HAL Id: hal-01832150
https://hal.archives-ouvertes.fr/hal-01832150
Submitted on 12 Jul 2018
HAL is a multi-disciplinary open access
archive for the deposit and dissemination of
sci-entific research documents, whether they are
pub-lished or not. The documents may come from
teaching and research institutions in France or
abroad, or from public or private research centers.
L’archive ouverte pluridisciplinaire HAL, est
destinée au dépôt et à la diffusion de documents
scientifiques de niveau recherche, publiés ou non,
émanant des établissements d’enseignement et de
recherche français ou étrangers, des laboratoires
publics ou privés.
Brugada syndrome: Diagnosis, risk stratification and
management
Jean-Baptiste Gourraud, Julien Barc, Aurélie Thollet, Hervé Le Marec,
Vincent Probst
To cite this version:
Jean-Baptiste Gourraud, Julien Barc, Aurélie Thollet, Hervé Le Marec, Vincent Probst.
Bru-gada syndrome: Diagnosis, risk stratification and management.
Archives of cardiovascular
dis-eases, Elsevier/French Society of Cardiology, 2017, Equipe I Equipe IIa, 110 (3), pp.188–195.
�10.1016/j.acvd.2016.09.009�. �hal-01832150�
Availableonlineat
ScienceDirect
www.sciencedirect.com
REVIEW
Brugada
syndrome:
Diagnosis,
risk
stratification
and
management
Diagnostic,
stratification
du
risque
rythmique
et
prise
en
charge
du
syndrome
de
Brugada
Jean-Baptiste
Gourraud
a,∗,
Julien
Barc
b,
Aurélie
Thollet
a,
Hervé
Le
Marec
a,
Vincent
Probst
aal’InstitutduThorax,INSERM,CNRS,UNIVNantes,CHUNantes,Nantes,France bl’InstitutduThorax,INSERM,CNRS,UNIVNantes,Nantes,France
Received25July2016;receivedinrevisedform13September2016;accepted15September 2016
Availableonline27January2017 KEYWORDS Brugadasyndrome; Prognosis; Diagnosis; Suddencardiac death; Riskstratification
Summary Brugadasyndromeisarareinheritedarrhythmiasyndromeleadingtoanincreased riskofsuddencardiacdeath,despiteastructurallynormalheart.Diagnosisisbasedonaspecific electrocardiogrampattern,observedeitherspontaneouslyorduringasodiumchannelblocker test.Amongaffectedpatients,riskstratificationremainsachallenge,despiterecentinsights fromlarge populationcohorts. Asimplantable cardiacdefibrillators — the main therapyin Brugadasyndrome—areassociatedwithahighrateofcomplicationsinthispopulation,the mainchallengeisrisk stratificationofpatients withBrugadasyndrome. Asidefromthetwo mainpredictorsofarrhythmia(symptomsandspontaneouselectrocardiogrampattern),many riskfactorshavebeenrecentlysuggestedforstratifyingriskofsuddencardiacdeathinBrugada syndrome.Wehavereviewedthesedataanddiscusscurrentguidelinesinlightofrecentprogress inthiscomplexfield.
©2017ElsevierMassonSAS.Allrightsreserved.
MOTSCLÉS Syndromede Brugada;
Résumé LesyndromedeBrugadaestunearythmiecardiaquehéréditairerare,responsable demortsubite.Enl’absencedecardiopathiestructurelle,lediagnosticreposesurl’ECGau repos oulors d’un test de provocation pharmacologique. Comme le seultraitement ayant
Abbreviations: BrS,Brugadasyndrome;ECG,electrocardiogram;EPS,electrophysiologicalstudy;ICD,implantablecardiacdefibrillator;
SCD,suddencardiacdeath;VF,ventricularfibrillation.
∗Correspondingauthorat:CHUNantesHGRL,BoulevardJMonod,44093Nantes,France.
E-mailaddress:jeanbaptiste.gourraud@chu-nantes.fr(J.-B.Gourraud).
http://dx.doi.org/10.1016/j.acvd.2016.09.009
Brugadasyndrome:Diagnosis,riskstratificationandmanagement 189 Pronostic; Diagnostic; Mortsubite; Stratificationdu risque
démontrésontefficacitéestl’implantationd’undéfibrillateur,maisqu’ils’accompagned’un risqueélevédecomplicationdanscettepopulation,l’évaluationdurisquerythmiqueest essen-tielleàlapriseenchargedecespatients.UnaspectECGspontanédesyndromedeBrugada etla présencede symptômesrestentleséléments lesplusimportantsdansla stratification durisquemaisdenombreuxautresparamètresontétérécemmentproposéspourstratifierle risquedemortsubite.Nousdiscuteronsl’analysedel’ensembledecesdonnéesauregarddes dernièresrecommandationsdepriseencharge.
©2017ElsevierMassonSAS.Tousdroitsr´eserv´es.
Background
Brugadasyndrome(BrS)isarareinheritedarrhythmia dis-easepredisposingtoventricularfibrillation(VF)andsudden cardiacdeath(SCD),withoutidentifiablestructural abnor-malities[1].BrSmainlyaffectsmiddle-agedpatients(aged
45 years at diagnosis), withan eightfold higher diagnosis
prevalence in men,despite an autosomalmode of
inheri-tance[2,3].
Diagnosisisbasedsolelyonaspecificbutlabilepattern
onanelectrocardiogram(ECG),definedasa≥0.2mV
coved-type ST-segment elevation in the right precordial leads.
However,theECGcanbesilent,requiringsodiumblockersto
unmaskthepathology.IdentificationofBrSpatientsis
cru-cialtoavoidsuddencardiacdeath(SCD),whichisoftenthe
firstsymptom[2].Amongthegeneralpopulation,the
preva-lenceofBrS appearstobeverylow,affecting 5in10,000
people[4],anditsrealimpactonSCDisuncertain. Inthe
absenceofprovenefficientdrugtherapy,implantable
car-diacdefibrillators (ICD)—themain therapyin BrS—have
beensuggestedforprimarypreventioninmanyBrSpatients.
However, the risk of SCD among asymptomatic patients
remainsrelativelylow(0.5—1.5%peryear)andtherateof
ICD-relatedcomplications is high in thisyoung population
[2,5]. Consequently,the main challenge for the physician
is the identification ofpatients at risk of arrhythmia who
requirespecifictreatment.
Thisreviewwillfocusonclinicalaspectsofthediagnosis
ofBrS,riskstratificationandimpactonmanagement.
Clinical
presentation
and
diagnosis
One-thirdofBrSpatientsareidentifiedaftersymptoms (syn-cope or aborted SCD), most of which occur at rest with vagal symptoms or during the night [2]. Syncope can be
caused by either non-sustained VFor a vasovagalepisode
withoutarelevantcharacteristictodistinguisharrhythmic
fromnon-arrhythmicaetiology[6].Fever,alcoholintakeand
medicationscanincreasearrhythmiaoccurrence;these
trig-gerscanunmaskaBrSECGpatterninasymptomaticpatients
[7,8].Theincreasedprevalenceof atrialfibrillationinBrS
canalsosuggestaneed forBrSscreeningtothephysician,
particularlyforyoungmen[9].
Figure 1. Electrocardiogram (ECG) patterns of Brugada
syn-drome.ModifiedfromRef.[27].ECGpatternsarerepresentedfrom
leftto right inright precordialleads.Only a type1 ECGallows
diagnosisofBrugadasyndrome.
Two-thirdsofBrSpatientsareasymptomaticatdiagnosis
[2,10].Ofthese,morethanone-thirdareidentifiedduring
familialscreening[2].Sincethe lastguidelineswere
pub-lished,symptomsarenotrequiredfordiagnosisthatisbased
onaspecificECGpattern[1].ThisECGpattern,previously
knownasatype1ECG,consistsofacovedST-segment
ele-vationinoneright precordialleadof>0.2mV,endingwith
anegativeTwave(Fig.1).OtherECGpatternsarenot
suf-ficientforthediagnosis[11],butcansuggesttheneedfor
asodiumchannelblockertesttothephysician,whichcan
unmaskatype1pattern.Ajmaline(1mg/kgover5—10min),
flecainide(2mg/kg over 10min) andprocainamidecanbe
used[1,12].Therespectivesensitivitiesandspecificitiesof
thesedrugshavebeenevaluatedwithageneticgold
stan-dard,butremainamatterofdebatebecauseofthegenetic
heterogeneityof thesyndrome[13,14]. Fornow, itseems
thatflecainide and procainamide have a lowersensitivity
thanajmaline[11,15].Besides ventricular arrhythmiaand
theappearanceofatype1ECGpattern,thesodium
chan-nel blocker test is usually stopped if the QRS widens to
130% of the baseline. However, some data argue against
thiscriterion,which does notseem tobeassociated with
theoccurrenceofcomplications[16].Evenifinitial
experi-encesreportedarelativelyhighrateofcomplicationsduring
thistest,morerecentexperienceshavedemonstratedthat,
Table1 VariablesidentifiedasbeingassociatedwithsuddencardiacdeathinBrugadasyndrome.
Variables Definition EffectonSCD Mainpublications
AbortedSCD — Increasedriska [2,5,10]
Syncope Causebyarrhythmia Increasedriska [2,5,10]
SpontaneousECGpattern Type1ECG Increasedrisk [2,5,10]
Oldage Aged>60years Decreasedrisk,but
needstobeconfirmedb
[37]
Sex Femalesex Decreasesriskb [32,37]
EPS VFoccurrence Increasedrisk,with
conflictingdata,
particularlywiththree
extrastimulib
[2,10,52]
Sinusdysfunction Infemales Increasedrisk,but
needstobeconfirmedb
[33]
SwaveinD1 Swave>0.1mV
and/or>40ms
Increasedrisk,but
needstobeconfirmedb
[38]
QRSfragmentation Atleastfourspikesinoneor
atleasteightspikesinallof
theprecordialleads
Increasedrisk,but
needstobeconfirmedb
[10,40]
Inferiortype1 Type1ECGininferioror
lateralleads
Increasedrisk,but
needstobeconfirmedb
[47]
Tpeak—Tendinterval MaximumTpeak—Tend
interval>100msinprecordial
lead
Increasedrisk,but
needstobeconfirmedb
[48]
Earlyrepolarization Jwave>0.1mVintwo
inferolateralleads
Increasedrisk,with
conflictingdatab
[39,45]
Post-exerciseST-segmentelevation ≥0.05mVinV1—V3post
exercise
Increasedrisk,but
needstobeconfirmedb
[56]
Type1ECGburden 24-hHoltermonitoring Increasedrisk,but
needstobeconfirmedb
[31]
Youngage Aged<18years Conflictingdatac [34,36]
FamilyhistoryofSCD SCDinfirst-degreerelatives Conflictingdatac [2,10,39]
Genetic SCN5Amutations Conflictingdatac [2,10,34]
Atrialfibrillation — Conflictingdatac [2,9,10,38]
PRduration PR>200ms Conflictingdatac [41,44]
QRSduration QRS>120ms Conflictingdatac [41,44]
Latepotentials Twoofthreepositivecriteria Conflictingdatac [42,44]
aVrsign Rwave≥0.3mVor
R/q≥0.75inaVr
Conflictingdatac [2,10,43]
ECG:electrocardiogram;EPS:electrophysiologicalstudy;SCD:suddencardiacdeath;VF:ventricularfibrillation.
a—cAnindicationofthestrengthofdataassociatingthevariablewithSCD(fromaforconsistentandprospectivedatatocforconflicting
results).
The diagnosis of a type 1 ECG pattern is usually per-formed in V1—V3 leads at baseline or during the sodium channelblocker test. Diagnosis can alsobe performed by elevatingV1—V2leadsinthethirdandthesecondintercostal space,asthisincreasessensitivitywithoutmodifying prog-nosis[18].Basedonasingletertiary-centrestudy,thelatest
consensusreport alsoproposedacceptanceofthe
diagno-sisof BrSeveninpatientswithonlyoneleadshowingthe
typicalaspect[1,19].Manyconditionsanddiseases,
includ-ing myocardial ischaemia, acute pericarditis, pulmonary
embolism,rightventricularcompressionandmetabolic
dis-order(hyper/hypokalaemia, hypercalcaemia), can exhibit
aBrugada-like type 1ECG pattern [1,20].These BrS
phe-nocopiescannot be differentiated from true BrS because
oftheiridenticalECGpatterns,andargueforasystematic
diagnosticapproachtoavoidmisdiagnosis[21].
TruecongenitalBrS has beenshown tofollow an
auto-somal mode of inheritance in families, and mutation
identification has been suggested for diagnosis. Over 20
genes have beenassociated withBrS[13], andSCN5A has
themajorityofmutations.However,studieshaveshownthat
somepreviouslyassociatedvariantsareactuallypresentin
thegeneral population,andareprobablynon-causal [22].
Furthermore, except for the SCN5A gene, the other
BrS-associatedgenespresentasmanyrarevariantsincasesas
in controls, suggesting a minorrole for these genes [23].
Interestingly, the concept of a more complexinheritance
hasemergedfromtheobservationofincompletepenetrance
amongmutationcarriers andof phenocopiesamong
fami-lies[3],andhasbeenrecentlyillustratedbythediscovery
of frequent geneticvariants (>10% in the general
Brugadasyndrome:Diagnosis,riskstratificationandmanagement 191
[3,13,24,25]. Thus, the indication for SCN5A screening in
clinical diagnosticsmaybe restrictedtotheidentification
ofpatientsatriskinafamily[23].
Risk
stratification
Once thediagnosis of BrS has been made,the main chal-lengeistostratifytheriskofVF.Numerousvariableshave beensuggested[26,27],butotherthanprevioussymptoms
(syncopeand abortedSCD)and spontaneousECG pattern,
allremainamatterofdebate(Table1).
Main
risk
factors
Symptoms
Patients with a history of SCD have a 10% annual risk of recurrenceduringthefirst4years[2,10].Althoughthis
inci-dence subsequently decreases, it remains significant, and
laterecurrencecanbeobserved[5].Thus,ICDimplantation
isindicatedforallcardiacarrestsurvivors[1].
Amongpatientswhoarediagnosedaftersyncope,therisk
of arrhythmia has been consistently considered as
signifi-cant [2,5,6,10].Withabout 1.5%/year withVF,this riskis
fourfoldhigherthaninasymptomaticpatients[2].However,
benignvasovagalsyncopeisalsofrequentlydescribedinBrS
patients[2,6].Althoughproarrhythmiceffectsofvagal
stim-ulationhavebeendescribed,onlysyncopeprobablycaused
bynon-sustained VFhasbeenconsistentlyassociatedwith
SCD,increasingtheriskto5%/year[6,28].Thus,incaseof
syncopeofarrhythmicorigin,thereisnodoubtthatanICD
isneeded.
However,theabilitytodifferentiatearrhythmicsyncope
fromneutrallymediatedsyncoperemainsarealchallenge.
A detailed clinical history, specific triggers (pain, seeing
blood, micturition) and prodromes (palpitations, nausea,
visualdisturbance)mayhelptodistinguisharrhythmicfrom
non-arrhythmicsyncope.Unfortunately,noneofthese
varia-blesissufficienttoprovideaccurateprognosticinformation
[28].Given therelatively highrate ofcomplications after
ICDimplantation,thelatestguidelineshaverestrictedthis
implantation to‘‘patients with a spontaneoustype IECG
andhistory ofsyncope judged tobe likelycaused’’by VF
[1]. Although association witha spontaneous type 1 ECG
increasesthe risk of SCD, alarge number of patients are
diagnosedafterthesodiumchannelblockertestorwithan
uncertainclinicalhistory,andthusremaininthegreyzone
forICDimplantation[2].
Spontaneous
ECG
pattern
Identification of a spontaneouspattern of BrS on an ECG hasbeen consistentlyassociatedwithan increasedriskof SCD [2,10,29], ranging from 0.81%/year in asymptomatic
patientsto2.3%/yearinsymptomaticpatients[2].Although
therisk of appropriateICDtherapy for thosewith
asymp-tomatic BrS patients is low, it is cumulative over time,
reaching12% at10 years[5]. Regardingthe extreme
con-sequenceswithoutICDimplantation,ithasbeensuggested
that a multifactorial approach could help to stratify the
riskofSCD[5,29].However,becauseofthelimitedsizeof
populationandfollow-up,identificationofpatientswiththe
highestriskremainsachallenge.
Aspontaneoustype1ECGpatternisvariableovertime,
withmarkedday-to-dayvariabilityintheJwaveelevation
[30].Thus,long-termevaluationofthetype1ECGburden
usingHolterrecordingappears tobeanattractive toolto
stratifythe risk of arrhythmia [31]. Unfortunately,so far,
essentiallybecauseof the lack of efficienttools toeasily
assesstheSTsegmentoveralongperiod,thereisnoclear
demonstrationofthevalueofthisvariable.
Clinical
factors
Sex
AstransmissionofBrSisobservedwithanautosomalmode ofinheritance,theprevalenceofBrSisexpectedtobe sim-ilaramongmenandwomen.However,BrSclearlyhasahigh predominanceinmen,andathreefoldincreaseintherisk ofatype1ECGpatternand/orcardiacevent[32,33].
How-ever,malepredominanceisalsoobservedinasymptomatic
patients,whichleads toanon-significant association with
SCD[2,32].
AsmostriskfactorsforSCDwereassessedinpopulations
involvingalargepredominanceofmen,theyappeartobe
lessaccuratefor women.Identification of conduction
dis-turbanceandsinusdysfunctioninwomencouldbeabetter
markerofriskthanaspontaneoustype1ECGandsymptoms
[32,33].
Age
SCDduetoBrSisrareinchildren.However,theriskcanbe significant,particularlyinchildrenwithprevioussymptoms anda spontaneousECG pattern[34]. A drug-induced
pat-ternhasagoodprognosis,butperformingasodiumchannel
blockertestinchildrenisquestionablebecauseoffrequent
complicationsandfalsenegatives[35,36].
Limiteddataareavailableinolderpatients.However,the
riskofarrhythmiaappearstodecreasesignificantlyafterthe
ageof60years[37].
Family
history
and
genetics
Given the genetic background of BrS, a family history of SCDandSCN5Amutationsweresuggestedtostratifyriskof arrhythmia[34,38,39].However,largemultivariable
analy-sesdidnotconfirmthisassociationfurther[2,10].Age,the
numberofSCDsandthedegreeoftherelationshipmay
mod-ifytheeffectoffamilyhistoryonindividualrisk[34,38,39].
Atrial
arrhythmia
AtrialfibrillationismorecommoninBrS,andcanbeginearly, evenin childhood [9,34]; it has been suggested, in
case-control studies, to be associated withprognosis, but the
relationship hasnot been demonstrated in a large cohort
[2,9,10,38].
ECG
variables
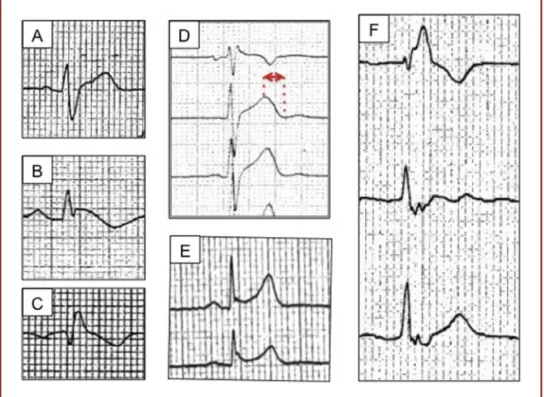
ManyECGvariableshavebeenassociatedwiththeprognosis ofBrSpatients,butwithconflictingreportsorwithout repli-cationinanindependentcohort[26,27](Fig.2,Table1).
Figure 2. The main electrocardiogram (ECG) variables associated with prognosis in Brugada syndrome. The ECGs (25mm/s with
0.1mV/mm) illustrate:A:anSwaveinD1;B:atype1ECGpatterninD2;C:aVrsign; D:aprolonged Tpeak—Tendinterval inV1—V3
leads;E:earlyrepolarizationinD2andD3;andF:fragmentedQRSinV1—V3leads.
Conduction
disturbance
ThepresenceoffragmentedQRScomplexeshasbeen con-sistentlyassociated witha twofoldtoninefoldincreasein arrhythmiaoccurrence[10,40].Ofnote,criteriadefinition
andECGrecordingfiltersettingsvariedamongstudies,
limit-ingthescopeofriskstratification,andexplainingitsabsence
fromthelatestguidelines.
Conductiondelayhasalsobeenhighlighted,intermsof
QRSduration[41],latepotential[42]andtheaVrsign[43].
However,thesevariableswerenotconfirmedinsubsequent
studies[2,10,44].
Caló et al. found that a wide or large S wave in lead
I was a predictor of VF in a multivariable analysis of
asymptomaticpatientswithaspontaneousBrSpattern[38].
Additionally,these authorsprovidedan interesting finding
regarding pathophysiology, as this S wave wasassociated
with a conduction delay in the right ventricular outflow
tract.
Repolarization
variables
InBrS,somestudiesidentifiedamoresevereprognosisinthe presenceofanearlyrepolarizationpattern[39,45],whereas
others did not find any relationship between early
repo-larizationandtherisk ofarrhythmia [46].The riskofSCD
appearstoincreasewhenearlyrepolarizationislocatedin
aninferiorleadwithahorizontalSTsegment[39].
Atype1ECGpatterninperipheralleadswasadditionally
describedinabout10%ofpatients,andwasassociatedwith
anincreasedriskofSCD[47].
Finally, a Tpeak—Tend interval >200ms, defining high
transmuraldispersionofrepolarization,hasbeenassociated
withincreasedoccurrenceofVF[48];however,thiswasnot
confirmedinadditionalstudies[49].
Electrophysiological
study
From clinical variables, the incremental prognostic value of an electrophysiological study (EPS) is highly controver-sial. Whereas some authors have proposed an association betweeninducedVFandcardiacevents,largeprospective studieshavedemonstratedthatanEPSdoesnotstratifythe riskofarrhythmia[2,10,50,51].The latestguidelineshave
restrictedtheuseofanEPStoaclassIIbforICDimplantation
[1].
Althoughmostcase-controlstudiesidentifyahighevent
rateafterapositive EPS,themainquestion iswhetherto
integratethisexaminationintotheriskstratificationofBrS.
Sroubek et al. recently reportedin a large meta-analysis
thattheinductionofventriculararrhythmiawasassociated
with a twofold to threefold increased risk of VF (hazard
ratio2.55;P=0.005)[52].However,theincrementalvalue
of an EPS appears to be small in patients with a high or
low risk of arrhythmia, as defined by clinical variables.
Considering intermediate-riskpatients, theadditional risk
ofapositiveEPSdoesnotexceeda1%/yearVFincidence.
Considering the limitations in EPS reproducibility [10],
and the fact that a negative EPS cannot exclude further
Brugadasyndrome:Diagnosis,riskstratificationandmanagement 193
Figure3. Indicationforimplantationofanimplantablecardioverterdefibrillator(ICD),accordingtotheriskofsuddencardiacdeath
(SCD).ModifiedfromRefs.[1,2].TheriskofSCDisrepresentedwitharedarrow.TheredboxesrepresentsanindicationforICDimplantation;
thegreenboxrepresentsapatientwhoshouldnotbeimplanted,accordingtothelatestguidelines;theorangeboxesarenotaddressedin
theguidelines.ECG:electrocardiogram.
appearstobe controversial,and itcannot beusedasthe onlyvariabletodefinethemanagementofthepatient.
Management
of
BrS
Eachpatientshouldfirstbereferredtoaspecializedcentre forinheritedarrhythmia.InFrance,theCardiogennetwork involvesthreereferencecentresand22competencecentres specializedinthemanagementofinheritedarrhythmia.
Forallpatients,thefirststepofmanagementisfocused oncounsellingindailylife:thisincludesavoidingexcessive alcohol intake,treating fever aggressively anddecreasing exerciseactivityprogressively.Alistoftreatmentsthatcan increase the arrhythmia risk is given to the patient (the updated list is available on brugadadrugs.org). A familial screeningshouldalwaysbeperformedtoachieveearly iden-tificationofaffectedrelativeswhocouldbeatriskofSCD
[1].
Afterthisfirststep,whichappliestoallpatients,the
dis-cussionstartsaboutwhichtherapeuticapproachtopropose
(Fig.3).Untilnow,theonlyprovenefficienttherapyisICD
implantation,but other possibilitieswill certainlyemerge
inthe nextfewyears,suchascatheterablation, whichis
restrictedtopatientswithfrequentarrhythmiarecurrences.
Asymptomaticpatientswithadrug-inducedECGpattern
present with a very low risk of arrhythmia that does not
indicateICDimplantation.Bycomparison,thereisnodoubt
abouttheindicationinsymptomaticpatientswitha
sponta-neousECGpattern.
ThemainquestionremainingrelatestoICDimplantation
inpatientswithintermediaterisk.AspontaneousECG
pat-ternin an asymptomaticpatientdefinesacumulativerisk
ofVFreaching12%at10years[5].Thisriskappearshigher
thaninsymptomaticpatients withvasovagalsyncope,and
argues for an early discussion with the patient about an
ICDimplantation[28].Inthesecases,individualassessment
ofassociatedriskfactorsshouldbeperformedtoincrease
stratificationaccuracy.However,physicianshaveto
recog-nizethat,fornow,evenifwehavearelativelyclearpicture
oftheriskatapopulationlevel,wearestillunableto
prop-erlystratifypatientriskatanindividuallevel.Thus,inour
view,it is essential toprovide the patientwith complete
informationaboutthelimitsofourknowledge.More
impor-tantly, the patient has to be involved with the decision,
asthe therapeutic choice will have a great psychological
impact,regardlessofthefinaldecision.
Observational studies have suggested that quinidine
should have a beneficial effect on arrhythmia; however,
becauseoflimiteddata,itcannotbeencouragedinprimary
prevention[53,54].Highratesofhydroquinidinesideeffects
andlownumbersofarrhythmiceventsmaypreventfurther
evidencebeingobtained,eveninhigh-riskpatients[55].The
useofquinidinemaybediscussedonacase-by-casebasisin
highlyspecializedcentres.
Conclusions
and
perspectives
Oncethe diagnosis ismade, riskstratification, and there-fore management, is often complex in BrS. Although a spontaneousECG patternandsymptomsarethetwomain predictorsofSCD,manyvariableshavebeensuggested,and theserequirefurtherevaluationinlargepopulations. Iden-tificationofintermediate-riskpatientsunderliestheneedto increasetheaccuracyofsuchstratificationandtoimprove therapywhereprevalenceofcomplicationsisastrong lim-itingfactor.Acombination ofriskfactorsin anintegrated clinicaland geneticscorecouldbe thenextsteptowards suchpersonalizedmedicine.
Thedevelopmentofnewdefibrillationtechnology,such as a subcutaneous ICD, could facilitate the decision, by reducingtherateofcomplicationsarisingfromICD implan-tation, and by making it possible to remove the system
easily in case of complication. Finally, catheter ablation, whichiscurrentlyrestrictedtohighlysymptomaticpatients, should be another means of decreasing the arrhythmic risk. Although promising, this technique still needs long-termstudies beforeindications caninclude asymptomatic patients.
Sources
of
funding
None.
Disclosure
of
interest
Theauthorsdeclarethattheyhavenocompetinginterest.
References
[1]PrioriSG,WildeAA,HorieM,etal.HRS/EHRA/APHRSexpert consensus statement on the diagnosis and management of patientswithinherited primary arrhythmiasyndromes: doc-ument endorsedbyHRS,EHRA,andAPHRS inMay2013and byACCF,AHA,PACES,andAEPCinJune2013.HeartRhythm 2013;10:1932—63.
[2]Probst V, Veltmann C, Eckardt L, et al. Long-term prog-nosis of patientsdiagnosed with Brugada syndrome: results from the FINGER Brugada Syndrome Registry. Circulation 2010;121:635—43.
[3]Probst V,WildeAA, BarcJ,et al.SCN5Amutations andthe roleofgeneticbackgroundinthepathophysiologyofBrugada syndrome.CircCardiovascGenet2009;2:552—7.
[4]GallagherMM,ForleoGB,BehrER,etal.Prevalenceand sig-nificance ofBrugada-type ECGin12,012apparentlyhealthy Europeansubjects.IntJCardiol2008;130:44—8.
[5]SacherF,ProbstV,MauryP,etal.Outcomeafterimplantationof acardioverter-defibrillatorinpatientswithBrugadasyndrome: amulticenterstudy—Part2.Circulation2013;128:1739—47.
[6]SacherF,ArsacF,WiltonSB,etal.SyncopeinBrugada syn-drome patients: prevalence, characteristics, and outcome. HeartRhythm2012;9:1272—9.
[7]Mizusawa Y, Morita H, Adler A, et al. Prognostic signif-icance of fever-induced Brugada syndrome. Heart Rhythm 2016;13:1515—20.
[8]Ohkubo K, Nakai T, Watanabe I. Alcohol-induced ventric-ular fibrillation in a case of Brugada syndrome. Europace 2013;15:1058.
[9]KusanoKF,TaniyamaM,NakamuraK,etal.Atrialfibrillationin patientswithBrugadasyndrome relationshipsofgene muta-tion, electrophysiology, andclinicalbackgrounds. JAm Coll Cardiol2008;51:1169—75.
[10]PrioriSG,GaspariniM,NapolitanoC,etal.Riskstratificationin Brugadasyndrome:resultsofthePRELUDE(PRogrammed ELec-tricalstimUlationpreDictivevaluE)registry.JAmCollCardiol 2012;59:37—45.
[11]WildeAA,AntzelevitchC,BorggrefeM,etal.Proposed diag-nostic criteriafor theBrugadasyndrome: consensusreport. Circulation2002;106:2514—9.
[12]Arnalsteen-DassonvalleE,HermidaJS,KubalaM,etal. Ajma-linechallengefor thediagnosis ofBrugadasyndrome:which protocol?ArchCardiovascDis2010;103:570—8.
[13]GourraudJB,BarcJ,TholletA,etal.TheBrugadaSyndrome: ARareArrhythmiaDisorderwithComplexInheritance. Front CardiovascMed2016;3:9.
[14]Nattel S. Are all sodium channel blockers created equal? Clinical-basic correlationsbased onobservations in Brugada syndrome.HeartRhythm2005;2:261—2.
[15]WolpertC,EchternachC,VeltmannC,etal.Intravenousdrug challengeusingflecainideandajmalineinpatientswith Bru-gadasyndrome.HeartRhythm2005;2:254—60.
[16]Batchvarov VN, Govindan M, Camm AJ, Behr ER. Signifi-cance of QRS prolongation during diagnostic ajmaline test inpatientswithsuspectedBrugadasyndrome.HeartRhythm 2009;6:625—31.
[17]VeltmannC,WolpertC,SacherF,etal.Responsetointravenous ajmaline:aretrospectiveanalysisof677ajmalinechallenges. Europace2009;11:1345—52.
[18]MiyamotoK,YokokawaM,TanakaK,etal.Diagnosticand prog-nosticvalueofatype1Brugadaelectrocardiogramathigher (thirdorsecond)V1toV2recordinginmenwithBrugada syn-drome.AmJCardiol2007;99:53—7.
[19]SarkozyA,SorgenteA,BoussyT,etal.Thevalueofafamily his-toryofsuddendeathinpatientswithdiagnostictypeIBrugada ECGpattern.EurHeartJ2011;32:2153—60.
[20]ShimizuW.AcquiredformsoftheBrugadasyndrome.J Elec-trocardiol2005;38:22—5.
[21]Gottschalk BH, Anselm DD, Brugada J, et al. Expert car-diologists cannot distinguish between Brugada phenocopy andBrugadasyndromeelectrocardiogrampatterns.Europace 2016;18:1095—100.
[22]BehrER,Savio-GalimbertiE,BarcJ,etal.Roleofcommonand rarevariantsinSCN10A:resultsfromtheBrugadasyndrome QRSlocusgenediscoverycollaborativestudy.CardiovascRes 2015;106:520—9.
[23]LeScouarnecS,Karakachoff M,Gourraud JB,et al.Testing theburdenofrarevariationinarrhythmia-susceptibilitygenes providesnewinsightsintomoleculardiagnosisforBrugada syn-drome.HumMolGenet2015;24:2757—63.
[24]BezzinaCR, BarcJ, Mizusawa Y,et al. Common variantsat SCN5A-SCN10A and HEY2 are associated with Brugada syn-drome,ararediseasewithhighriskofsuddencardiacdeath. NatGenet2013;45:1044—9.
[25]HermidaJS,Arnalsteen-DassonvalleE,KubalaM,etal.Dual phenotypictransmissioninBrugadasyndrome.ArchCardiovasc Dis2013;106:366—72.
[26]AdlerA,RossoR,ChorinE,HavakukO,AntzelevitchC,Viskin S.RiskstratificationinBrugadasyndrome:Clinical character-istics,electrocardiographicparameters,andauxiliarytesting. HeartRhythm2016;13:299—310.
[27]ProbstV,ChatelS,GourraudJB,MarecHL.Riskstratification andtherapeuticapproachinBrugadasyndrome.Arrhythm Elec-trophysiolRev2012;1:17—21.
[28]OldeNordkampLR,VinkAS,WildeAA,etal.SyncopeinBrugada syndrome: prevalence, clinical significance,and clues from history takingto distinguish arrhythmicfrom nonarrhythmic causes.HeartRhythm2015;12:367—75.
[29]Delise P, Allocca G, Marras E, et al. Risk stratification in individuals with the Brugada type 1 ECG pattern without previous cardiac arrest: usefulness of a combined clini-cal and electrophysiologic approach. Eur Heart J 2011;32: 169—76.
[30]Richter S, Sarkozy A, Veltmann C, et al. Variability of the diagnostic ECG pattern in an ICD patient population withBrugadasyndrome.JCardiovascElectrophysiol2009;20: 69—75.
[31]ExtramianaF,Maison-BlancheP,BadiliniF,MessaliA,DenjoyI, LeenhardtA.Type1electrocardiographicburdenisincreased insymptomaticpatientswithBrugadasyndrome.J Electrocar-diol2010;43:408—14.
[32]BenitoB,SarkozyA,MontL,etal.Genderdifferencesin clin-icalmanifestations ofBrugada syndrome.JAm CollCardiol 2008;52:1567—73.
Brugadasyndrome:Diagnosis,riskstratificationandmanagement 195
[33] SieiraJ,ConteG,CiconteG,etal.Clinicalcharacterisationand long-termprognosisofwomenwithBrugadasyndrome.Heart 2016;102:452—8.
[34] AndorinA, Behr ER,Denjoy I,et al. Impactof clinicaland geneticfindingsonthemanagement ofyoung patientswith Brugadasyndrome.HeartRhythm2016;13:1274—82.
[35] Conte G, de Asmundis C,CiconteG, et al. Follow-upfrom childhood to adulthood of individuals with family history ofBrugada syndrome and normal electrocardiograms.JAMA 2014;312:2039—41.
[36] Conte G, Dewals W, Sieira J, et al. Drug-induced Bru-gada syndrome in children: clinical features, device-based management, and long-term follow-up. J Am Coll Cardiol 2014;63:2272—9.
[37] Conte G, DEA C, Sieira J, et al. Clinical characteristics, management,andprognosisofelderlypatientswithBrugada syndrome.JCardiovascElectrophysiol2014;25:514—9.
[38] CaloL, Giustetto C,Martino A, et al. Anew electrocardio-graphic marker of suddendeath in brugada syndrome: the S-waveinleadI.JAmCollCardiol2016;67:1427—40.
[39] KamakuraS,OheT,NakazawaK,etal.Long-termprognosisof probandswithBrugada-patternST-elevationinleadsV1—V3. CircArrhythmElectrophysiol2009;2:495—503.
[40] MoritaH, Kusano KF, Miura D, et al. Fragmented QRS as a markerofconductionabnormalityandapredictorofprognosis ofBrugadasyndrome.Circulation2008;118:1697—704.
[41] TokiokaK, KusanoKF, Morita H, et al. Electrocardiographic parameters and fatal arrhythmic events in patients with Brugadasyndrome:combination ofdepolarizationand repo-larizationabnormalities.JAmCollCardiol2014;63:2131—8.
[42] TakagiA,NakazawaK,SakuraiT,NankeT,MiyakeF. Prolonga-tionofLAS40(durationofthelowamplitudeelectricpotential component(<40microV)oftheterminalportionoftheQRS) inducedbyisoproterenolin11patientswithBrugadasyndrome. CircJ2002;66:1101—4.
[43] BabaiBigiMA,AslaniA,ShahrzadS.aVRsignasariskfactor forlife-threateningarrhythmiceventsinpatientswithBrugada syndrome.HeartRhythm2007;4:1009—12.
[44] MauryP,RollinA, SacherF,et al.Prevalenceandprognostic roleofvariousconductiondisturbancesinpatientswiththe Brugadasyndrome.AmJCardiol2013;112:1384—9.
[45] Sarkozy A, Chierchia GB, Paparella G, et al. Inferior and lateral electrocardiographic repolarization abnormalities in
Brugada syndrome. Circ Arrhythm Electrophysiol 2009;2: 154—61.
[46]LetsasKP,SacherF,ProbstV,etal.Prevalenceofearly repolar-izationpatternininferolateralleadsinpatientswithBrugada syndrome.HeartRhythm2008;5:1685—9.
[47]RollinA,SacherF,GourraudJB,etal.Prevalence, characteris-tics,andprognosisroleoftype1STelevationintheperipheral ECGleadsinpatientswithBrugadasyndrome.HeartRhythm 2013;10:1012—8.
[48]MauryP,SacherF,GourraudJB,etal.IncreasedTpeak-Tend interval is highly and independently related to arrhyth-mic events in Brugada syndrome. Heart Rhythm 2015;12: 2469—76.
[49]JunttilaMJ,BrugadaP,HongK,etal.Differencesin12-lead electrocardiogram between symptomatic and asymptomatic Brugada syndrome patients. J Cardiovasc Electrophysiol 2008;19:380—3.
[50]BrugadaP,BrugadaR,MontL,RiveroM,GeelenP,BrugadaJ. NaturalhistoryofBrugadasyndrome:theprognosticvalueof programmedelectricalstimulationoftheheart.JCardiovasc Electrophysiol2003;14:455—7.
[51]FauchierL,IsorniMA,ClementyN,PierreB,SimeonE,Babuty D. Prognostic value of programmed ventricular stimulation in Brugada syndrome accordingto clinicalpresentation: an updatedmeta-analysisofworldwidepublisheddata.IntJ Car-diol2013;168:3027—9.
[52]SroubekJ,ProbstV,MazzantiA,etal.Programmedventricular stimulationforriskstratificationintheBrugadasyndrome:a pooledanalysis.Circulation2016;133:622—30.
[53]BouzemanA,TraulleS,MessaliA,etal.Long-termfollow-up of asymptomatic Brugada patients with inducible ventric-ular fibrillation under hydroquinidine. Europace 2014;16: 572—7.
[54]ProbstV,GourraudJB.QuinidineinBrugadasyndrome:stilla longwaytogo.CircArrhythmElectrophysiol2015;8:1309—10.
[55]AndorinA,FouchardS,LeMarecH,etal.QUIDAMStudy: assess-mentofhydroquinidinetherapyinthemanagementofBrugada syndromepatientsathigharrhythmicriskandimplantedwith anICD.ACVDSuppl2016;8:225—6[abstract0332].
[56]Makimoto H, Nakagawa E, Takaki H, et al. Augmented ST-segment elevation during recovery from exercise predicts cardiaceventsinpatientswithBrugadasyndrome.JAmColl Cardiol2010;56:1576—84.