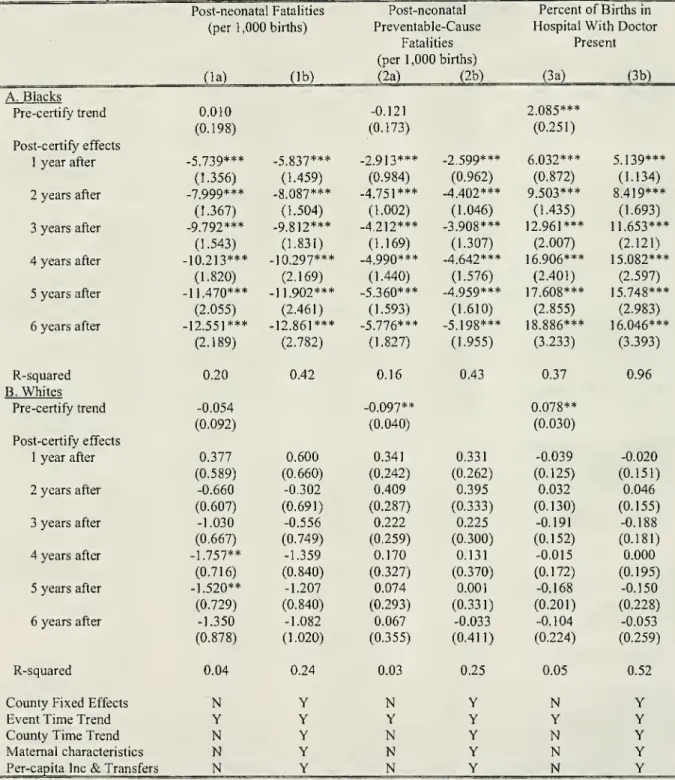
Table
4
presents the resultsfrom
fittingequation (2) forthe three dependentvariables. Itreportsresults
from
aparsimonious specificationthat includes just thetimetrendand
thesix 1(xct=
i) indicators,and
thefrillspecificationdescribedabove
(andintherow
headingsof Table4). PanelsA
and
B
give theresultsforblack
and
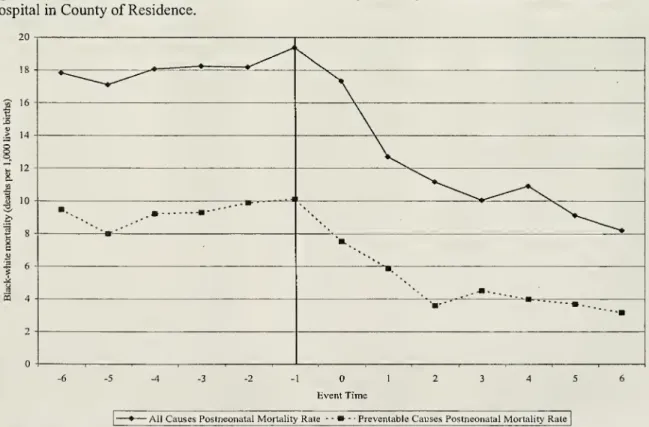
whiteinfants, respectively.Figure 3
summarizes
the post-neonatal mortality results graphically. Specifically, itis basedon
the estimationofaversionof equation(2) fortheblack-whitedifferenceinthepost-neonatal mortality for
all causes and, separately,preventablecauses.
The
specification'sonly covariates area fullset ofevent-timeindicators,
and
theirassociatedparametersareplotted.The
vertical line divides the yearsbeforeand
after
Medicare
certification.The
tableand
figure provide dramatic support for the integration hypothesis. There is littleevidence of a trend in either all cause or preventable cause post-neonatal mortality rates in the years
preceding
Medicare
certification. In the first year after certification, the black all cause post-neonatalmortahtyrate declined
by
about 6 deaths (per 1,000hve
births). This is greater than a25%
reduction intheblackpost-neonatality
mean
(for x=
0) ina single year.By
the end ofthe event-window, thedechne
is roughly 13 deaths (per 1,000 live births)
which
ismore
than a50%
decline.The
preventable causepost-neonatal mortalityrateestimatessuggestthatreductions inthesefatalitiesaccountedfor
40%)-45%
ofthe overall post-neonatal decline.
Notably, the adjustmentfor the full setofcovariateshas
no
substantiveimpacton
the estimatedcoefficients.^^ Thus, the observable relative risk characteristics of black mothers cannot explain the
column
(la) results.^' Further, the black-white differenceshown
in Figure 3 leads to nearly identicalconclusions;this
undermines
thepossibility that the introductionofa healthtechnology availabletobothraces or other secularshocksexplainthe results.
Finally,
columns
(3a)and
(3b) provide an opportunity to assess whether TitleVI
ofthe CivilRights
Act and
theMedicare
certifications achievedtheirmost
basic goalofincreasing blacks' accesstohospitals. Itistemptingto treatthe
measured
variableastheendogenous
variable inan equationforpost-'^The
additionof yearfixedeffects tothe richer specification incolumns (lb)and(2b) leadstothesamequalitative conclusions. However, thestandarderrorson theevent timeindicatorsaresubstantiallylargerduetothedifficulty
ofseparately identifying the year and event time fixed effectswith the modestvariation in Medicare certification dates.
^'
The
shareof black motherswho
wereteenagers orunmarriedincreasedinMississippiduringthelate 1950s.neonatal mortality (with certification as the instrument), but this
would
be inappropriate since thepercentageofbirths in ahospital
do
not directly affectdeaths inthepost-neonatal period, especiallythosedue to preventable causes."" Nevertheless, it is teUing that the entries
document
a largeand
preciselyestimated increase in the percentage of black births occurring in hospitals as
soon
asone
year afterMedicare
certification. Notably, therewas
a substantial pre-existingupward
trend in births in hospitalsamong
blacks.However, even
after accountingforthistrend,thepercentof blacksbom
inahospitalwas
more
than 12 percentagepoints(20percent)higherthreeyearsafter certification.B. AlternativeExplanations
For another factor to explain the post-neonatal mortality results, it
would
have
to exert animmediate
effecton
post-neonatal deaths (especiallyamong
preventable causes)and
vary acrossMississippi counties in the
same
way
as theMedicare
certification dates.These
aredemanding
criteria.Nevertheless, this subsection briefly considers alternative explanations for the paper's findings, in
particular the
major
changes in social welfareand
public healthprograms
resultingfrom
theWar
on
Poverty.
The
Medicaid
program, initiated in 1966, providedmoney
to poorer families for medical care.However,
Mississippi did not begin its participation inMedicaid
until January 1, 1970,by
which
timemost
ofthe reductions in black post-neonatal mortality in Mississippihad
already occurred. Similarly,overthis period the
AFDC
program
appears tohave
played amuch
smallerrole in Mississippi than inotherstates.'"
Moreover,
our event-studyestimates are essentiallyunchanged by
adjustment forcounty-leveltransferpayments,includingboth
AFDC
and
Food
Stamp
payments.''^Neither
do programs
that specifically targeted public health appear important for Mississippi'*"
We
attempted to obtain annual counts of infant admissions during the 1960s by race and age (along with
informationonthe principle diagnosis)fromseveralofthelargerMississippihospitals. Despiteouroffertobearthe
costof producingthese dataandredacting allpersonalidentifiers,ourrequestswererepeatedly denied.
'"
For example, caseloadsinMississippigrewatlessthan half the nationalratebetween 1965and 1970(Department
of Health and
Human
Services 1998:22). Accordingto theBEA's
governmenttransferpayments dataintheREIS
file,therewere nopayments fromthe
AFDC
programtoMississippiuntil after 1968. *'SeparateworkinprogressfindsthattheFood Stamps Program(FSP)nationalroll-outduringthelate 1960s and
early1970sdidimprovecertainperinatal outcomes(e.g. gestationlength). However, nodiscernibleeffectswere
foundforpost-neonatal mortality (whilenodistinguishablefromthezero, thepointestimateswerepositive,i.e.
FSP
associatedwithanincreasein
PNMR).
Moreover,noassociationwasfoundbetweencounty-leveladoptionofFSP
andbirths inhospital:
Almond
etal.(2006a).duringthisperiod. Real federalspending undertheMaternal
and
ChildHealth(MCH)
program
increasedonly 17 percent in Mississippi
between
1965and
1970(DHHS
2001:80),and
MCH
expenditures (perpoor
child) in Mississippiwere
less than half the national average in 1969 (Davisand
Schoen
1978:146).''^ Also, whilethe proliferationof
community
health centers duringthe 1970s hasbeen
foundto decreaseinfantmortality, especially
among
blacks, therewere
only 51 such centers inthe entirenationas of 1968
(Goldman
and
Grossman
1988). Further,community
health centers did not provide theaggressivemedical treatmentthat
would
havebeen
requiredby
infantswithpneumonia and
diarrhea.Finally, changes in birth technology
do
not coincide with the timing of the infant mortalityreductions forblacks in Mississippi (see footnote 22).
Moreover,
technological innovations are widelythought to impact early infant death resulting
from
prematureand
low
birth weight births,which
is notconsistent with the striking reduction in preventable post-neonatal infant deaths
among
blacks inMississippi.
In
summary,
we
areunabletoidentify a viablealternative explanation fortheevent studyresults.Our
conclusionfrom
the Mississippi data is that the federallymandated
integration of health carefacilities played a central role in the sharp decline in blacks' post-neonatal mortality rates.
To
put theresults in
some
context, the Table 3 estimates imply thatjust 6 years after successful integration,270
additionalblack post-neonatesperyear survivedtoage 1 inMississippi.
V. Interpretation
How
largewas
the mortality reduction causedby
mandated
integrationand
what
was
theassociated welfare gain?
Answering
these questions requires additional assumptions, but informs theimportance of the health effects here
documented and
how
theycompare
with effectsfrom
othergovernment
interventions.The
case for a causal impact ofmandated
integration is strongest in the rural South (whereex-ante access disparities
were
greatest)and
for causes of deathknown
to be treatable in hospitals.The
black-white preventable causepost-neonatal estimates in
column
(1)of Table 3 indicatea trend breakof0.66 deaths per 1,000 births lower in
1966
than predictedby
pre-existing trends, 1.32 per 1,000 births"•^
Refersto"Title
V
HealthProgramtotalsor theMCH
BlockGranttotals.'lowerin 1967,
and
soon untilitwas
6.6 deathsper 1000births lowerin 1975.The
multiplication ofthese declines in thePNMR
by
the annualnumber
of blackbirths in therural South implies that roughly 4,700 additional survived
from
age 1month
to age 1 year during theyears 1965-1975
and
25,300 infantsfrom
1965-2002.'*'' Alternatively, itmay
be reasonable toascribe theentire post-1965 trend break inpost-neonatal mortality (i.e. post-neonatal deaths
from
all causes) to themandated
integration. Inthis case,thesenumbers
would
rise to 7,100and
38,600, respectively.''^These
calculations suggest that the
mandated
integration of hospitals in the rural South accounted for16%
(based
on
preventable causes only) or25%
(basedon
all post-neonatal fatalities) ofthe national 7.5 per 1,000declineinthenationalblackPNMR
between
1965and
1975.An
alternativemeans
to assess themagnitude
ofthese gains is to askhow much
blacks in therural South
would
havebeen
willingtopay
(WTP)
forthese reductionsininfant mortality.''^To
developan estimate of
WTP, we
use Ashenfelterand
Greenstone's (2004) upperbound
estimate of $1.9 million(2005S)asthe valueofa statistical life(VSL)."*'
With
thisvalueand
a3%
discountrate,we
estimate thatblacks in the rural South in 1965
had
aWTP
for the reduction in infantmortality that occuiredbetween
1965 and 1975 of$7.3 billion (forpreventable cause post-neonatal fatalities)
and
$11.1 billion (for allcause post-neonatal mortality).
Among
all black residents ofthe rural South, theWTP
per
capitawas
$1,400and
$2,100 (for preventableand
all-causePNMR
reductions, respectively). Ifwe
keep thereduction inblackpost-neonatal deaths constantatthe 1975reduction for the
1975-2002
period, there areadditional gains of $20.1 billion (preventable causes)
and
$30.8 (allpost-neonatal causes) for the1975-^
Fortheyearsafter1975,we
holdthePNMR
reduction constantatthe 1975levelof6.6.per 1,000births.'*'
Alternativeassumptionswould causethesenumberstobeevenlarger. For example, it
may
beappropriatetousetheestimatesfromTable2thatrelyonthe 1955-65 period(ratherthan the 1960-65 periodas inTable3) toestimate the pre-1966 trend. Thetrendbreakestimates in Table 3 are largerbecause theblackpost-neonatal mortalityrate
worsened from 1955-1960, which is consistent with white resistance to the burgeoning Civil Rights
movement
(Garrow 1986 andCaro 2002). Additionally, itmight beappropriate to addthe reductioninthe black-white post-neonatal mortalityrateintheruralSouth,althoughthiseffect isn't statistically significant. Therewerealsopre-1965accessdisparities intheurban South so
some
may
considerit appropriateto addthe post-1965trendbreakin post-neonatal mortality. This argumentisundermined bythefindingofnotrendbreakinpreventable causes(seecolumn(2c)ofTable3). Our viewisthattheevidenceinfavorofattributingany
IMR
declines inother regionsisweak
duetotheabsenceof evidenceonex-ante accessdisparities,
''^
Obviously, this approach assumes the
WTP
waspositive only forblacks in the South and to the extent this isincorrect, willyieldconservative estimates.
"
Thisis atthelow end oftherangeofestimatesofthe
VSL,
butwe
thinkit is appropriateto beconservative forseveralreasonsincluding that thisestimatecomes frommorethan twodecades afterthe Civil Rights Act, blacks in
therural Southhadrelativelylowincomes,and
WTP
topreventaninfantdeathmay
belowerthanforanadultdeath(Murphyand Tope!2006).
2002
period(an additional/7ercapitagainof $3,900 and$5,900J.These
measures
ofWTP
for theimprovements
in infant mortality likely underestimate(potentially substantially) a
measure
ofWTP
for hospital integration. Integrationpresumably
reduced mortahty ratesamong
otherage groupsand
reducedmorbidities across all ages. Further, the practice ofsegregation
may
haveimposed
additional costs on hospitals thi-ough duplication ofservices.'*^On
theother side of the ledger, the
expanded
supply of health carepresumably
had
a social cost,and
a fullwelfare analysis
would
account for theseadded
costs. Itmay
also be appropriate to subtract theadministrative costsincurredinthe achievement ofintegration, althoughthey are likely to be a relatively
smallone-timecost.
VI.
Conclusions
Passage ofTitle
VI
ofthe Civil RightsAct
marked
a reversal offederal policy with respect torace. Inprohibiting discrimination
and
segregationin allinstitutionsreceiving federal funds,and
throughits vigorousenforcement
by
theJohnson
Administration, blackaccess to hospitals intherural Southwas
quickly
and
dramatically expanded, withlargebenefits interms ofinfant lives saved.We
conclude thatthe benefits of 1960s Civil Rights legislation extended
beyond
the labor marketand
therefore aresubstantially largerthanhas
been
recognizedpreviously.These
findings are relevant for current discussions regarding the efficient allocation of publicresources in developing countries.
More
than a third ofchildren inlow-income
countriesdo
not receivetreatment for acute respiratory infections and only half receive proper care for diarrhea (Jha et al.,
2002:2037). This paper illustrates that health treatments are sought out
when made
availableand
canhavelarge
and immediate
benefits."^Desegregation"requireslesspersonnel andcontributestotheefficiencyofthe hospitaliftherearenottwowaiting
rooms, two maternityunits, andtwo intensive careunits
~
oneforNegroesand one forwhites."(Nash 1968:249).Similarly,